NEUROIMAGING
Neurosonology
Updated on 12/12/2023, published on 24/11/2021
Definition and capabilities of neurosonology
- neurosonology refers to the use of ultrasonography to evaluate the cerebral circulation and nervous system (such as peripheral nerves and brain structures)
- it enables noninvasive assessment of blood flow in intracranial and extracranial vessels and is an essential component of diagnosing and monitoring cerebrovascular diseases
- neurosonology includes:
- the combination of both methods allows for a comprehensive, noninvasive diagnosis of cerebrovascular disease:
- detection of occlusions, stenoses, and vasospasms
- including the evaluation of the impact of extracranial stenoses/occlusions on intracranial circulation (reduction of velocities and indices)
- assessment of collateral circulation
- assessment of cerebral vasomotor reactivity (CVR or CVMR)
- detection of AV malformations
- assessment of the feeding arteries (“feeders” are characterized by increased flow velocities and decreased pulsatility index and resistance index
- assessment of the feeding arteries (“feeders” are characterized by increased flow velocities and decreased pulsatility index and resistance index
- monitoring of recanalization in acute stroke (→ TIBI)
- periprocedural monitoring during CAS or CEA
- periprocedural detection of embolizations (HITS)
- indication for shunt placement during CEA (when Vmean drops to < 30 cm/s or 50% of baseline values after artery occlusion)
- detection of R-L shunts (bubble test) and spontaneous microembolizations
- diagnosis of cerebral circulatory arrest (brain death) → see here
- therapeutic applications – sonothrombolysis, sonolysis (currently considered experimental methods)
- diagnosis of intracranial hypertension
- detection of occlusions, stenoses, and vasospasms
Indications for neurosonology
- patients with stroke symptoms in the carotid or vertebrobasilar (posterior) circulation, including amaurosis fugax
- monitoring of recanalization therapy (→ TIBI)
- patients with chronic cerebrovascular disease, especially those with previously documented extra- and/or intracranial artery disease, assessment of collateral circulation and vasomotor reactivity
- patients with a focal neurological deficit of unknown origin in whom a possible vascular etiology is considered
- patients with trauma to the cervical spine or with local pathological findings in the neck that may be related to the vascular system
