NEUROIMAGING / NEUROSONOLOGY
Neurosonology in intensive care
Updated on 25/01/2024, published on 15/02/2023
Monitoring of intracranial hypertension
B-mode |
Midline shift
- transtemporal approach, using the thalamic plane
- set the depth to 15-16 cm
- from both temporal approaches, measure the distance of the midline structures (preferably the middle of the third ventricle) from the inner edge of the contralateral bone. Subtract the two measurements from each other and divide the result by two
- another approach is to measure the distance from the probe to the center of the 3rd ventricle
[Stolz, 1999] [Motuel, 2014]
3rd ventricle width
- mesencephalic and thalamic planes via a transtemporal approach are used
- the width of the 3rd ventricle is defined as the distance between two echogenic lines bordering the anechogenic strip (normal width < 10 mm)
- the shaking test can be used to distinguish between normotensive and hypertensive hydrocephalus, for which the M-mode is used
Measurement of the optic disc elevation
- transorbital access using a 9-12 MHz probe
- direct measurement and monitoring of optic disc prominence
- not suitable for monitoring dynamic changes (unlike the ONSD measurement)
Optic nerve sheath diameter (ONSD)
- the optic nerve sheath (ONS) is an anatomical extension of the dura mater and the subarachnoid space around the optic nerve is continuous with the intracranial subarachnoid space
- any increase in pressure within the intracranial compartment affects the optic nerve head as swelling of the optic disc (papilledema)
- papilledema takes time to develop + ophthalmoscopy requires skill for accurate identification [Hansen, 1997]
- dilatation of the optic nerve sheath has been shown to be a much earlier manifestation of intracranial hypertension
- the optic nerve sheath is relatively easy to visualize with trans-orbital insonation
Doppler ultrasound
|
Doppler waveform changes
- increased PI and RI (due to the decrease in EDV)
- later, a gradual decrease in PSV may occur
- in severe conditions, flow reversal in late systole may be detected → initial stage of intracranial circulatory arrest
- approximate calculation of ICP= 10.927 x PI -1.284 (Balner equation) [Brandi, 2010]
Non-invasive ICP measurement (Vittamed)
- principles of the method can be found here
- a clinical trial is being prepared (→ more here)
Occlusion detection, recanalization monitoring
- transcranial Doppler (TCD or TCCD) is an ideal noninvasive, real-time bedside tool for the evaluation of cerebral vessels, particularly in the setting of an acute stroke
- strong correlation exists between TCCD and CTA
- an abnormal TCD/TCCD study, defined as either no or asymmetrical MCA flow, is associated with poor outcome
- direct signs of occlusion:
- indirect signs:
- assessment of basilar artery occlusion (BAO), especially of its distal segment, may be challenging
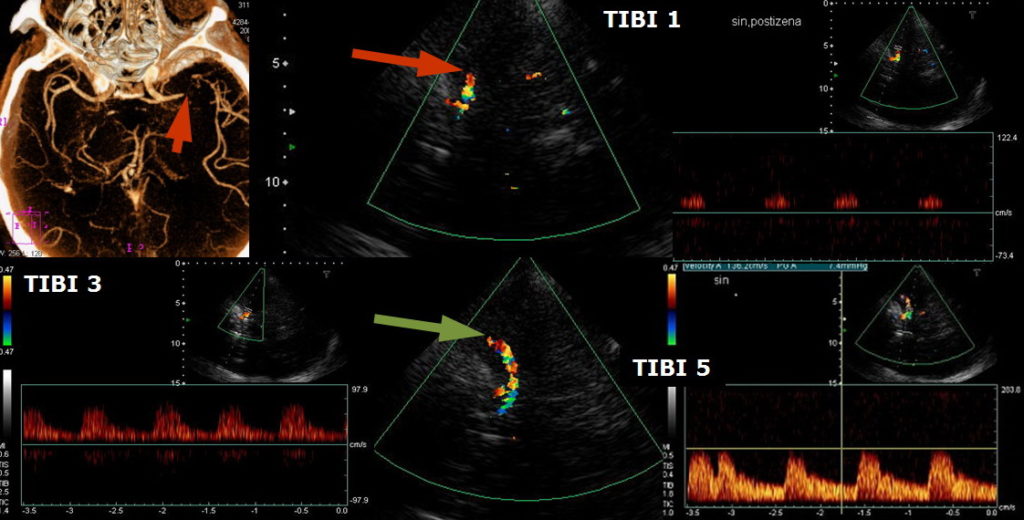
TIBI (Thrombolysis in Brain Ischemia)
- the TIBI classification was developed to grade residual flow
- it correlates with initial stroke severity, clinical recovery, and mortality in acute stroke patients
- no improvement in the residual flow correlates with the absence of early clinical recovery and increased mortality (Demchuk, 2012)
- no improvement in the residual flow correlates with the absence of early clinical recovery and increased mortality (Demchuk, 2012)
According to [Demchuk, 2001]
| Recanalization assessment [Clotbust, 2007] |
|
| Complete recanalization | TIBI 4-5 |
| Parcial recanalization | increase of TIBI by ≥1 grade (but not to 4 or 5) |
| Reocclusion | decrease of TIBI by ≤1 grade |
COGIF
Differentiation of TIBI grades 1-3 (minimal flow, blunted flow, dampened flow) may be difficult. The flow patterns of these grades not only reflect partial M1 recanalization but also the hemodynamic situation in other segments. The COGIF scoring system was designed to more clearly follow the recanalization process; it is exclusively based on known hemodynamic changes of the Doppler spectrum. The time course of grades during the serial examination must be encoded.
| Recanalization assessment | |
| Complete recanalization |
COGIF 4 |
| Partial recanalization |
improvement by ≥1 grade (but not to 4) |
| No change |
baseline COGIF grade persists |
| Worsening | decrease by ≥1 grade |