ISCHEMIC STROKE / CLASSIFICATION AND ETIOPATHOGENESIS
Temporal arteritis
Updated on 31/01/2024, published on 13/05/2023
- temporal arteritis (TA), also known as giant cell arteritis (GCA), is a systemic inflammatory vasculitis of medium and large-sized arteries that primarily affects elderly adults
- the temporal artery is most commonly involved
- aorta and the subclavian, iliac, ophthalmic, occipital, and vertebral arteries can be affected too
- it is more common in women and mostly affects individuals over the age of 50
- the most prominent symptoms are headaches, jaw claudications, and visual disturbances (ischemic optic neuropathy – ION)
- if untreated, it can result in severe complications (most usually blindness)
- TA is sometimes associated with polymyalgia rheumatica (both entities are considered a continuum of a pathological process and temporal arteritis is a sign of advanced inflammation)
Etiopathogenesis
- large and/or medium-sized artery inflammation
- external carotid artery (ECA) and its branches (superficial temporal artery – STA) are most commonly involved
- ICA and intracranial segments or other major arteries are rarely affected
- the exact cause is unknown; several risk factors have been identified
- age – rarely affects those under 50; most patients are between 70 and 80
- sex – women have double risk
- race and geographic region – more common among white people in Northern European populations
- polymyalgia rheumatica – having polymyalgia rheumatica increases the risk of developing temporal arteritis
- family history
- histology
- vessel involvement is segmental, with narrowing or even obliteration of the vessel lumen
Clinical presentation
General symptoms
- general symptoms are dominated by anorexia, weight loss, fever (~15%), night sweats, depression, fatigue
- frequent headache (40-90% of patients; may be severe)
- elevated inflammatory markers (CRP, ESR)
- myalgia, stiffness in the neck, shoulders, or hips (related to polymyalgia rheumatica, which may be present in up to 50% of cases)
Local findings
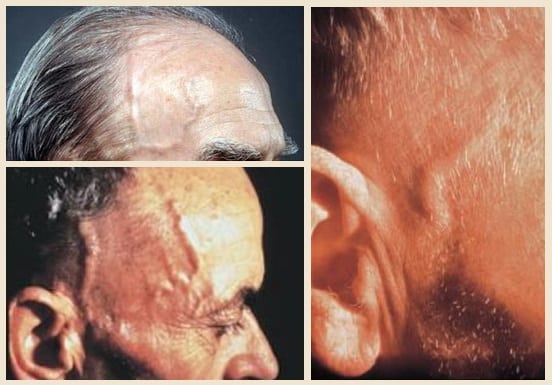
- scalp tenderness, pain, and tenderness over the temples; the skin may appear red
- the temporal artery is swollen and sensitive to palpation, with absent pulsation
- palpable nodules may be present
- sometimes arteritis may be occult, and the initial symptoms are headache and unilateral blindness
Symptoms of ischemia
- involvement of the ECA
- pain when speaking and/or chewing (jaw claudication)
- ophthalmic artery, cilliary arteries, and central retinal artery (CRA) involvement presenting with loss of vision
- ischemic optic neuropathy (ION)
- anterior x posterior
- amaurosis fugax
- retinal exudates
- oculomotor nerve palsy (CN III) with diplopia
- ischemic optic neuropathy (ION)
- ICA, VA involvement (stroke or TIA) – rare
Diagnostic evaluation
- local findings that are evident on clinical examination (inspection, palpation) are described above
Diagnostic criteria
- if there is a reasonable clinical suspicion, it is not advisable to delay treatment
- the rapid improvement of subjective symptoms after the start of corticosteroid therapy becomes an important diagnostic criterion (in other autoimmune diseases, the improvement is not so rapid and significant)
| Diagnostic criteria In the presence of 3 out of 5 criteria, the sensitivity is ~ 93% |
|
|
Differential diagnosis
- in the presence of myalgia, consider polymyalgia rheumatica
- other vasculitides
Management
Causal (immunosuppressive) therapy
- immediate treatment initiation is crucial in suspected temporal arteritis to prevent vision loss, even before biopsy confirmation
- high-dose corticosteroids are the first choice and may be combined with immunosuppressive drugs (combination allows lower maintenance doses of corticosteroids)
- a high initial dose of steroids helps to control symptoms quickly
- subsequent lower dose given over a longer period should prevent relapse
- precautions are needed for long-term use of corticosteroids to avoid side effects
- a high initial dose of steroids helps to control symptoms quickly
- treatment duartion is guided by the clinical course and CRP/ESR levels
- ESR decline is usually rapid, sometimes with a latency of 3-5 days
Without vision loss
- PREDNISONE
- recommended initial dose is 20-40mg daily for 4-8 weeks
- subsequently, a gradual tapering regimen should be initiated, reducing the dose by 5 mg every 4 weeks until reaching a daily dose of 10 mg
- keep the maintenance dose of 5-10 mg prednisone daily for a minimum of 12 months
- steroids may be discontinued if the patient is asymptomatic and inflammatory markers are normal after a 12-month maintenance period
- the overall duration of treatment typically ranges from 3 to 4 years
- this approach aims to balance the therapeutic benefits of prednisone with minimizing potential side effects associated with long-term use
Vision loss
- PREDNISONE
- initial dose 60-80mg daily for 4-8 weeks
- then gradually reduce the dose to 20 mg
- then proceed as in the uncomplicated form to 5-10mg daily (or 5 and 10 mg every other day)
- METHYLPREDNISOLONE
- start with pulse therapy – 1g/day for 3-5 days
- concurrent administration of H2-blockers or PPI and potassium is required
- then switch to oral medication (PREDNISONE 60-80 mg daily)
- maintain the high dose for several weeks before tapering
- it is not clear whether PO or parenteral therapy is better for stroke prevention (AHA/ASA 2021)
- “steroid-sparing” agents aid in steroid tapering, help prevent relapse of temporal arteritis and reduce steroid-related adverse events in the subacute phase
- immunosuppressants (azathiprine, methotrexate, cyclophosphamide)
- may also be used when corticosteroids are not tolerated or are found to be ineffective
- monoclonal antibodies can be used in resistant forms
- tocilizumab seems effective in corticosteroid-resistant AAION (FDA approval in 2017)
- no effect of infliximab has been demonstrated (AHA/ASA 2021 3/B-R)
- immunosuppressants (azathiprine, methotrexate, cyclophosphamide)
- lifelong use of low-dose corticosteroids may be necessary in some cases
- regular monitoring is essential
Prevention of ischemia
- antiplatelet therapy (ASPIRIN 100mg daily) to reduce the risk of a stroke or heart attack
Complications
- unilateral vision loss (rarely bilateral); may be permanent
- aortic aneurysm – this complication can develop even years after GCA diagnosis; annually monitor the aorta with chest X-rays or other imaging tests (ultrasound or CT)
- stroke – an uncommon complication of GCA