- patients with a pathological physical examination (cervical murmurs, blood pressure asymmetry on upper extremities, etc.)
- follow-up of patients after CEA/CAS
- patients scheduled for major surgery, especially cardiac and vascular surgery involving extracorporeal circulation (ECC)
- patients with cardiovascular disease and multiple vascular risk factors
- patients with vascular malformations, especially AV shunts (detection of feeding vessels, post-procedure monitoring) → DAVF
- differential diagnosis of headaches, especially migraine
- detection of the right-to-left shunt (RLS) in suspected paradoxical embolism (PFO, pulmonary AV shunts)
B-mode
- B-mode is a two-dimensional ultrasound image composed of bright dots representing the ultrasound echoes
- time (echo distance) and amplitude (echogenicity) of the returned echo signal are processed
- B-mode allows the visualization and assessment of anatomical structures in the insonated area
- the vascular wall is displayed as a double line with a hypoechoic center
- an important parameter is the ultrasound resolution
- lateral resolution is worse than axial resolution and depends on the size and shape of the probe
- lateral resolution deteriorates with increasing distance from the probe (unlike axial resolution)
Color Doppler Imaging (CDI) / Color Flow Mode (CFM)
- CDI/CFM allows the visualization of flow direction and velocity within the operator-defined color box
- Doppler shifts of the returning ultrasound waves within the color box are color-coded based on average velocity and direction
- flow is typically depicted as red when moving toward the probe and blue when moving away from the probe (specific user settings)
- shades of each color denote different velocities (lighter shade = higher velocity)
- the color is superimposed over the B-mode image, facilitating the identification of the vessel course and examination of the flow channel
- under physiological conditions, aliasing does not occur in arteries (unless the Nyquist limit is reached)
- aliasing (visible in color Doppler, not power Doppler!) appears as red to blue hues (may mimic flow in the opposite direction), not separated by a black region of no flow. The artifact disappears if the velocity scale is increased above the peak flow velocity
- aliasing helps to detect areas of increased flow, such as stenosis or AV fistula
