ADD-ONS / ANATOMY
Anatomical variants of cerebral arteries
David Goldemund M.D.
Updated on 10/04/2024, published on 24/11/2022
 Overview of anatomical variants
Overview of anatomical variants
Variants in the arrangement of blood vessels supplying the brain are quite common. While they are often of minor clinical significance, their knowledge and recognition are essential if surgical or endovascular treatment in the head or neck is considered. Unfavorable vascular anatomy complicating endovascular treatment is discussed separately.
| Anomalous vessel morphology |
| Persisting communicants and aberrant vessels |
|
 Clinical significance of anatomical variants
Clinical significance of anatomical variants
| Distinguish anatomical variations from pathology, as it has implications for the supplied area and surrounding structures |
|
| Hemodynamic consequences |
|
| Association with other anomalies |
|
| Planning a surgical or endovascular procedure |
|
 Hypoplasia and absence of the carotid artery
Hypoplasia and absence of the carotid artery
| Content available only for logged-in subscribers (registration will be available soon) |
 Hypoplasia/aplasia of the vertebral artery
Hypoplasia/aplasia of the vertebral artery
Aplasia
- rare anomaly (~1%)
- contralateral VA is compensatorily enlarged (diameter >4 mm)
- only the vertebral vein can be detected on the affected side
Hypoplasia
- relatively common anatomical variety (~1-6%; more often on the right side)
- lumen diameter < 2-3 mm (different cut-offs reported)
- ultrasound findings: PSV < 40cm/s, increased peripheral resistance (↑ PI, RI) but non-zero diastolic flow (adjust scale properly)
- compensatory enlargement of the contralateral VA accompanies hypoplasia/aplasia
- hypoplastic vessel may terminate in PICA (~ 0.2%)
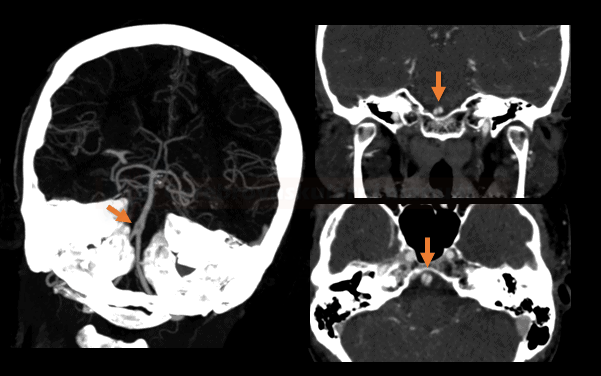
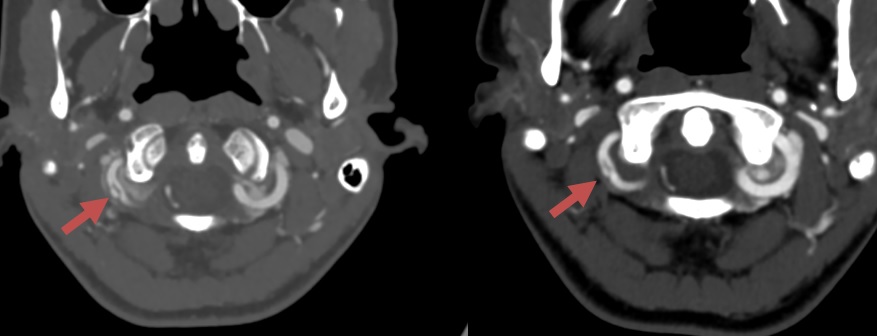
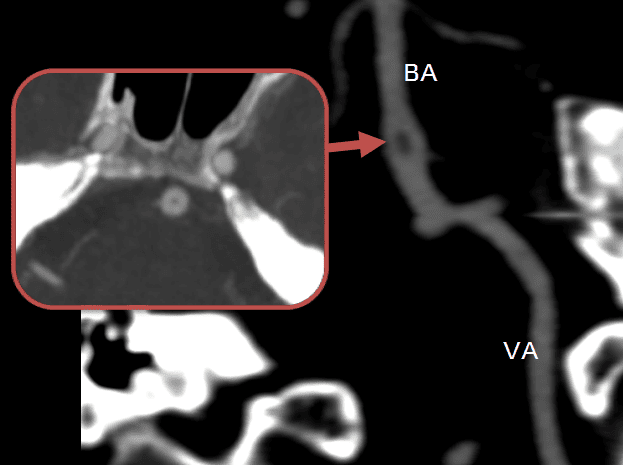
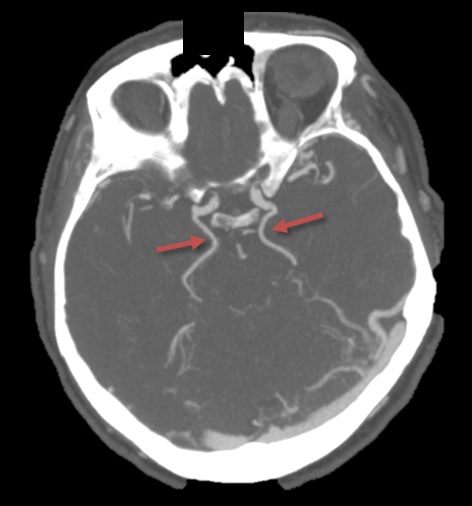
 Fenestrations and duplications
Fenestrations and duplications
- duplication – two separate arteries instead of one
- fenestration – the partial splitting of an artery (each part has its own media and intima, adventitia may be shared)
- can be confused with thrombus or dissection [Wang, 2020] [Tourdias, 2011]
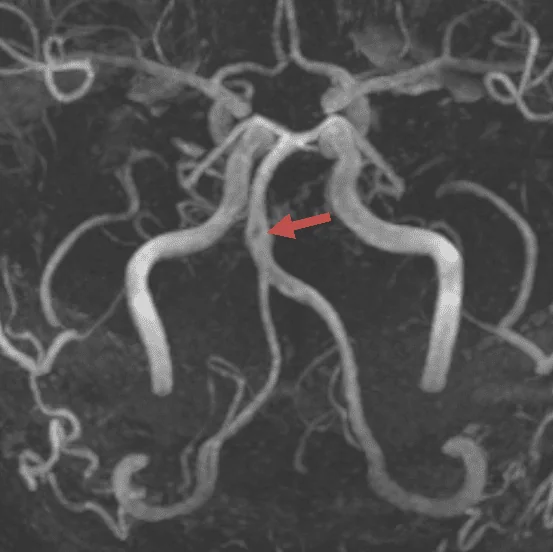
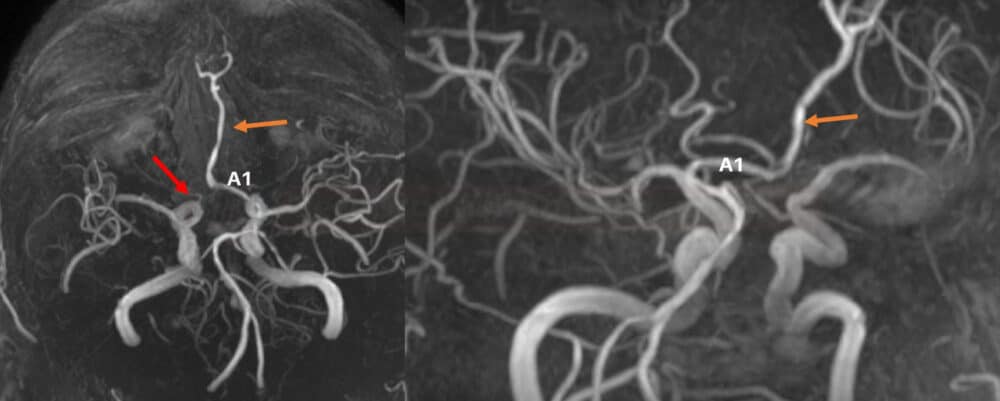
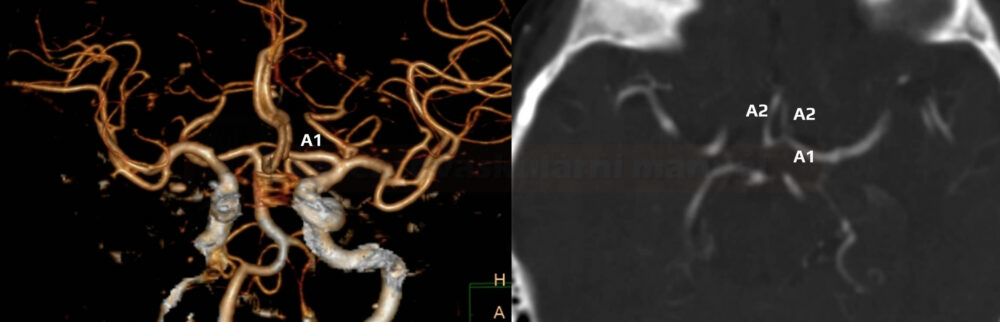
Azygos anterior cerebral artery
