ADD-ONS / GENERAL NEUROLOGY
Capsular warning syndrome
Updated on 25/07/2024, published on 01/03/2024
Introduction
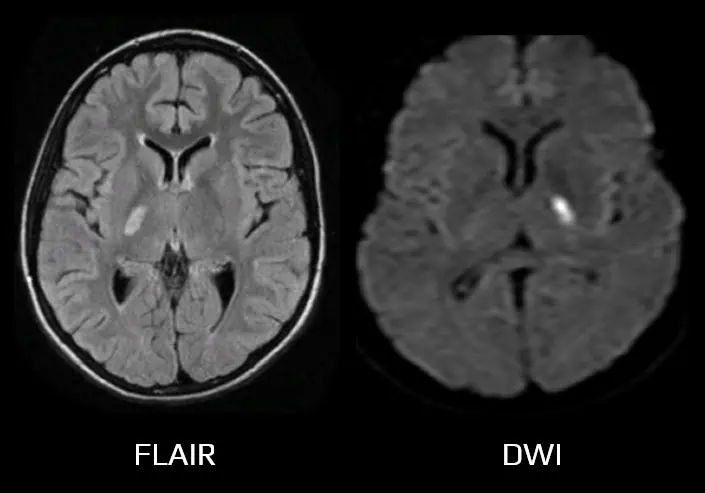
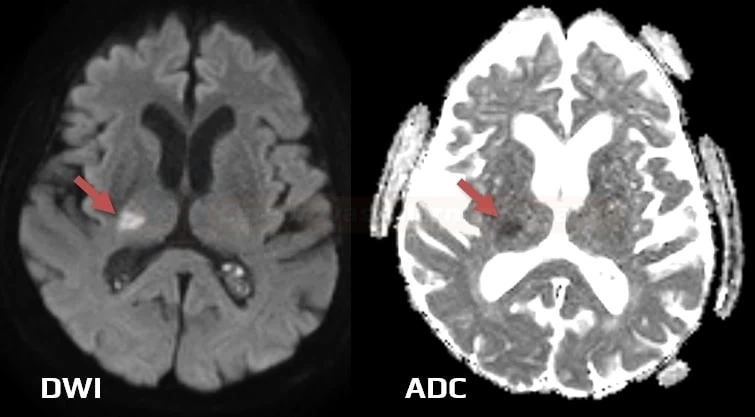
- internal capsule syndrome is characterized by disruption of the vertical connection between the cerebral cortex and subcortical structures
- the term Capsular Warning Syndrome (CWS) is defined by at least three stereotyped episodes of motor lacunar syndrome (MLS) or sensorimotor lacunar syndrome (SMLS) within 24 hours, with complete recovery between episodes, which involves two of three body parts (face, arm, or leg) or more, without cortical symptoms
- varying time intervals can be found in the literature – 24, 48, 72 hours, or even 7 days
- CWS is associated with a high risk of subsequent stroke with a permanent deficit
- the 7-day risk of stroke after CWS may be as high as 60-80% (He, 2019)
- hypertension and dyslipidemia are the most common risk factors, as is typical for lacunar stroke in general
- capsular-warning syndrome (CWS) and stuttering lacunar syndrome (SLS) are both associated with transient neurological deficits (TIAs) related to small vessel disease
- CWS specifically involves the internal capsule, while SLS may affect various deep structures supplied by perforating arteries (thalamus, pons, basal ganglia, etc.)
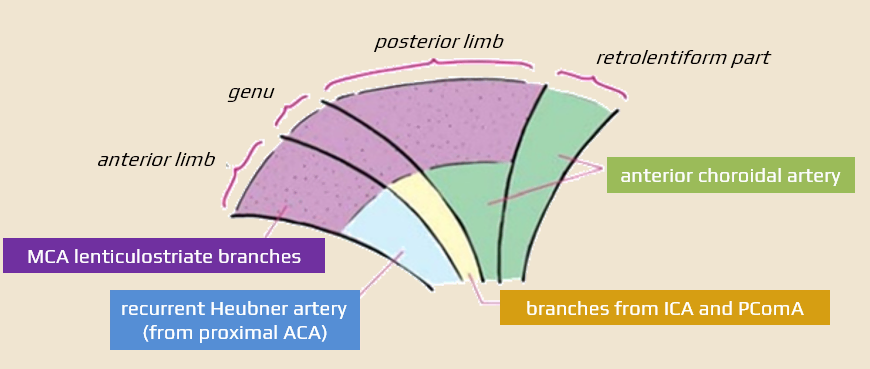
Anatomic notes
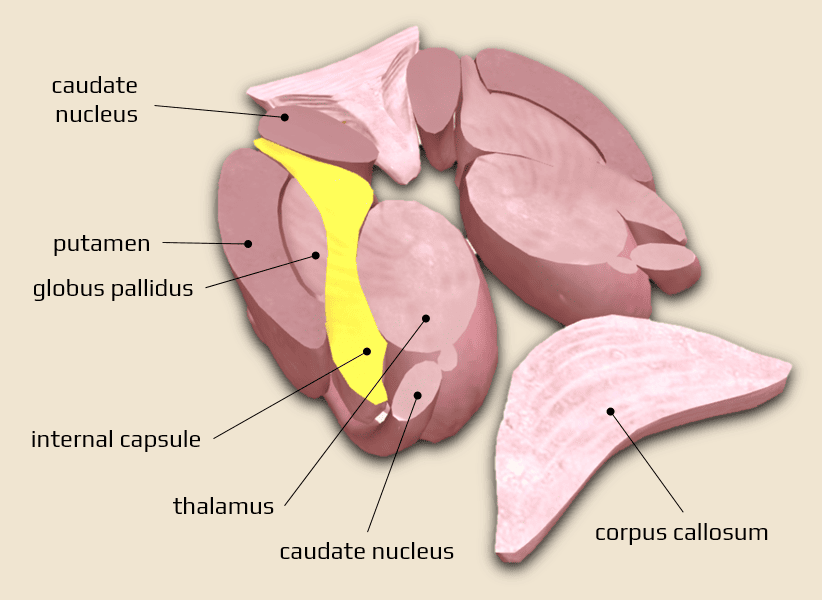
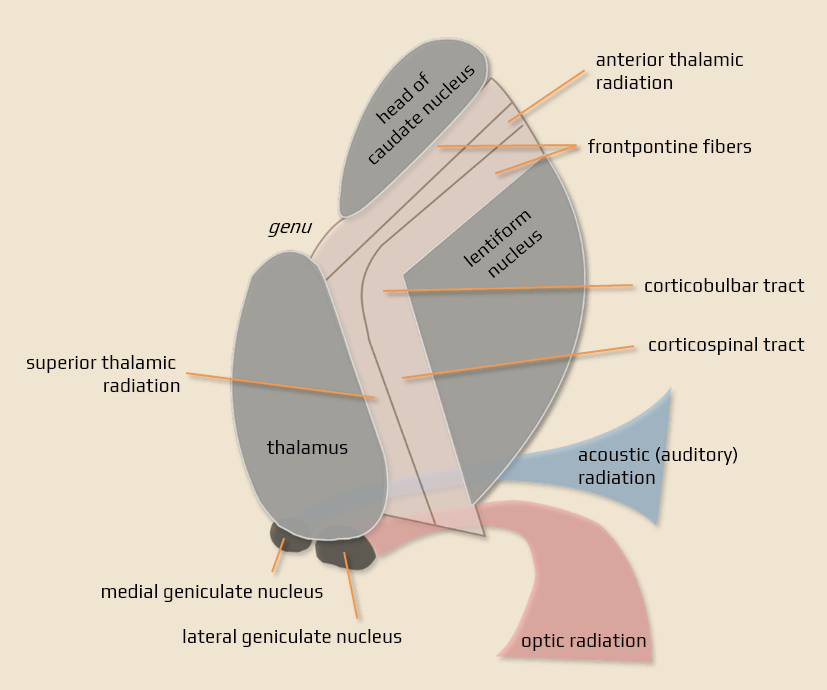
- internal capsule consists of cortical centripetal and centrifugal pathways located between the thalamus and basal ganglia
- anterior limb (crus) – located between the head of the caudate nucleus and the lentiform nucleus – fronto-pontine pathways
- genu – cortico-nuclear pathways (for facial muscles)
- posterior limb (crus) – between the thalamus and lentiform nucleus – cortico-spinal (for limb and trunk muscles), cortico-rubral and cortico-reticular tracts
- retrolentiform part – extended part dorsal to the lentiform nucleus
- parieto-occipito-pontinne tract
- optic radiation
- acoustic (auditory) radiation
- each part contains fibers connecting the thalamus and cortex – the anterior (frontothalamic pathway), superior, and posterior thalamic radiations
Vascular supply of the internal capsule
Clinical presentation
