ISCHEMIC STROKE / ACUTE THERAPY
Angiographic grading of cerebral revascularization
Updated on 06/11/2023, published on 03/03/2022
- revascularization is a broader term and includes:
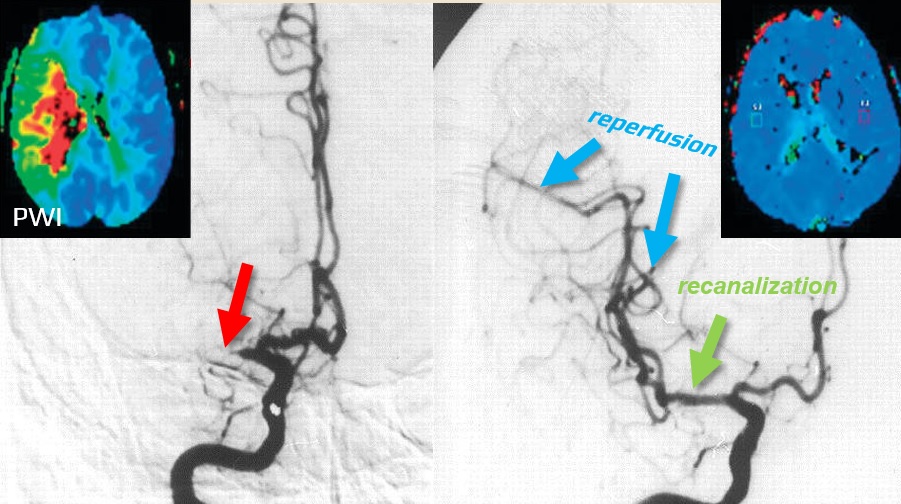
- recanalization (the removal of a clot from the target vessel)
- anterograde reperfusion (restoration of blood flow to the peripheral circulation)
- recanalization does not automatically mean reperfusion (if peripheral embolization persists, recanalization will have minimal or no clinical effect)
- reperfusion is a better marker of revascularization because it considers the state of the tissue and is, therefore, more closely related to the clinical outcome
- on the other hand, the quantification of recanalization is an essential parameter for evaluating the direct effects of an intervention
- upon the completion of each endovascular intervention, both recanalization (via AOL scale) and reperfusion (via mTICI scale) should be documented
- criteria of successful intervention: mTICI 2b-3 and AOL 2-3
- other scales have been introduced but are rarely used
- The Qureshi scale
- The Recanalization in Brain Ischemia (RBI) scale
- the Mori scale
| Revascularization | ||
|
Recanalization
|
restoration of flow in the occluded arterial segment (primary arterial occlusive lesion) |
AOL |
|
Reperfusion
|
restoration of flow in the territory of an occluded vessel (distal vascular bed) |
mTICI
|
Reperfusion assessment
Modified Treatment In Cerebral Infarction (mTICI)
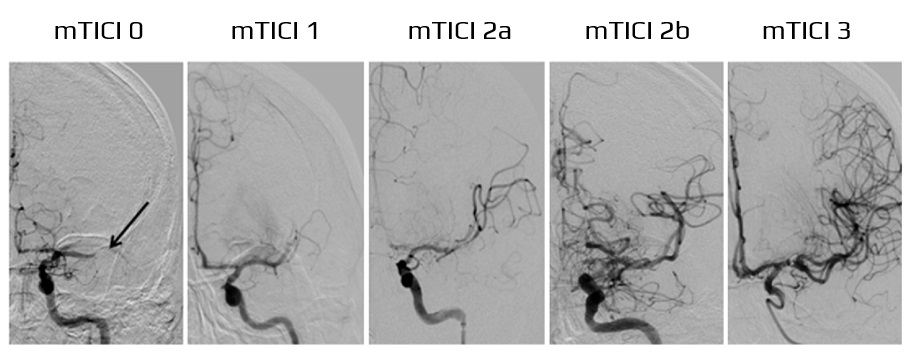
- the modified Treatment In Cerebral Infarction (mTICI) score specifies the extent of tissue perfusion; it was derived from the original TICI classification (Thrombolysis In Cerebral Infarction)
- the original name was changed to reflect the current endovascular practice better
- TICI 2 category was subdivided to distinguish between reperfusion in < 1/2 of the target vascular territory (mTICI 2a) and > 1/2 of it (mTICI 2b) [Zaidat, 2013]
- score has good interrater reliability and is a strong predictor of clinical outcomes