- the persistent embryonic middle artery supplying the corpus callosum is a rare vascular anomaly with a prevalence of 0.2-4% [Dimmick, 2009]
- both ACA territories are supplied by a single A2 trunk ⇒ its occlusion causes a bihemispheric ischemia
Bihemisferic ACA
- hypoplasia of one A2 segment; contralateral ACA supplies both hemispheres
- prevalence 2-7%
- hypoplastic A2 segment distinguishes this variety from the anterior azygos artery; the clinical significance is similar
Anterior communicating artery (AComA) hypoplasia/aplasia
- AComA may not be apparent on angiography; however, this does not necessarily indicate its absence
- the prevalence of true aplasia is about 5% based on surgical findings
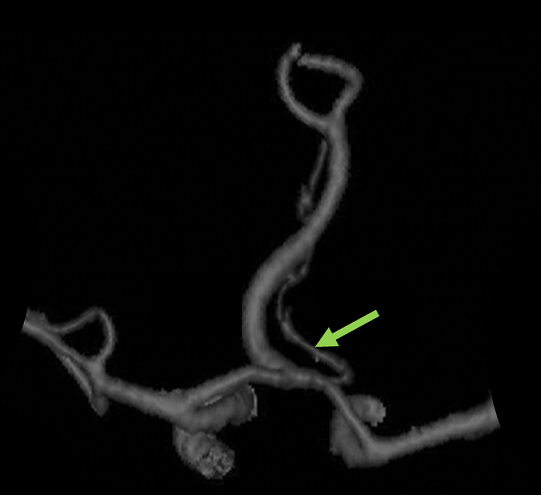
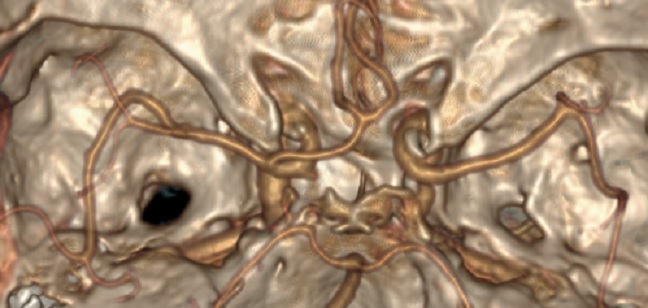
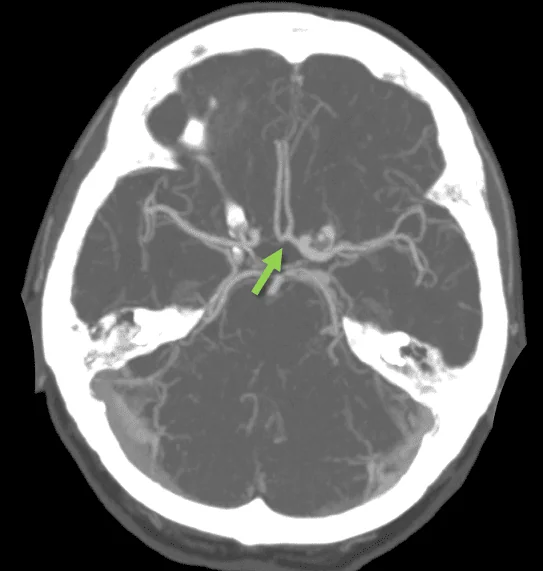
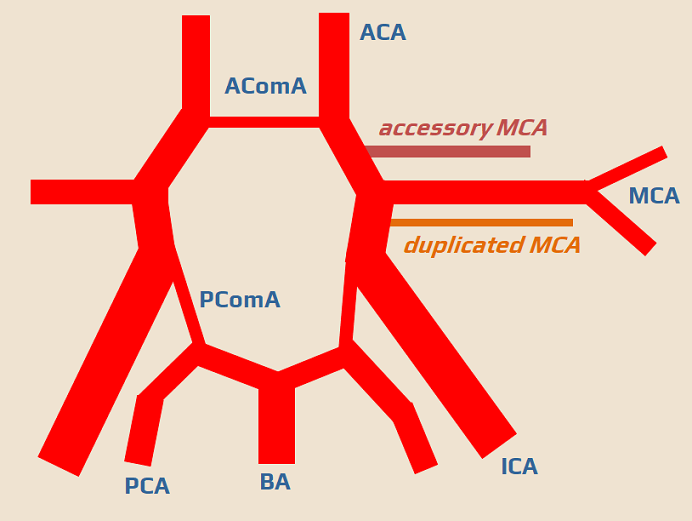
Accessory and duplicated middle cerebral artery
- an accessory MCA arises from the A1 segment of the ACA and runs parallel to the M1 segment of the MCA; prevalence is 2-3%
- a duplicated MCA arises from the distal ICA
- both the recurrent Heubner artery and the accessory MCA represent primitive anastomoses with the piriform cortex. The accessory MCA disappears during normal development.
