GENERAL NEUROLOGY
Disorders of consciousness
Updated on 11/07/2024, published on 21/11/2023
Definition of consciousness
- consciousness is a state wherein an individual is awake, fully and correctly aware of themselves and their environment, capable of receiving and processing stimuli, acting according to their will, and responding adequately to both internal and external stimuli
- 3 components of consciousness are assessed:
- arousal (vigilance, wakefulness) – related to brainstem
- awareness – related to the cortico-thalamic network
- attention
- deviations from the normal state of consciousness are referred to as disorders of consciousness
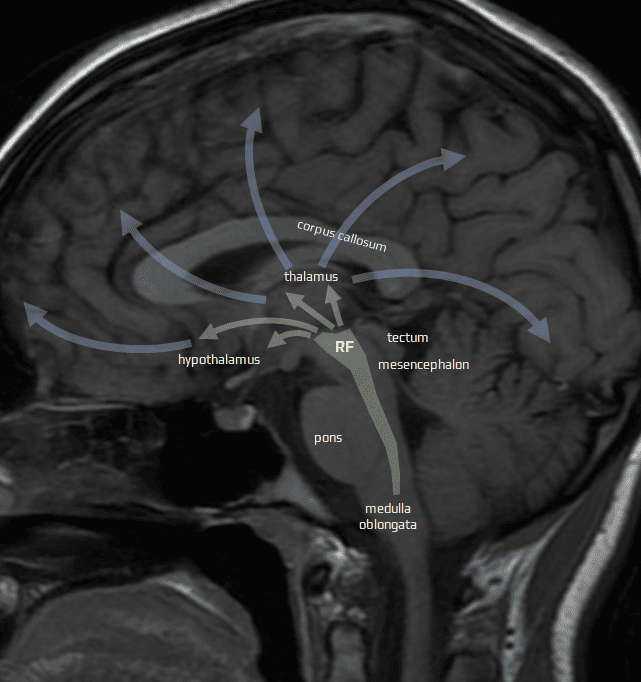
Anatomical substrate of consciousness
- the anatomical substrate of consciousness is complex and not fully understood
- consciousness probably arises from integrated neural processes across multiple brain regions; key structures include:
- cerebral cortex – particularly the prefrontal cortex, which is crucial for executive functions and awareness
- thalamus – a relay station for sensory and motor signals to the cortex, playing a significant role in consciousness and alertness
- ascending reticular activating system (ARAS) – located in the brainstem; it regulates wakefulness and sleep-wake cycle
- the main component of ARAS is the brainstem reticular formation (RF)
- RF is a network of neurons controlling autonomic functions, regulating consciousness, motor control, and modulation of sensory information
Classification of disorders of consciousness
Qualitative consciousness disorders
Quantitative consciousness disorders
Qualitative and quantitative consciousness disorders may coexist
Clinical evaluation
- the patient’s survival is the priority, so initial therapy is aimed at preserving or restoring vital functions
- secure airway with OTI (usually followed by mechanical ventilation), establish venous access, insert a urinary catheter, etc.
- if trauma is suspected, stabilize the C-spine until imaging rules out the traumatic lesion
- standard neurologic examination is not helpful in comatose patients; a specific set of tests must be used to:
- evaluate the level of consciousness
- determine the location/extent of the lesion (structural or functional)
- evaluate the cause (probable structural lesion v.s. diffuse metabolic disorder or intoxication)
- repeated examinations help to assess the progression or regression of the lesion (course of rostrocaudal deterioration syndrome)
- evaluate the level of consciousness
General examination
Airway and breathing
- if signs of respiratory insufficiency are observed, check airways and decide whether intubation and mechanical ventilation are required; search for extracerebral causes (pulmonary or cardiac)
- the initial assessment includes an arterial blood acid-base balance (ABR) test; adequate measures should be taken in the case of hypoxemia (Pa02 < 9 kPa) or hypercapnia (PaC02 > 6.5 kPa)
- in unconscious patients, intubation should not be delayed to reduce the risk of aspiration and ensure effective ventilation and safe transportation for further investigations (CT, MRI, etc.)
