ISCHEMIC STROKE / ETIOLOGY
Susac syndrome
Updated on 15/07/2024, published on 18/02/2022
- rare microangiopathy affecting the arteries of the brain, retina, and cochlea (retino-cochleo-cerebral dysimmune vasculopathy)
- in partial forms of this syndrome, only 2 of the 3 components are clinically apparent. There are reports of subacute bilateral sensorineural hearing loss with bilateral retinal artery occlusion without apparent cerebral dysfunction
- described by John Susac in 1979 (first reported in 1973) (Pfaffenbach, 1973)
- initially termed “small infarctions of cochlear, retinal, and encephalic tissues (SICRET)” syndrome or “retinopathy, encephalopathy, and deafness microangiopathy (RED-M)” syndrome
- predominantly affects females (3:1) in the 2nd-4th decade (range 7-72 years), often associated with delivery
- the exact cause is unknown; autoimmune microangiopathy or autoimmune coagulopathy (with APL positivity) are considered (Bucciarelli, 2014)
- different pathogenetic mechanisms can cause the same clinical syndrome
Clinical presentation
- most commonly monophasic, progressive course
- brain dysfunction
- acute or subacute encephalopathy (neuropsychiatric manifestations)
- headaches
- stroke
- epileptic seizures
- cranial neuropathies
- sensorineural hearing loss, tinnitus, vestibular dysfunction
- ocular symptoms
- visual disturbances (visual field defects) – due to retinopathy (occlusion of the retinal artery or its branches – BRAO)
- uveitis
Diagnostic evaluation
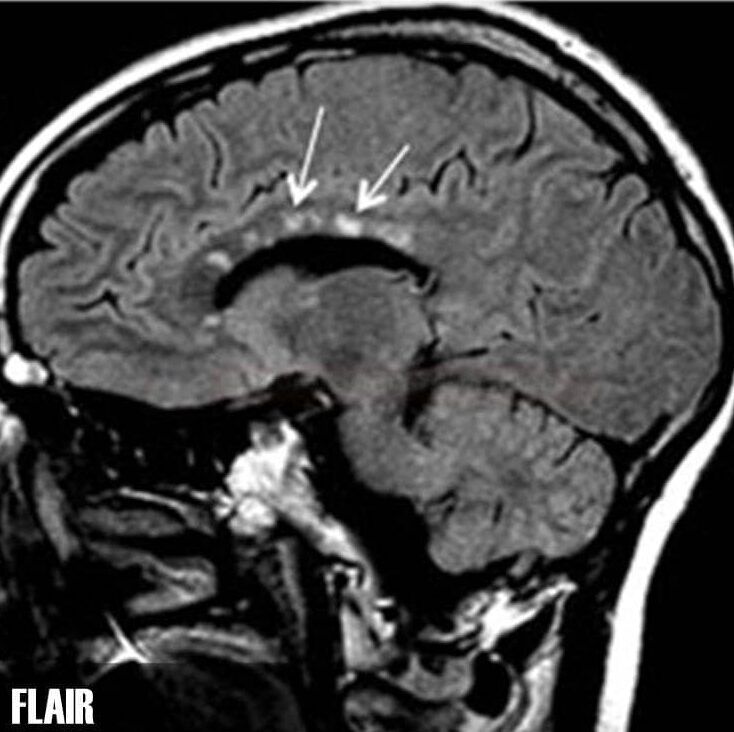
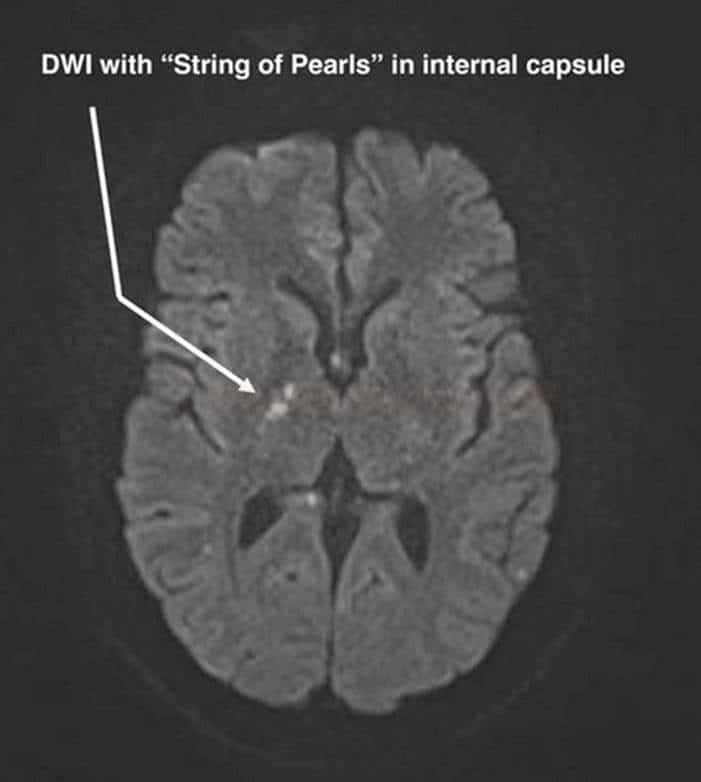
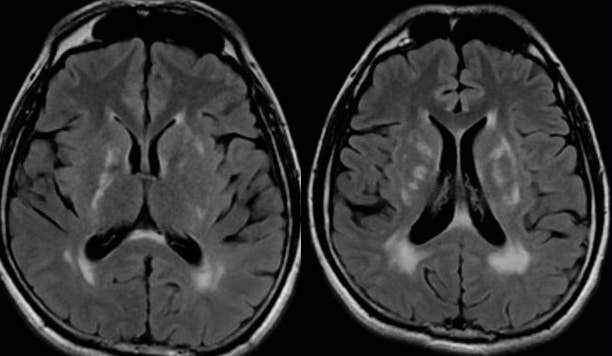
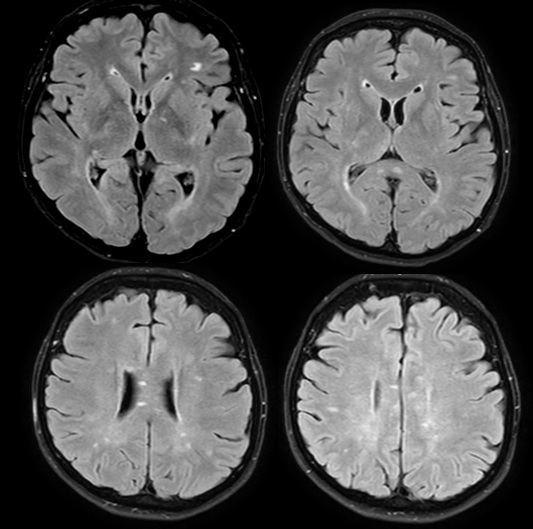
Brain imaging (MRI)
- leukoencephalopathy with a tendency to involve the central corpus callosum
- microinfarcts in the internal capsule – “string of pearls“
- specific lesions in the corpus callosum – “snowball lesions“