- clinical significance
- aneurysms may form in the proximal segment of the accessory ACM
- accessory MCA may serve as a collateral circulation during occlusion of the main MCA
Variations of MCA branching
| Content available only for logged-in subscribers (registration will be available soon) |
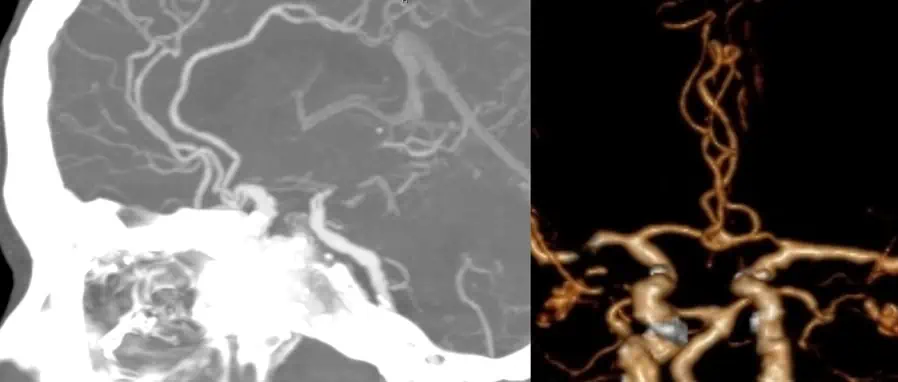
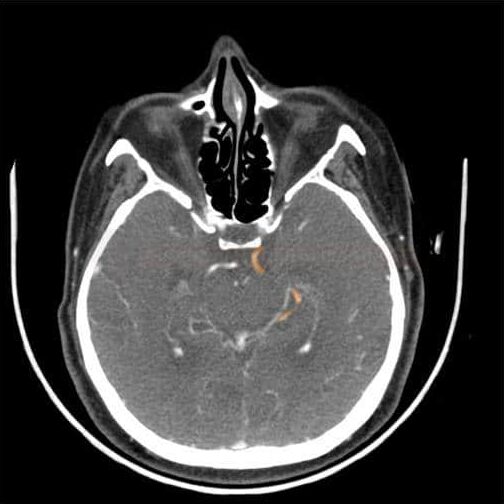
Fetal PCA
- during early development, the PCA arises from the ICA; persistence of this configuration is termed a fetal-type PCA
- PComA typically has a larger caliber compared to the P1 segment of the PCA
- classification of fetal PCA
- complete – P1 segment is absent
- partial – P1 segment is hypoplastic and has a smaller diameter than the PComA
- prevalence approx. 10-26%
- bilateral fetal PCA may be associated with hypoplasia/aplasia of the terminal segment of the basilar artery
Percheron artery
| Content available only for logged-in subscribers (registration will be available soon) |
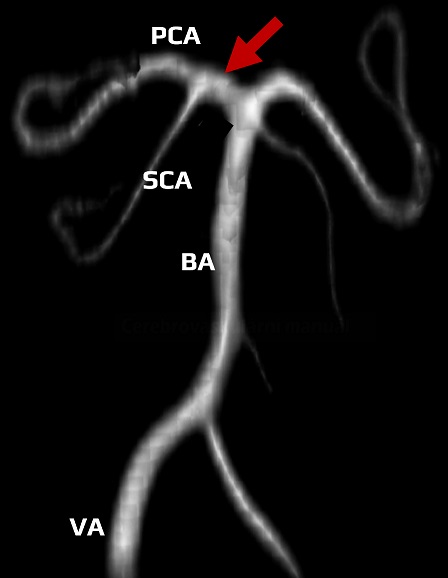
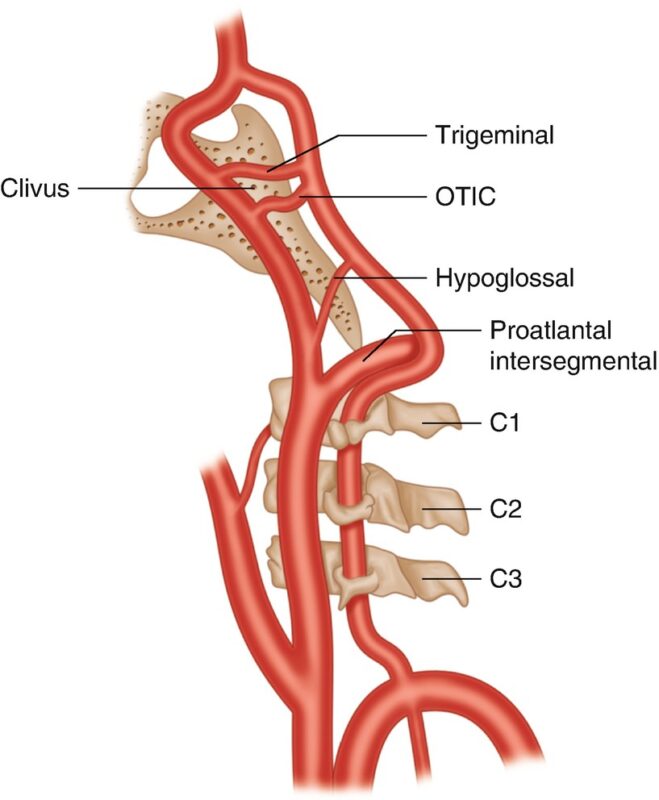
 Persistent communication between the ICA and the BA
