ISCHEMIC STROKE / CLASSIFICATION AND ETIOPATHOGENESIS
CRYPTOGENIC STROKE
Updated on 11/04/2024, published on 17/12/2021
Definition of cryptogenic stroke
- cryptogenic stroke (CS) = a stroke of unknown etiology (a diagnosis of exclusion)
- TOAST 5 (no strict diagnostic algorithm defined)
- ASCOD (Atherosclerosis, Small Vessel Disease, Cardiac Causes, Other, and Dissection)
- CCS (Causative Classification System)
- CISS
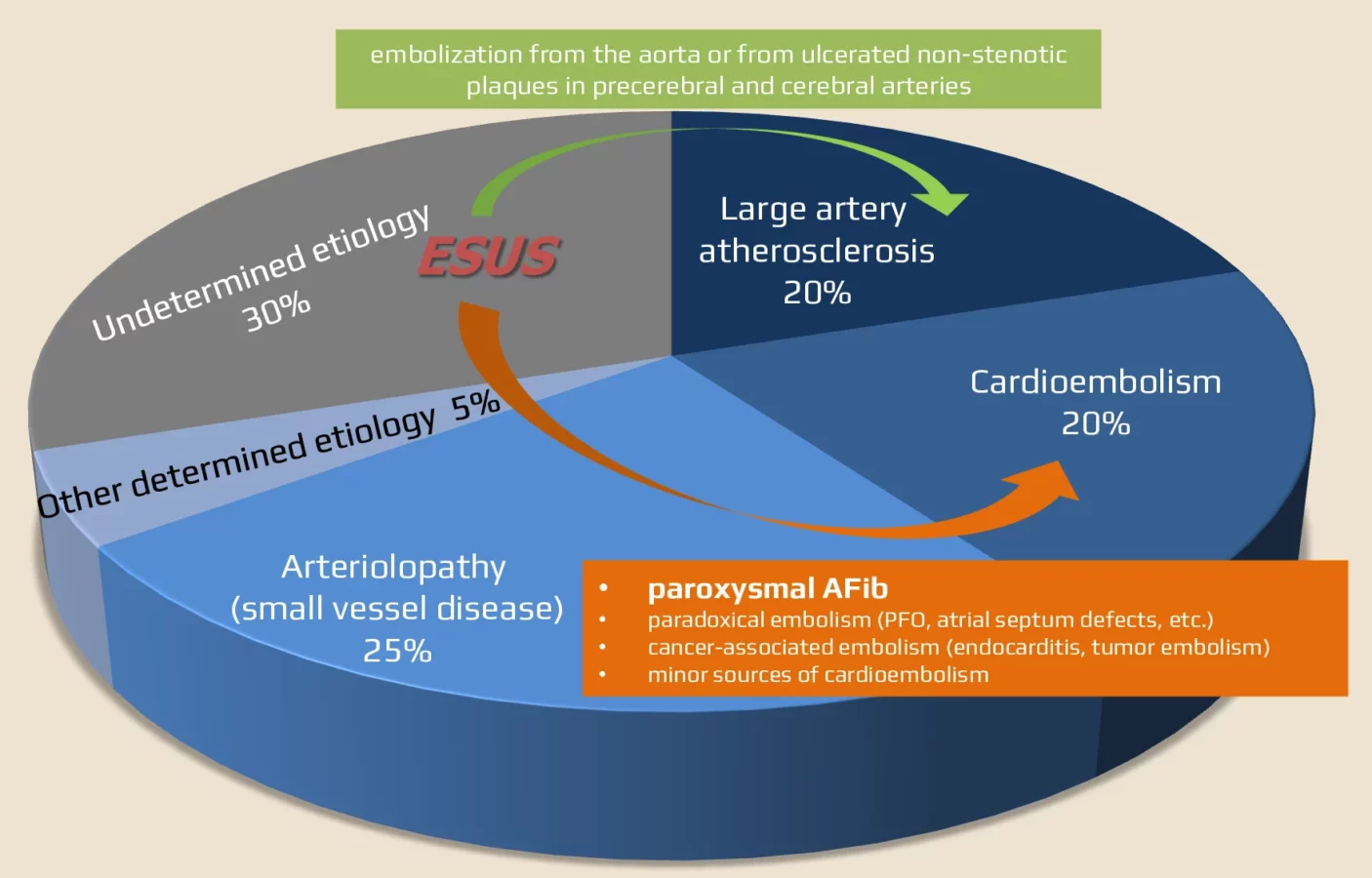
- CS accounts for 15-40% of strokes (Yaghi, 2017)
- CS seems to be more common in younger patients (juvenile strokes) – accounting for up to 40% of patients < 55y of age [Bang, 2014] [Meier, 2003], [Putaala, 2009]
- however, some studies have found lower rates of CS in younger versus older patients
- results depend on the diagnostic criteria used (TOAST overestimates the number of patients with stroke of undetermined etiology (TOAST 5), mainly because patients with ≥ 2 potential etiologies fall into this group
- the diagnosis of cryptogenic stroke can only be made after a thorough diagnostic evaluation → see here
- detection of occult paroxysmal AFib is a priority in older patients (EMBRACE, CRYSTAL AF)
- PFO detection is a priority in younger patients
- also search for aortic arch atherosclerosis, atrial cardiopathy, and sub-stenotic atherosclerosis (unstable non-stenotic plaques)
- the well-defined subtype of CS is Embolic Stroke of Undetermined Source (ESUS)
ESUS (Embolic Stroke of Undetermined Source)
| ESUS criteria (must meet all) |
Non-lacunar infarction detected on the brain CT/MRI
|
| Absence of extra- or intracranial atherosclerosis leading to ≥ 50% stenosis in the artery supplying the infarcted area (CTA/MRA/ultrasound) |
| Absence of a significant cardioembolic source (e.g., AFib, intracardiac thrombus, myxoma, etc.) |
| Absence of other specific causes of stroke (dissection, vasculitis, etc.) |
| Vascular imaging supporting embolic etiology |
|
- ESUS is associated with a higher recurrence risk, similar to that of cardioembolic stroke
[Ntaios, 2015]
- suspicion of thromboembolism is supported by:
- MR SWI findings [Gratz, 2014]
- histologic examination of material from mechanical recanalization, where the thrombus composition is similar in cardioembolic and ESUS patients
[Tobias Boeckh-Behrens, 2019]
- ESUS may be caused by unrecognized cardioembolic etiology (i.e., TOAST 2) or by embolization from non-stenotic plaques in the aorta and carotid artery (TOAST 1)
- paradoxical embolization (PFO) or other non-atherosclerotic causes are more common in individuals < 50 years of age
- paroxysmal AFib and atherosclerotic plaques predominate in those > 50 years of age
- paradoxical embolization (PFO) or other non-atherosclerotic causes are more common in individuals < 50 years of age