- grey matter involvement and leptomeningeal enhancement may be present (in ~ 30%)
- such findings are useful in the DDx of MS and ADEM
Ophthalmological examination
- widefield fluorescein angiogram can show artery occlusion
- peripheral branch retinal artery occlusion (BRAO)
- segmental vessel wall increased fluorescence/leakage, capillary dropout, peripheral nonperfusion, and peripheral capillary changes
- peripheral branch retinal artery occlusion (BRAO)
- look for signs of uveitis
Laboratory tests
- CSF
- oligoclonal bands are commonly absent
- sporadic lymphocytic pleocytosis or elevated CSF protein may occur
- CBC: occasional monocytosis or eosinophilia
- mild elevation of serum antinuclear and/or antiphospholipid antibodies
Diagnostic criteria
| Suspected | Incomplete | Complete |
| 1 symptom | 2 symptoms | complete clinical triad (approx 13%) |
| absence of significant vascular risk factors (atherosclerosis and/or coagulopathy) | ||
+ one of the following risk factors:
|
||
Dg. criteria according to Vishnevskia-dai
Differential diagnosis
- demyelinating diseases
- multiple sclerosis (MS)
- NMO
- ADEM
- multi-infarct disorders
- other autoimmune diseases
- antiphospholipid syndrome
- Behçet’s disease
- Takayasu arteritis
- granulomatosis with polyangiitis (Wegener’s)
- systemic lupus erythematosus (SLE)
- sarcoidosis
- Sjögren’s syndrome
- infections
- Creutzfeldt Jakob disease
- Lyme borreliosis
- viral encephalitis
- syphilis
- Progressive Multifocal Leukoencephalopathy (PML)
- malignancy/paraneoplastic syndrome
Management
- treatment of Susac syndrome must be aggressive and sustained to control symptoms and prevent further brain damage and vision loss
- the mainstay of treatment is immunosuppressive therapy
- plasma exchange in refractory cases (Salazar, 2024) (Vilayet, 2023)
- antiplatelet therapy (commonly aspirin or clopidogrel)