Persistent communication between the ICA and the BA
During embryonic development, a number of arteries either disappear or transform into others. Rarely, these persist after birth (prevalence ~ 0.1-1%). These include, for example, persistent fetal arterial anastomoses between the internal carotid artery (ICA) and the posterior circulation (vertebrobasilar):
- Persistent Primitive Trigeminal Artery (PPTA)
- Primitive otic and hypoglossal artery
- Proatlantal Intersegmental Artery (PIA)
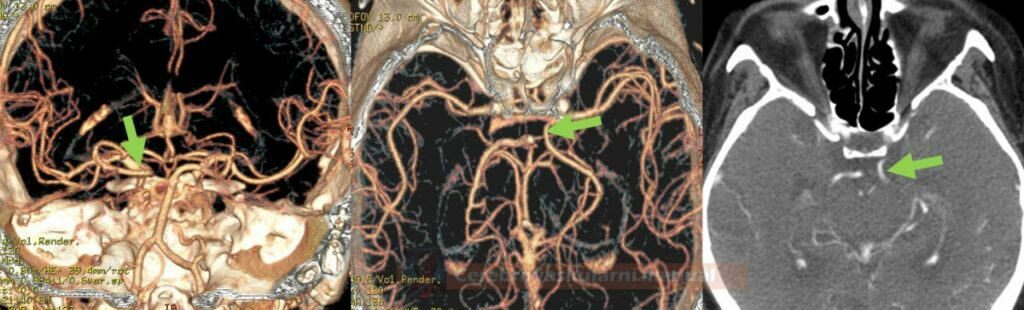
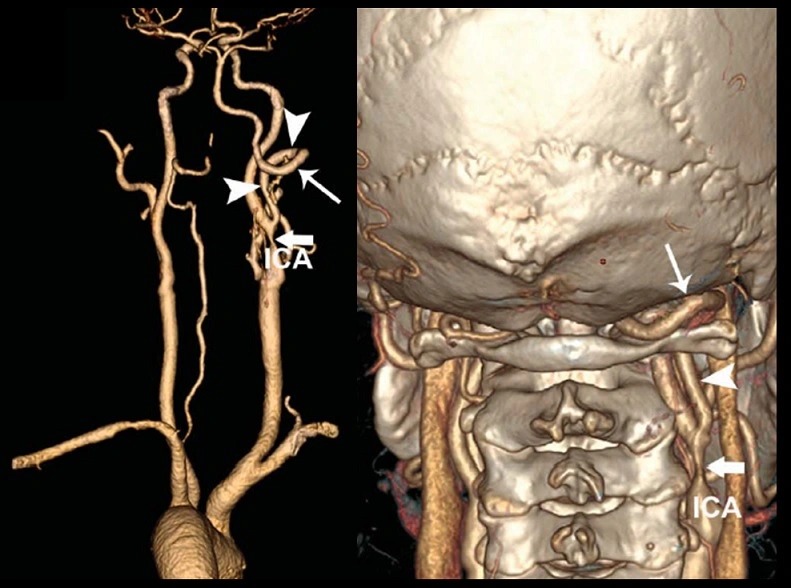
Proatlantal intersegmental artery (PIA)
- type I: (~55%)
- arises from the ICA
- corresponds to the first segmental artery
- does not pass through intervertebral foramina
- type II: (~40%)
- arises from the ECA
- corresponds to the second segmental artery
- it passes through the foramen magnum (as opposed to the hypoglossal artery, which enters intracranially via the hypoglossal canal)
Persistent trigeminal artery (PTA)
| Content available only for logged-in subscribers (registration will be available soon) |