General clinical presentation of internal capsule lesions
Anterior limb (crus)
- inappropriate laughter and crying (fronto-thalamic pathways)
- pseudocerebellar syndrome (fronto-ponto-cerebellar pathways)
Genu and posterior limb
- contralateral hemiplegia (hemiparesis) incl. CN VII and (corticonuclear and corticospinal tracts) – typical spastic Wernicke-Mann posture in the chronic stage
- hemianesthesia (hemihypesthesia) – lesion of thalamocortical pathways for superficial and deep sensation
- hemiataxia (thalamoparietal pathways)
- hemianopia (visual pathway)
- combination of motor, sensory deficits, and hemianopia may mimic hemispheric lesions (LVO occlusion) ⇒ DDx of anterior choroid artery occlusion vs. MCA occlusion
Bilateral internal capsule lesion
- bilateral lesions (usually as part of status lacunaris) lead to quadriparesis and pseudobulbar palsy
Characteristics of Capsular Warning Syndrome (CWS)
- CWS is characterized by at least three stereotyped episodes of lacunar syndrome within 24 hours (or up to 7 days)
- sensorimotor and motor lacunar syndromes are the most common
- the onset of symptoms is abrupt
- the duration of each episode varies (usually within 2-50 minutes)
Etiopathogenesis
- the exact pathophysiological mechanism of the symptom fluctuation remains unclear
- probably caused by the arteriolosclerosis of small-penetrating vessels and intermittent hemodynamic changes secondary to structural arterial changes and/or hypertension (Ladeira, 2017)
Diagnostic evaluation
- a standard etiologic diagnostic workup is required
- however, the most probable cause is small vessel disease (TOAST 3)
Management
- the most effective treatment of CWS remains unclear; it is also unclear how effectively current treatment can stop or prevent fluctuations in stuttering lacunar syndromes
- intravenous thrombolysis (IVT) should be administered to all eligible patients
- patients presenting with disabling symptoms within the therapeutic time window
- intravenous thrombolysis is safe for CWS patients (He, 2019)
- aspirin +/- clopidogrel when IVT is not an option
- DAPT (ASA+CLP) shows promising results in this setting (Barberich, 2019) (Asil, 2012) (Hawkes, 2019)
- initiate strict management of vascular risk factors, particularly arterial hypertension and dyslipidemia