- aliasing (visible in color Doppler, not power Doppler!) appears as red to blue hues (may mimic flow in the opposite direction), not separated by a black region of no flow. The artifact disappears if the velocity scale is increased above the peak flow velocity
- advantages:
- shows flow velocity for both small and large vessels at different depths
- shows flow information at greater depths
- improves separation of adjacent arteries and veins
Power Doppler Imaging (PDI)
- PDI encodes the energy (power) of moving particles
- with the optimal gain setting, the lumen of the artery is homogeneously filled with color
- independent of insonation angle, with no signal aliasing, more sensitive to slow flow
- PDI provides no directional information, has a lower frame rate, and may exhibit artifacts from surrounding slow-moving tissue
- in newer machines, directional information is shown on Directional PDI Maps
B-flow mode
- B-flow is a unique flow mode (on GE systems) that directly images blood reflectors and tissue simultaneously, providing an accurate morphologic representation of intraluminal blood flow throughout the entire field of view
- compared to other flow modes, B-Flow offers several advantages:
- it displays the true vessel diameter
- it has high spatial resolution to show fine vessel details (including plaque morphology) and flow in larger vessels
- it is angle-independent
- B-flow may be helpful to
Pulse wave Doppler
- spectral Doppler permits the graphical display of velocities over time
- pulsed Doppler enables the recording of Doppler shifts in a user-defined area (sample volume/gate)
- these curves provide information about absolute velocities and the direction of flow
- Doppler signals are also converted to audio signals, which enable the investigator to “hear” the blood flow during the examination
- higher velocities = high-pitched sounds
- lower velocities= low-pitched sounds
- during the examination, assess the following parameters:
- under physiological conditions, the flow is laminar, continuous, without turbulence and low-frequency murmurs
- measure flow in multiple segments (see below)
- angle correction is necessary – the angle between the direction of blood flow in the artery and the ultrasound beam should be ≤ 60 degrees (usually 50-60°)
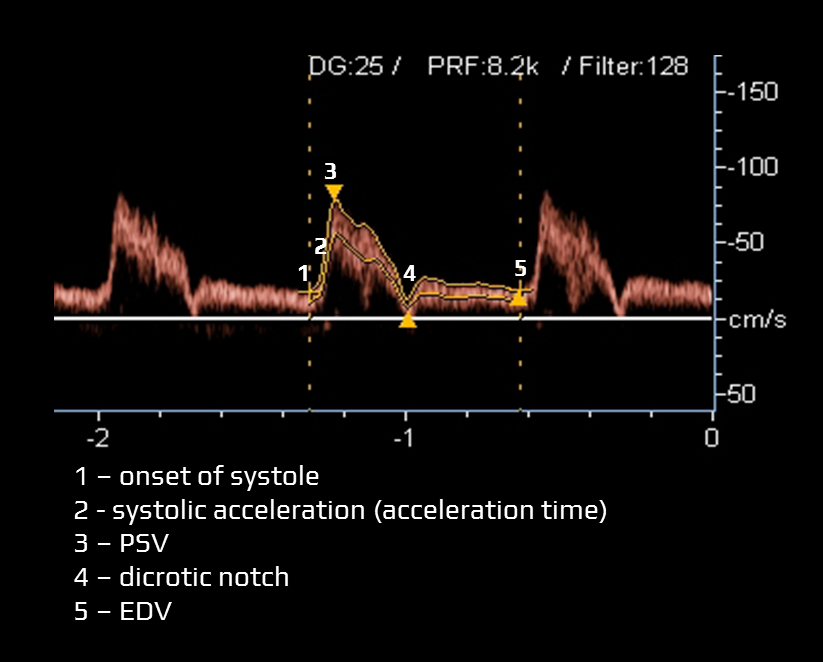
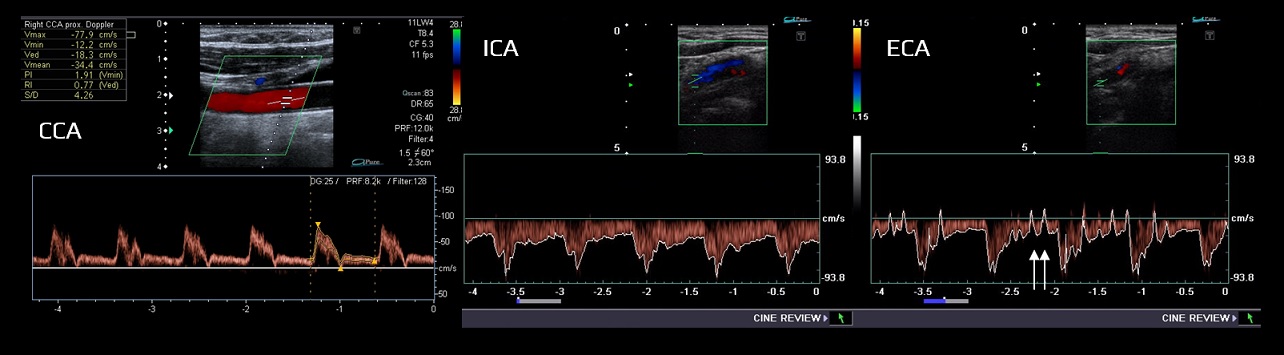
Doppler waveform
- several factors influence the character of the flow:
- heart ejection fraction (EF)
- flow volume and pressure
- resistance and geometry of the vascular system
- vessel wall elasticity
- blood viscosity