Persistent primitive hypoglossal artery (PPHA)
 Persistent communication between ICA and ECA
Persistent communication between ICA and ECA
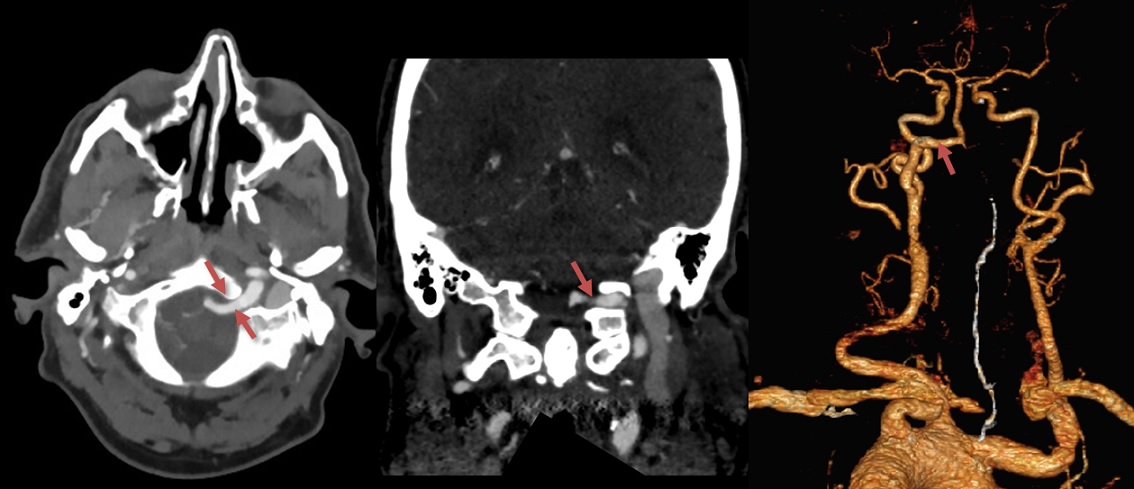
Persistent stapedial artery (PSA)
- temporary embryonic communication between the ECA and ICA
- persists in ~ 0.5% of the population
- clinical significance:
- may cause pulsatile tinnitus
- may be misdiagnosed as a glomus tumor on CTA
- may complicate otolaryngological (ENT) surgery and cause severe bleeding
- management varies from observation to surgical intervention, depending on the symptomatic burden and associated pathology
 Other anomalies
Other anomalies
- left-sided brachiocephalic trunk (BCT)
- bilateral absence of ECA (often associated with PIA)
- persistent first cervical intersegmental artery
- rare; can cause compressive symptoms or be a surgical consideration in neck operations
- ACE arising from the aortic arch in combination with ipsilateral PIA
- may complicate surgical or interventional procedures
- common origin of the BCT and the left CCA from the aortic arch