ISCHEMIC STROKE / ACUTE THERAPY
Surgical treatment of an acute ischemic stroke
Updated on 21/12/2023, published on 27/01/2022
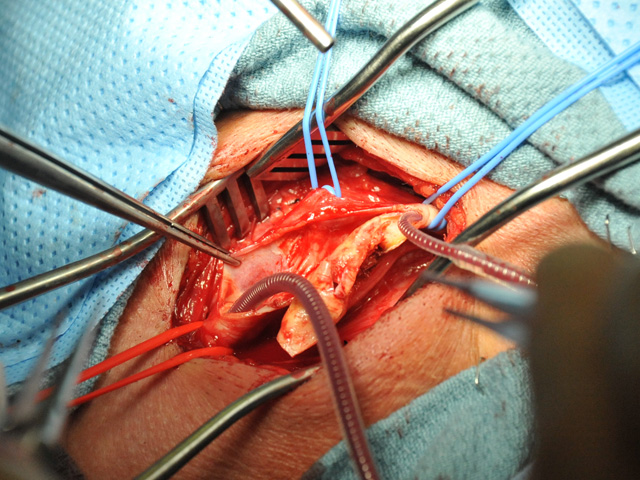
Emergency carotid endarterectomy (< 24h)
- insufficient data on the effectiveness of the method in acute stroke (AHA/ASA 2019 IIb/B-NR)
- surgical risk in neurologically unstable patients is increased, although good results have been reported in case series; no randomized controlled trials (RCTs) are available
- can be considered in the following scenarios:
- crescendo TIA/stroke with the initial mild deficit and small ischemic lesion on CT/MRI caused by significant stenosis or thrombotic ICA occlusion with presumed hypoperfusion mechanism [Gorlitzer, 2009] [Gajin, 2013]
- intracranial occlusion (above skull base) must be excluded; it is challenging to differentiate distal ICA thrombosis from blood stagnation without retrograde contrast filling
- CEA indication is supported by the finding of low flows in the MCA and depleted vasomotor reactivity (CVR) on TCCD and/or significant MR DWI/PWI mismatch
- acute surgical revision of thrombosed ICA after recent CEA (in the absence of intracranial thromboembolic occlusion)
- crescendo TIA/stroke with the initial mild deficit and small ischemic lesion on CT/MRI caused by significant stenosis or thrombotic ICA occlusion with presumed hypoperfusion mechanism [Gorlitzer, 2009] [Gajin, 2013]
- the acuteness of carotid occlusion can be assessed by CT perfusion (CTP) or ultrasound [Herzig, 2011]
Tandem lesion
- in case of simultaneous severe carotid stenosis/occlusion and intracranial occlusion, mechanical embolectomy should be performed (if the relevant criteria are met)
- after a successful intracranial embolectomy, it is possible to proceed with:
- emergency carotid angioplasty with stenting (⇒ issue with antiplatelet therapy arises for thrombolysed patients)
- emergency carotid angioplasty to achieve recanalization with delayed stenting of the adequately medically prepared patient or early CEA
- emergency carotid endarterectomy (Slawski, 2018)
Emergency EC-IC bypass
- the effectiveness and safety of the method are not proven
- endovascular revascularization methods are preferred