ISCHEMIC STROKE / CLASSIFICATION AND ETIOPATHOGENESIS
Antiphospholipid syndrome
Updated on 21/06/2024, published on 28/04/2023
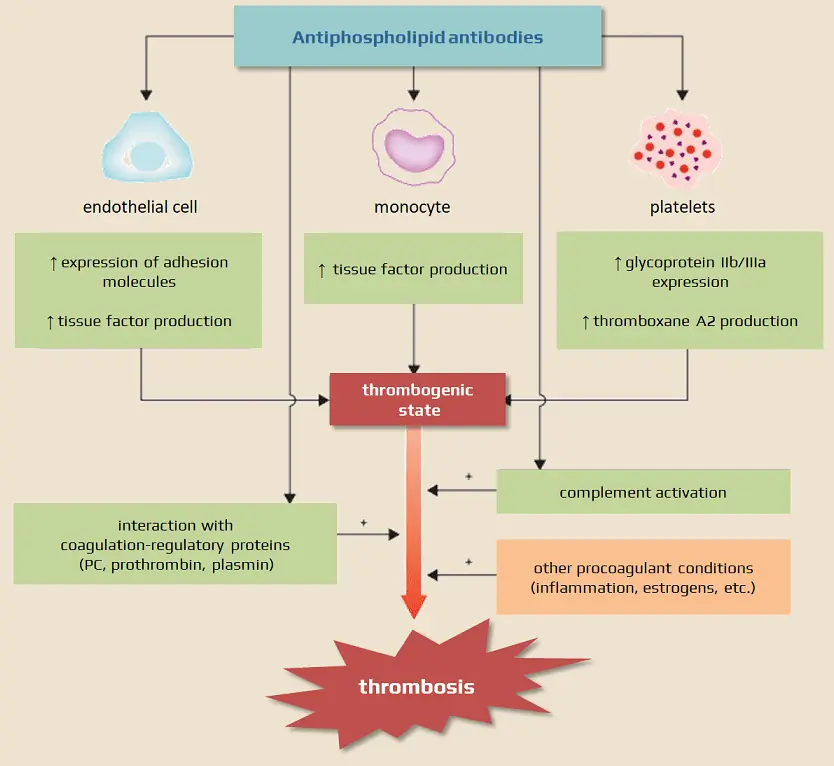
- antiphospholipid syndrome (APS) is an acquired autoimmune disease
- the diagnosis is based on the presence of clinical symptoms (thrombosis or pregnancy morbidity) along with persistently elevated titers of antiphospholipid antibodies (APLA or aPL)
- most people are diagnosed between the ages of 20 and 50, and it affects 3-5 times as many women as men
Classification
|
I. Primary APS
|
|
II. Secondary APS
|
|
Clinical presentation
Neurologic signs and symptoms
- amaurosis fugax
- occlusion of retinal arteries and veins
- TIA/stroke (thromboembolic etiology)
- transverse myelitis (in patients with SLE)
- dural sinus thrombosis
- dementia
- epileptic seizures
- migraine
Other signs and symptoms
-
pulmonary hypertension
-
arterial and venous thromboses and/or pulmonary embolism
-
livedo reticularis
-
valvular vegetations
-
autoimmune thrombocytopenia
-
autoimmune hemolytic anemia
-
the rare microangiopathic form can lead to fatal Multiple Organ System Dysfunction (MOSD) – known as catastrophic antiphospholipid syndrome (CAPS)
Pathologic conditions related to pregnancy
-
repeated early abortions
-
unexplained fetal deaths in the 2nd and 3rd trimesters
-
severe pre-eclampsia
-
chorea gravidarum
-
severe fetal growth restriction
Diagnostic evaluation
Laboratory tests
The 3 main types of antiphospholipid (aPL )antibodies are:
- lupus anticoagulans (LA)
- anticardiolipin antibodies (ACLA)
- anti-β2-glycoprotein I (anti-β2GPI)
- LA is most specific for predicting thrombosis; the concurrent presence of both ACLA and anti-β2GPI further increases the risk
- testing should be performed before or after the discontinuation of heparin/warfarin
- after 3 months, discontinue warfarin for a short period and collect the blood samples
- a prophylactic dose of LMWH does not affect the test results
- after 3 months, discontinue warfarin for a short period and collect the blood samples
- testing outside pregnancy is recommended for patients with pregnancy-related disorders
- detection of antibodies alone, especially at low titers, is highly nonspecific and cannot be used to establish a diagnosis ⇒ in antiphospholipid syndrome, antibodies should be high and repeatedly present at high titers (a minimal interval of ∼ 3 months between the 2 samples) to confirm the diagnosis
- testing asymptomatic individuals for the presence of antiphospholipid antibodies is not recommended; even if antibodies are present, primary thromboprophylaxis is not indicated (AHA/ASA 2010 III/B)
- routine testing of individuals with TIA/stroke is not recommended unless they have other symptoms of APS and no evident stroke etiology (AHA/ASA 2014 III/C)
Neuroimaging
CT+CTA, MRI+MRA, SPECT
- regional blood flow disorders
- infarcts, white matter lesions