- the Doppler waveform refers to the morphology of pulsatile blood flow on spectral Doppler ultrasound
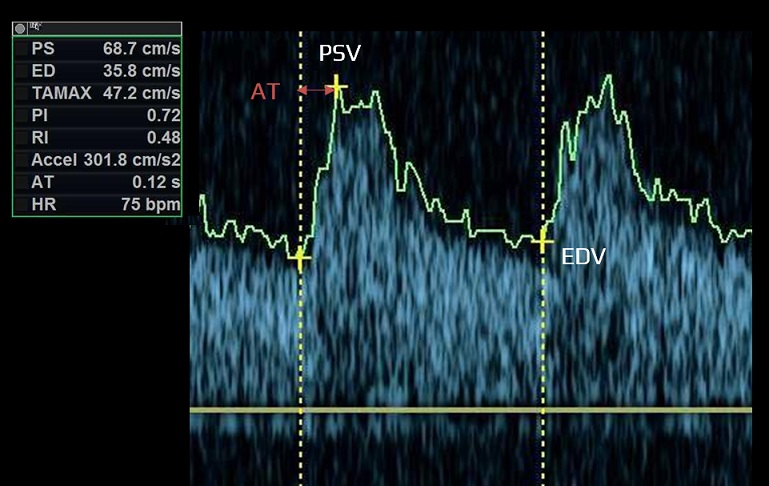
- typical items assessed within the Doppler waveform:
- acceleration time (systolic acceleration)
- time required for blood flow to reach peak velocity from the onset of systole (measured in milliseconds)
- a prolonged acceleration time may indicate proximal arterial stenosis/occlusion, stenosis of the aortic valve, or impaired cardiac contractile force
- peak systolic velocity (PSV) – the highest flow velocity during systole
- dicrotic notch
- a slight, downward deflection observed after the peak systolic velocity. This notch corresponds to aortic valve closure and the beginning of diastole in the cardiac cycle
- a prominent dicrotic notch may be indicative of increased peripheral resistance, commonly observed in conditions such as hypertension
- conversely, a blunted or absent dicrotic notch may indicate low systemic vascular resistance and may be seen in conditions like sepsis
- end-diastolic velocity (EDV)
- EDV is the velocity at the end of diastole; it is influenced by peripheral resistance (including distal stenosis)
- mean velocity (Vmean) is calculated
- resistance index and pulsatility index can be calculated from the above-stated values
- acceleration time (systolic acceleration)
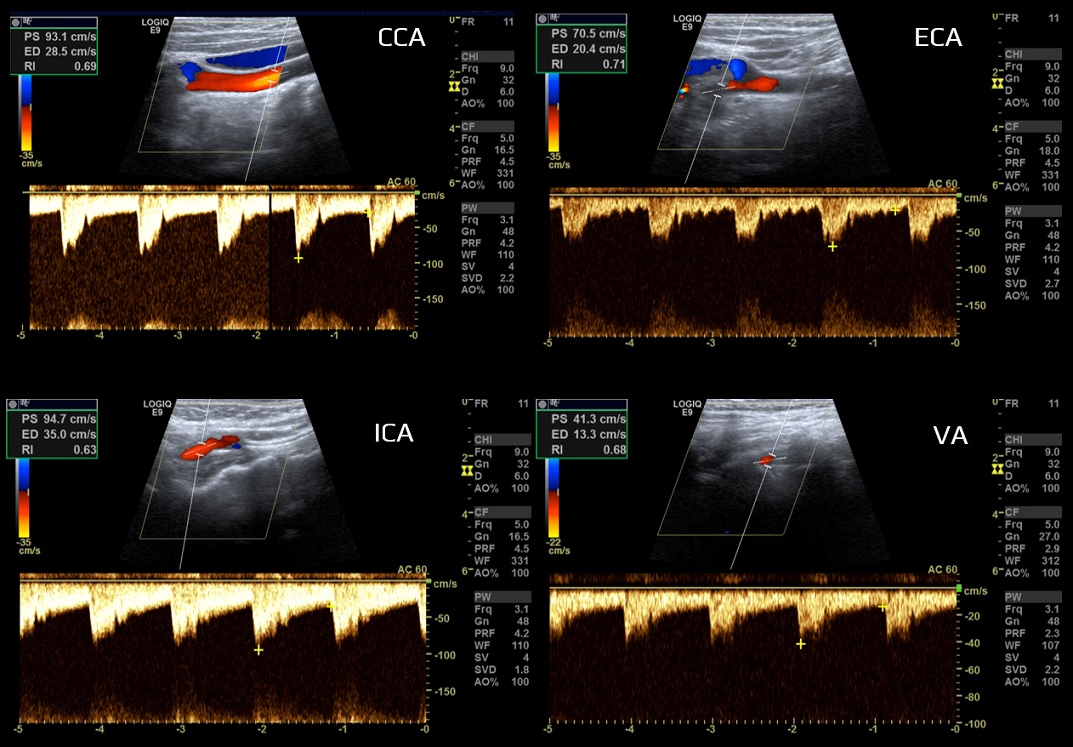
- vessels are classified according to the peripheral resistance
- high-resistance limb type (typically the ECA)
- low-resistance parenchymal type (typically the ICA, VA)
- the CCA waveform has an intermediate profile under physiological conditions because it depends on peripheral resistance in both intracranial (brain) and extracranial regions (skin, muscles)
Examined vessels
Usual arteries to be examined:
- extracranial:
- common carotid artery (CCA)
- internal carotid artery (ICA)
- external carotid artery (ECA)
- superficial temporal artery (one of two terminal branches of the external carotid artery) in suspected temporal arteritis
- superficial temporal artery (one of two terminal branches of the external carotid artery) in suspected temporal arteritis
- vertebral artery (VA)
- subclavian artery (SA)
- TCCD:
- terminal ICA (TICA)
- middle cerebral artery (MCA)
- anterior cerebral artery (ACA)
- posterior cerebral artery (PCA)
- vertebral artery (VA)
- basilar artery (BA)
- ophthalmic artery (OA)
- anterior communicating artery (ACom/AComA)
- posterior communicating artery (PCom/PComA)