- a patient who is intubated, ventilated, relaxed, and sedated cannot be thoroughly neurologically examined; therefore, it is rational to perform a rapid baseline neurological examination before sedation starts
Blood pressure
- hypotension poses a greater risk than hypertension and should be addressed immediately
- when systolic blood pressure (SBP) falls to < 60 mmHg, cerebral blood flow autoregulation is lost; the critical value is higher in patients with chronic hypertension
- rapid administration of volume expanders and sympathomimetics is the basic measure for hypotension
- decompensated hypertension may be
- reflex reaction to intracranial hypertension (Cushing’s reflex with concomitant bradycardia)
- stress reaction (usually with tachycardia)
- cause of altered consciousness (via hypertensive encephalopathy, IC bleeding)
- reflex reaction to intracranial hypertension (Cushing’s reflex with concomitant bradycardia)
Basic cardiac evaluation
- initial ECG should followed by continuous ECG monitoring
- severe arrhythmia may be the cause of coma or indicate its etiology (embolic stroke in AFib) and require immediate treatment
- bradycardia is associated with intracranial hypertension, cardiac conduction blocks, or with certain toxins and drugs (beta-blockers)
- tachycardia is present in hypovolemia, hyperthyroidism, fever, anemia, and as an effect of certain toxins and drugs (cocaine, anticholinergics)
Once the vital functions are intact or stabilized, the patient can undergo more detailed examination
Body temperature
- hyperthermia
- may indicate neuroinfection
- central hyperthermia is less frequent and typically occurs in subarachnoid hemorrhage or hypothalamic lesions
- hyperthermia may also be present in thyrotoxic crisis, malignant hyperthermia, neuroleptic malignant syndrome, and intoxication with certain drugs (atropine and other anticholinergics)
- hypothermia
- profound hypothermia may itself cause altered consciousness
- it may result from external hypothermia, metabolic disorder, or barbiturate intoxication, rarely due to lesions of the posterior hypothalamus
- profound hypothermia may itself cause altered consciousness
Physical appearance
- cachexia suggests a chronic disease, most often a malignancy
- an obese patient is often treated for diabetes or hypertension
- specific appearance indicates endocrinopathies (cushingoid habitus) or chronic alcoholism
Skin changes
- needle punctures (intravenous drug injection)
- eyelid edema (renal failure)
- pale skin (significant anemia)
- increased pigmentation (porphyria, Addison’s disease, disseminated melanoma)
- generalized cyanosis (hypoxia, CO2 intoxication)
- cherry red coloration (CO intoxication)
- grey-blue coloration (methemoglobin intoxication)
- localized cyanosis is indicative of multiple arterial emboli or vasculitis
- icterus (hepatic dysfunction or hemolytic anemia)
- petechiae (DIC, thrombocytopenic purpura, drug AEs, meningococcal sepsis)
- Kaposi’s sarcoma, anogenital herpetic lesions, or oral candidiasis may indicate AIDS syndrome
- spider nevi, loss of pubic and axillary hair, and gynecomastia are manifestations of liver cirrhosis
Examination of the oral cavity
- an injured tongue is an indicator of a probable epileptic seizure
- gum hypertrophy suggests hydantoin therapy
- alcohol intoxication, diabetic ketoacidosis (acetone), uremia (fishy odor), and hepatic encephalopathy (putrid odor) are identifiable by distinct smells
Chest, abdomen, extremities
- abdominal examination: hepatomegaly, splenomegaly, abdominal resistance, ascites, défense musculaire and urinary retention
- check lower extremities for phlebothrombosis (risk of pulmonary embolism) and edema (indicative of heart failure)
- breast examination in women, testicular examination in men
- per rectum examination
- generalized lymphadenopathy may signal malignancy, infection (including AIDS), inflammatory connective tissue disease, sarcoidosis, or other systemic diseases
- heart murmur may indicate congenital or rheumatic heart defects, myxoma, or bacterial endocarditis
- conjunctival congestion is common in malignant arterial hypertension or congestive heart failure
- other symptoms
- vomiting (intracranial hypertension, intoxication, or metabolic disorders)
- bed-wetting, tongue biting may result from an epileptic seizure
- signs of trauma – periocular hematoma (raccoon eyes) in skull base fractures, mastoid process hematoma (battle sign) in pyramid fractures, CSF leak, or bleeding from the nose, mouth or ear
- look for evidence of previous surgery
Meningeal signs
- neuroinfection, subarachnoid hemorrhage, carcinomatous meningitis, increased intracranial pressure, or tonsillar herniation
→ Meningeal syndrome
Others
- conjunctival congestion is often observed in malignant arterial hypertension or congestive heart failure
- vomiting may indicate intracranial hypertension, intoxication, or metabolic disorder