- a diagnosis of ESUS implies that the stroke is embolic in origin (given the non-lacunar characteristics of the ischemia)
- the source of the embolus is unknown after a thorough evaluation
- although cryptogenic stroke implies that the cause is unknown, the stroke is not necessarily embolic
- individuals diagnosed with ESUS have a cryptogenic stroke, but the reverse is not always the case
Cryptogenic stroke recurrence
- short-term risk of recurrent cryptogenic stroke is 1.6% at 7 days, 3-4.2% at 1 month, and 5.6% at 3 months (Lovett, 2004)
- patients with ESUS have a relatively high recurrence rate compared to other stroke subtypes (nearly 20% at 2 years) (Ntaios, 2015)
Management
- the mainstay of prevention of cryptogenic stroke (including ESUS) is antiplatelet therapy
- ASA or clopidogrel or short-term DAPT (ASA+CLP)
- ticagrelor is not recommended in this indication (negative posthoc analysis of ESUS patients in the SOCRATES trial) (AHA/ASA 2021 3/B-NR)
- DOACs are not recommended (AHA/ASA 2021 3/B-R)
- in younger patients with significant PFO and no other plausible cause of stroke, consider PFO occlusion
- in older patients, rigorously and repeatedly search for cardioembolic etiology (particularly paroxysmal AFib), as this would be an indication for anticoagulant therapy
- in a study that followed ESUS patients for up to 3 years, the rate of paroxysmal AFib was as high as 41.4%! [Kitsiou, 2021]
- use a long-term loop recorder or implantable device
- vascular risk factor management + lifestyle modifications are also essential
ESUS and anticoagulation
- randomized trials involving ESUS patients have yielded negative results so far ⇒ anticoagulation is not superior to ASA
- negative results of NAVIGATE ESUS trial with rivaroxaban 15 mg vs. ASA 100mg [Hart, 2018]
- however, a positive effect of rivaroxaban was found in the subgroup with moderate and severe left atrial enlargement – patients with left atrial diameter > 4.6 cm had 1.7% vs. 6.5%/year stroke risk (rivaroxaban vs. aspirin) [Healey, 2019]
- neutral results of the RESPECT-ESUS trial (ASA vs. dabigatran 110/150 mg) [Diener, 2019]
- negative results with apixaban in selected patients
- ARCADIA – apixaban vs. ASA in patients with atriopathy (characterized by higher ECG voltages, left atrial enlargement, and NT-proBNP>250 pg/L) – apixaban did not significantly reduce recurrent stroke risk compared with aspirin
- ATTICUS – apixaban vs. ASA in patients with additional risk factors (left atrial size > 45 mm, spontaneous echo contrast in the LAA, LAA flow velocity ≤ 0.2 m/s, CHA2DS2-VASc score ≥ 4, or PFO)
- ARCADIA – apixaban vs. ASA in patients with atriopathy (characterized by higher ECG voltages, left atrial enlargement, and NT-proBNP>250 pg/L) – apixaban did not significantly reduce recurrent stroke risk compared with aspirin


