ISCHEMIC STROKE / ETIOPATHOGENESIS
Aortic arch atherosclerosis
Updated on 06/11/2023, published on 16/04/2023
Anatomy
- the aorta is the main and largest artery in the human body
- it originates from the left ventricle and extends down to the abdomen, where it branches into the common iliac arteries and a small median sacral artery
- it consists of these segments:
- ascending aorta
- coronary arteries originate in the aortic sinuses
- aortic arch
- the arch has 3 major branches: the brachiocephalic trunk, the left common carotid artery, and the subclavian artery
- aortic arch ends, and the descending aorta begins approx. at the level of the Th4-5 intervertebral disc
- descending aorta (divided by the diaphragm at the level of Th12 into the thoracic and abdominal parts)
- major thoracic branches: intercostal and subcostal arteries, the superior and inferior left bronchial arteries, and variable branches to the esophagus, mediastinum, and pericardium
- major abdominal branches: lumbar and musculophrenic arteries, renal and middle suprarenal arteries, and visceral arteries (the celiac trunk, the superior mesenteric artery, and the inferior mesenteric artery)
- ascending aorta
- in healthy adults, the aorta is usually less than 40 mm in diameter and gradually narrows downwards
- the aorta enlarges with age at a rate of about 0.9 mm every ten years in men and 0.7 mm every ten years in women
Aortic conditions and diseases
- aortic atherosclerosis
- inflammatory disorders (e.g., Takayasu arteritis)
- aortic aneurysms and pseudoaneurysms (abdominal, thoracic, thoracoabdominal)
- acute aortic syndromes (AAS)
- aortic dissection – type A and B
- intramural hematoma (IMH)
- penetrating aortic ulcer (PAU)
- aortic dissection – type A and B
- traumatic aortic injury
- genetic syndromes (e.g., Marfan syndrome)
- congenital defects (e.g., coarctation of the aorta)
Aortic arc atherosclerosis
- aortic arch atherosclerosis is common in individuals aged over 60
- there is an increased risk of thrombus formation, which may be the source (along with atheroma particles) of systemic or cerebral emboli
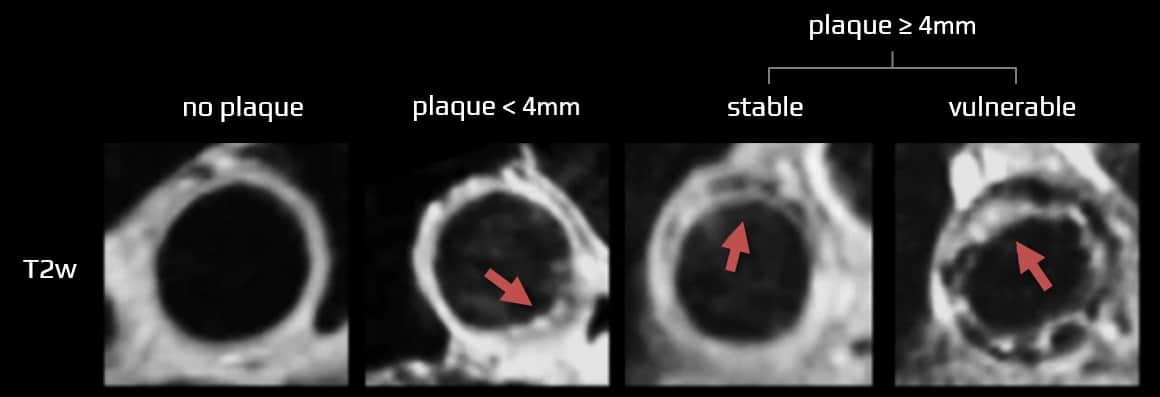
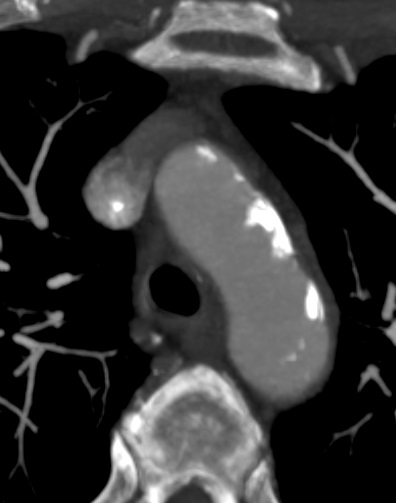
- the advent of transesophageal echocardiography (and later CTA/MRA) allowed the detection of atherosclerotic plaques within the aortic arch
Clinical presentation
- involvement of each aortic segment is associated with specific consequences and complications
- ascending aorta and arch: stroke, systemic embolization (distal arch)
- abdominal aorta: aneurysm formation, abdominal angina, PAD, etc.)
- atheromatous plaques in the aortic arch are associated with an increased risk of cerebrovascular embolic events (→ complications during extracorporeal circulation)
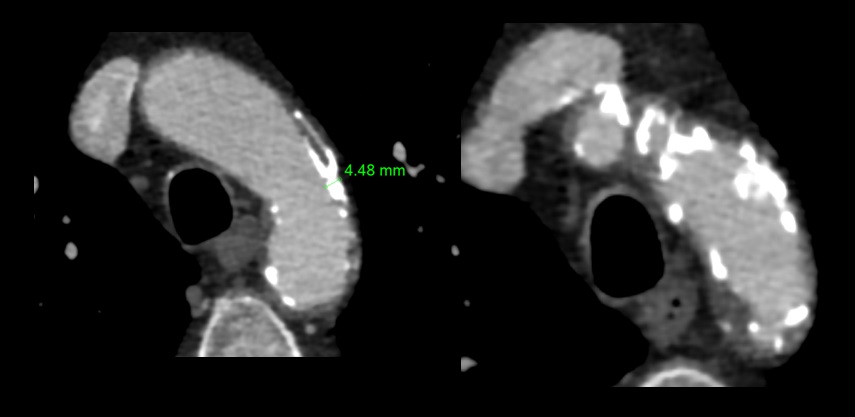
- especially plaques ≥ 4 mm are associated with an increased risk of recurrent stroke
- extensive aortic arch atherosclerosis is also associated with an increased risk of “silent” white matter lesions [Tugcu, 2016]
- assessment of the aortic arch may help identify individuals who may benefit from aggressive treatment of vascular risk factors
- stroke caused by aortic arch atherosclerosis is usually classified as large artery atherosclerosis (CISS, TOAST 1) or cardio-aortic embolism (SSS-TOAST 2)
Risk factors of atherosclerosis
- atherosclerosis is a complex systemic disease in which vascular risk factors play a critical role
Diagnostic evaluation
Clinical examination and laboratory tests
- clinical examination
- palpation and auscultation of the neck and abdomen to detect a noticeable pulsation or turbulent flow causing murmurs
- blood pressure measurement on both arms
- laboratory examination – screening for cardiovascular risk factors
Imaging methods
| Content available only for logged-in subscribers (registration will be available soon) |
Management
Vascular risk factors management
- complex and aggressive management of vascular risk factors is indicated (patients with aortic atherosclerosis belong to the very high-risk group)
Antiplatelet therapy
- stroke patients or asymptomatic patients with extensive aortic atherosclerosis should receive antiplatelet therapy unless anticoagulation is indicated for another reason (e.g., Afib) (AHA/ASA 2021 1/C-LD)
- consider short-term anticoagulant treatment on a case-by-case basis in the presence of documented mobile thrombus
Surgery/stenting
- there are no data on the benefit of prophylactic aortic arch surgery or stenting to prevent stroke