- bed-wetting, tongue biting may be consequent to an epileptic seizure
- signs of trauma – periocular hematoma (raccoon eyes) in skull base fractures, the mastoid process hematoma (battle sign) in pyramid fractures, cerebrospinal fluid (CSF) leakage, bleeding from the nose, mouth or ear
- look for signs of past surgery
Neurologic examination
|
Beneš-Drábek classification of unconsciousness
|
|
|
I. Response to verbal stimulus
|
|
|
1st degree (normal)
|
full consciousness, swift answers
|
|
2nd degree (somnolence I)
|
answers slowly, often inappropriately
|
|
3rd degree (somnolence II)
|
complies with several simple commands
|
|
4th degree (somnolence III)
|
complies with a single simple command
|
|
5th degree (somnolence IV)
|
verbal stimulus elicits an awakening and orienting response; the patient opens their eyes and may produce an unintelligible sound
|
|
II. Response to painful stimulus
|
|
|
6th degree (sopor)
|
purposeful defensive movements of the upper extremities or escape reactions of limbs or the entire body, facial reactions
|
|
7th degree (semicoma)
|
nociceptive stimulus elicits non-purposeful flexion/extension of the limbs
|
|
8th degree (coma)
|
decorticate/decerebrate rigidity
|
|
9th degree (deep coma)
|
changes in breathing and heart rate, no motor response
|
|
10th degree (deep coma)
|
no response to any stimuli
|
| Ramsay score |
|
| Clinical Score | Patient Characteristics |
| 1 | Awake; agitated or restless or both |
| 2 | Awake; cooperative, oriented, and tranquil |
| 3 | Awake but responds to commands only |
| 4 | Asleep; brisk response to a light glabellar tap or loud auditory stimulus |
| 5 | Asleep; sluggish response to light glabellar tap or loud auditory stimulus |
| 6 | Asleep; no response to glabellar tap or loud auditory stimulus |
One of the most commonly used measures of sedation, which divides a patient’s level of sedation into six categories ranging from severe agitation to deep coma
Oculomotor function depends on the integrity of the hemispheres, cerebellum, and brainstem. Voluntary eye movements cannot be assessed in comatose patients. However, assessment of the eye slits, eyelid muscles tonus, pupils and their reactions, eye position, and their spontaneous and reflex movements are valuable
Eye slits, eyelid muscle tone
- spontaneously opened eyes are usually a sign of preserved arousal
- in a coma, the eyelids tend to be clenched due to tonic contraction of the eye muscles; in a deep coma with muscle hypotonia, the eyes may be open (DDx of facial diplegia)
- in pontine lesions, tonic contraction of the eyelid elevators with their retraction may be present
- with the eyes closed, we test whether the patient will open them in response to verbal or painful stimulus
- blinking or opening the eyes in response to verbal stimulation is a favorable sign
- always test muscle tone by passively lifting the upper eyelid
Extraocular motility and ocular alignment
- aligned central position of the eyeballs or slight divergence up to 15-20 degrees is the most common presentation
- such findings suggest intact oculomotor innervation or a symmetrical disorder
- unilateral or asymmetric lesion leads to dislocations of the eyeballs
- eyes may be turned inward (esotropia), outward (exotropia), upward (hypertropia), or downward (hypotropia)
- a peripheral lesion (affecting the nucleus or nerve) has a typical presentation, such as eye deviation temporally (CN III lesions) or nasally (CN VI lesions)
- supranuclear disorders cause conjugate and disconjugate deviations
- horizontal conjugate deviation
- cortical lesion involving the frontal eye fields – conjugate deviation towards the lesion (“looking at ischemia”); during a seizure, eyes are deviated contralaterally (due to irritation)
- brainstem lesion (paramedian pontine reticular formation) – conjugate deviation away from the lesion
- vertical conjugate deviation
- downward – lesions in the rostral interstitial nucleus of the medial longitudinal fasciculus (riFLM) or posterior commissure
- upwards – lesions in the cerebellum and upper brainstem
- downward – lesions in the rostral interstitial nucleus of the medial longitudinal fasciculus (riFLM) or posterior commissure
- Botinelli-Fisher syndrome (thalamic hemorrhage syndrome) – downward deviation of the eyeballs, convergence spasm, upward gaze paresis, bilateral miosis, bilateral plegia, and hemianesthesia
- skew deviation (Hertwig-Magendie syndrome) – one eye is deviated upward and outward (externally), while the other is deviated downward and inward (internally)
- mesencephalic lesion on the side of the eye deviated superiorly
- cerebral lesion on the side of the eye deviated downward
- horizontal conjugate deviation
Spontaneous eye movements
- to test voluntary eye movements, passively open the patient’s eyes and observe for any purposeful movements (fixation)
- spontaneous involuntary eye movements are a pathological sign