→ FAZEKAS
- cortical atrophy
- venous sinus thrombosis
- arterial occlusion or stenosis
Diagnostic criteria
| I. Clinical criteria | |
| 1. Thrombosis – ≥ 1 attack of venous /arterial thrombosis | |
2. Pregnancy-related disorders
|
|
| II. Laboratory criteria |
|
|
|
| Antiphospholipid syndrome is present if at least one clinical and one laboratory criterion is present |
Therapy
Primary thromboprophylaxis
- testing of asymptomatic individuals and primary thromboprophylaxis are not recommended
Secondary stroke prevention
- the decision to initiate antiplatelet or anticoagulant therapy depends on the assessment of the individual risk of thrombosis and the risk of bleeding with anticoagulant therapy
- the risk of thrombosis depends on:
- titer and type of antibodies detected
- extent or frequency of thrombotic events and their location
- according to the APASS trial, there was no statistically significant difference between ASA and low-dose warfarin (INR 1.5-2.8)
- only a minority of patients had high LA and ACLA titer
- only a minority of patients had high LA and ACLA titer
- antiplatelet therapy is recommended for patients with low antibody titers who do not meet APS criteria (AHA/ASA 2021 1/B-NR)
- initiate anticoagulation therapy in patients with repeated high titers who meet APS criteria
- prefer warfarin with INR 2.5-3 (AHA/ASA 2021 2a/B-R)
- DOACs – insufficient data, higher risk of recurrence compared to warfarin according to observational studies; ASTRO-APS trial with apixaban is ongoing
- rivaroxaban is specifically not recommended in patients with a history of thrombosis and triple antibody positivity due to increased risk of bleeding (AHA/ASA 2021 3/B-R)
- dual antiplatelet therapy (DAPT) ASA + clopidogrel could be an alternative, but strong data are not yet available to make a strong recommendation (AHA/ASA 2021) [Ohnishi, 2019]
- the usefulness of a combination of warfarin + ASA is not established; there is a consensus in favor of anticoagulation alone
Deep vein thrombosis and APS
- long-term WARFARIN with INR 2.5-3
- DOAC rather not, further RCTs are required → more here
- rivaroxaban – TRAPS trial showed worse results than warfarin
- apixaban – ASTRO-APS trial is ongoing
Management of pregnant women with APS
- APS patients without a history of thrombosis and miscarriage: no clear recommendation; LWMH or LMWH+ASA can be used
- patients with APS + recurrent miscarriage (≥3): LMWH + aspirin 50 mg once daily
- treatment should be initiated as soon as possible after confirmation of pregnancy
- patients with APS + history of pre-eclampsia/eclampsia: aspirin 50mg once daily
- patients with APS + history of thrombosis: LMWH as thromboprophylaxis
- postpartum thromboprophylaxis with LMWH
- 6 weeks in patients with a history of thrombosis, 7 days for all others
- 6 weeks in patients with a history of thrombosis, 7 days for all others