- mTICI has superior reproducibility and predictive value compared to the original TICI [Yoo, 2013]
Recanalization assessment
- recanalization scales evaluate the direct impact of therapeutic intervention on the Target Arterial Lesion (TAL)
- these scales do not directly assess downstream perfusion but may still provide additional prognostic information (residual stenosis increases the risk of reocclusion or distal embolization)
Arterial Occlusive Lesion (AOL) scale
- the Arterial Occlusive Lesion (AOL) scale is designed to measure the degree of recanalization at the TAL
- it is preferred for its ease of use and accurate assessment of device effectiveness at the occlusion site
- AOL categorizes arterial patency based on the degree of luminal opening (none, partial, or complete)
- further qualification is made based on the presence (grades 2 or 3) or absence (grades 0 or 1) of downstream flow
- it is preferred for its ease of use and accurate assessment of device effectiveness at the occlusion site
- there is a good correlation between AOL and mTICI, as well as an excellent ability to predict the outcome
- however, assessing target arterial lesion (TAL) may be problematic (see below)
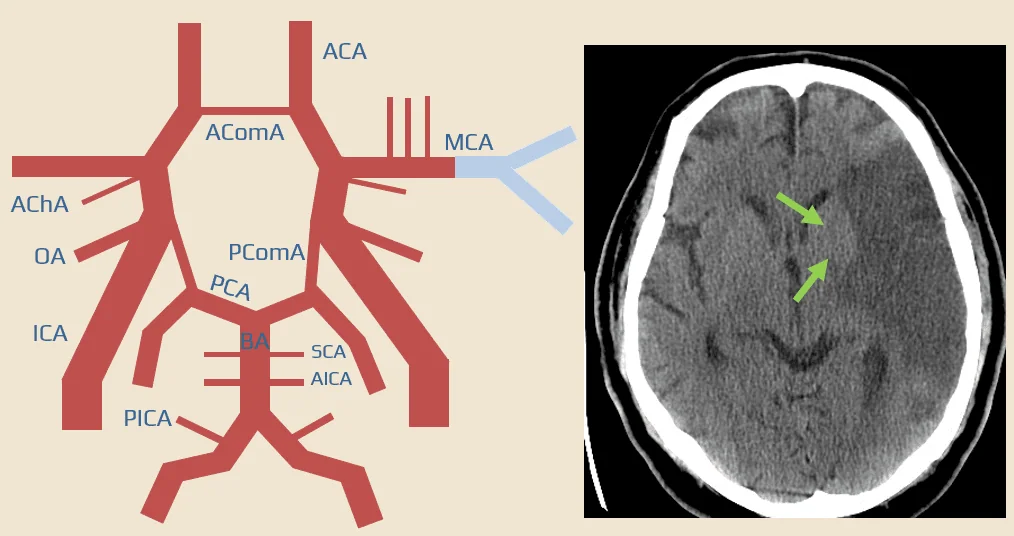
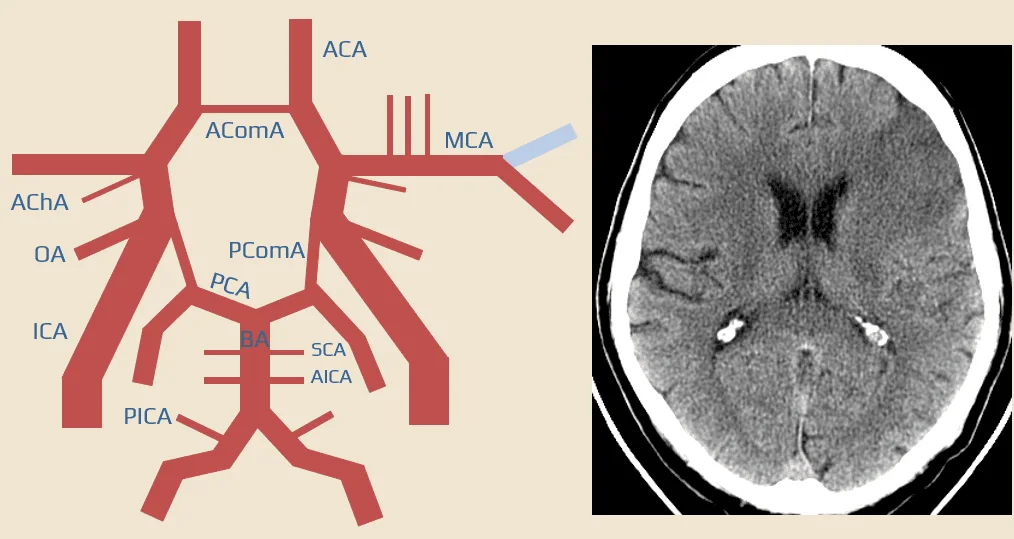
- for example, in a tandem lesion involving the ICA+M1, recanalization of the siphon with persistent M1 occlusion may yield conflicting assessments – AOL 3 / mTICI 0
- it would be better to evaluate the whole thrombus, although determining its distal end poses a problem.
- differentiating between partial recanalization with residual intraluminal thrombus and underlying intracranial atherosclerotic stenosis presents another challenge
- TAL = most proximal part of the intracranial occlusion
- except for isolated extracranial artery occlusion (e.g., ICA occlusion with distal hypoperfusion)
- in cases of combined occlusion involving the cervical segment of ICA+ M1, the target artery is the MCA
| ICA | MCA |
|
|