- these movements are typically conjugate and symmetric and can be divided into several types
- horizontal movements
- roving – slow, spontaneous, conjugate movements with an amplitude of up to 90 degrees, mostly horizontal. They are typical for disorders at the corticosubcortical level, and their presence excludes severe brainstem lesion
- ping-pong – fast, alternating lateral eye movements (observed in diffuse axonal injury, hypoxic-ischemic encephalopathy, and drug or toxin exposure)
- vertical movements
- bobbing – rapid, bilateral, downward jerk with a slow return to mid-position, suggestive of a pontine lesion
- dipping (inverse bobbing) – slow downward eye movement followed by a delayed quick return upward to mid-position; suggestive of the pontine lesion, but also observed in cerebellar hemorrhage, obstructive hydrocephalus, and metabolic encephalopathy
- reverse bobbing – a quick upward eye movement followed by a slow downward return to mid-position; commonly seen with metabolic encephalopathy
- bobbing – rapid, bilateral, downward jerk with a slow return to mid-position, suggestive of a pontine lesion
- horizontal movements
Reflex eye movements
- conjugate eye movements induced by stimulation of the vestibular system in patients with impaired consciousness
- caloric reflex
- oculocephalic reflex (Doll’s eye maneuvers)
Pupills
- normal pupils are round, regular, and equal in size (isocoric)
- mean pupil size is 2.5-8 mm (depending on light conditions)
- mydriatic pupils: 4.5-9 mm
- miotic pupils: 1-2 mm
Fundoscopic exam
- performed on non-dilated pupils so that the pupils can be appropriately monitored during a coma
- papilledema indicates high intracranial pressure, possibly due to intracranial mass or hemorrhage
- intraocular hemorrhage suggests Terson syndrome (a finding in which acutely raised intracranial pressure from subarachnoid hemorrhage or traumatic brain injury causes vitreous, subhyaloid, intraretinal, or subretinal bleeding)
- assessing motor function is valuable in determining the lesion´s extent and the patient’s level of unconsciousness
- evaluate the character and extent of spontaneous movements (if targeted, their extent and symmetry) or test the motor response to painful stimuli
- in all stages of somnolence, tone, and postural reactivity are normal, with spontaneous movements present
- sopor, semicoma, and coma can be differentiated by examining the muscle tone and motor response to pain
- in a coma, decorticate and decerebrate posturing (rigidity) is observed as a result of disconnection of the brainstem from inhibitory cortical and subcortical influence
- deep coma is characterized by hypotonia and postural nonreactivity
- decorticate rigidity
- exhibits predominant flexor activity in the upper limbs and persistent extensor activity in the lower limbs
- indicative of hemispheric dysfunction (lesion at corticosubcortical or diencephalic level)
- mortality rate ~ 50-55%
- decerebrate rigidity
- extensor posturing, trismus, and possibly opisthotonus
- patients are rigid, with extension and internal rotation of the arms and legs, flexion of the wrists, and plantar flexion of the feet
- mixed decerebrate rigidity (reverse decerebrate syndrome)
- characterized by extensor posture in the upper limbs and a flaccid or flexed posture in one or both lower limbs, abducted at the hip
- results from lesions in the pontine tegmentum, particularly affecting the vestibular nuclei and vestibulospinal pathways that facilitate ipsilateral extensor motoneurons
- occurs most commonly in primary pontine lesions
- prognosis is fatal (mortality 100%)
- generalized atony (flaccidity)
- atony with postural areactivity is caused by suppression of central motor mechanisms in the ponto-bulbar reticular formation
- spinal cord lesion must be excluded
- prognosis is generally fatal (mortality 100%)
| Motor response | Lesion location |
Mortality |
| decorticate rigidity | diencephalon or cortico-subcortical |
50% |
| decerebrate rigidity | diencephalon-upper brainstem | 85% |
| mixed decerebrate rigidity | pons | 100% |
| generalized atony | pons-medulla |
100% |
Respiration serves two primary functions:
- metabolic (automatic) for maintaining oxygenation and acid-base balance
- regulated by ponto-bulbar respiratory centers via the reticulospinal tracts
- voluntary (behavioral) – involved in speech and emotional-affective responses
- controlled by suprapontine regulatory systems
- controlled by suprapontine regulatory systems
- both systems cooperate and integrate in the reticular formation of the lower brainstem and, to some extent, at the spinal cord level
Central respiratory disorders refer to conditions that impair the brain’s ability to regulate breathing:
- functional or structural lesions in the circuits controlling voluntary and metabolic respiration
- adverse biochemical effect on the respiratory brainstem centers (toxins, drugs, etc.)
The topographic value of respiratory dysfunctions in comatose patients is reduced by concomitant metabolic disorders, mechanical ventilation, and other factors
For practical reasons, respiratory disorders can be divided into three groups:
- Cheyne-Stokes breathing
- breathing with gradually increasing and decreasing depth of breaths, followed by apnea
- the pattern repeats in both short and long cycles
- accelerated (tachypneic) breathing
- hypoxic hypocapnic hyperventilation
- primary central neurogenic hyperventilation
- characterized by accelerated and deepened breathing with a frequency >25 breaths per minute
- occurs with functional or structural lesions of the paramedian reticular formation of the lower half of the midbrain and the upper two-thirds of the pons
- rare (hypoxic hypocapnic hyperventilation is more prevalent)
- irregular breathing covers various patterns such as:
- apneustic breathing and variants
- characterized by individual deep breaths followed by a two to three-second pause
- cluster breathing is characterized by groups of equally deep breaths followed by a variably long apneic pause
- cogwheel-type breathing
- alternating breathing (alternation of small and large breaths)
- ataxic (Biot’s) breathing
- characterized by completely chaotic breathing with irregular deep and shallow breaths, followed by irregular pauses; the frequency of breaths usually decreases, often progressing to apnea
- results from a disorder of the inspiratory and expiratory centers in the reticular formation of the medulla oblongata
- gasping
- individual deep gasping breaths, followed by an apneic pause of variable duration
- it is an agonal type of breathing that precedes respiratory arrest
- apneustic breathing and variants
| Type of breathing | Definition | Lesion localization |
| Cheyne-Stokes respiration | alternating hyperpnea and apnea | diffuse hemispheric involvement or diencephalic lesion |
| central hyperventilation | hyperventilation with hypocapnia, elevated pO2 and pH | lower mesencephalon and upper 2/3 of the pons |
| hypoxic hypocapnic hyperventilation | hyperventilation with hypocapnia and hypoxia | peripheral (pulmonary) causes |
| apneustic breathing | short-lived respiratory spasm at full inhalation or brief pauses during inhalation | mid-caudal pons |
| ataxic breathing | irregular alternation of shallow and deep breathing with irregular pauses | dorsomedial oblongata |
| gasping | individual deep gasping breaths, followed by an apneic pause | oblongata |
Diagnostic methods
Brain CT/MRI
- essential for detecting or excluding intracranial lesions
- MRI surpasses CT in sensitivity for imaging brain pathologies
- the presence of metabolic disorders does not preclude the existence of concurrent structural lesions
Blood tests
- blood sampling is less extensive in structural lesions compared to supposed metabolic or toxic disorders
- metabolic disorders should be carefully corrected, including hypoglycemia, hypoxia, hypothermia/hyperthermia, hypercapnia, alkalosis/acidosis, as well as electrolytes and osmolality disturbances
Lumbar puncture
- infection
- SAH
- carcinomatous meningitis
ECG
- detects arrhythmias and coronary ischemia
- may reveal nonspecific changes in electrolyte imbalance or thyroid dysfunction
EEG
- essential to rule out non-convulsive status epilepticus
- helps in evaluating the severity of toxic-metabolic encephalopathy
- prognostic value
Evoked potentials
- somatosensory evoked responses (SEPs) and brainstem auditory evoked potentials (BAEPs) test specific pathways and cortical areas
- EPs are less influenced by sedation than EEG, making them useful for monitoring and establishing prognosis in relaxed, sedated, and comatose patients (e.g., after trauma or anoxia)