ISCHEMIC STROKE / CLASSIFICATION AND ETIOPATHOGENESIS
Marfan syndrome
Updated on 07/11/2023, published on 09/05/2023
- Marfan syndrome is an inherited connective tissue disorder
- individuals with Marfan syndrome are typically tall and thin, with unusually long arms, legs, fingers, and toes; the condition may become life-threatening due to aortic involvement
Etiopathogenesis
- inherited connective tissue disease
- familial form (75%)
- sporadic form (25%)
- autosomal dominant (AD) inheritance, many mutations were reported
- FBN1 gene (15q15-q21.1) and FBN2 gene (5q23-q31) – encode fibrillin
- TGFBR2 (transforming growth factor-beta receptor 2) gene, locus 3p22
- TGFBR1 gene, locus 9q22
- predominant involvement: skeletal, ocular, and cardiac; vascular involvement is characterized by altered tunica media
Mutations in the FBN1 gene cause connective tissue to be weaker. It is also believed that mutated fibrillin does not control the excess TGFB, and its increased activity leads to pathological changes in various body organs. This regulatory role is also impaired in the case of mutations in TGFBR1 and TGFBR2 mutations
Clinical presentation
Neurovascular symptoms
- Marfan syndrome predisposes individuals to certain cardiovascular complications that could lead to stroke:
- aortic dissection extending to supra-aortic arteries (mechanical occlusion ± peripheral embolization)
- dissection of cerebral arteries
- cardioembolism (due to valvular dysfunction, arrhythmias including AFib)
- (pseudo) aneurysm formation (⇒ rupture or embolization from the sac)
- intracranial aneurysms are less common compared to other connective tissue disorders
- pseudoaneurysms occur after dissection
Cardiovascular symptoms
- common cause of fatal complications (cause of death in up to 90%)
- dilation (up to 80%) or dissection of the ascending aorta [Hwa, 1993]
- incipient dilatation is often seen by the end of the first decade of life
- incipient dilatation is often seen by the end of the first decade of life
- frequently accompanied by aortic regurgitation, mitral valve prolapse, and dilatation of the pulmonary artery
Skeletal malformations
- tall figure
- long, thin limbs
- hypermobile joints
- thumb sign – thumb extends beyond the ulnar edge of the hand when fingers are clenched into a fist
- wrist sign – thumb extends beyond index finger when the wrist is grasped
- scapula alata
- pectus carinatum or excavatum
- pes planus
- arachnodactyly
- scoliosis and other spinal deformities
- dolichocephaly
Ophthalmologic symptoms
- lens ectopia (dislocation) – in up to 50% of cases, typically bilateral
- myopia – high-degree myopia is common due to elongation of the eyeball
- retinal detachment
- secondary glaucoma
- cataract (may develop at an earlier age, especially following lens surgery)
- corneal flatness
- astigmatism (irregular shape of the cornea or lens leading to blurred or distorted vision)
Diagnostic evaluation
- the diagnosis is established based on a combination of thorough clinical evaluation, family history, and imaging ⇒ see diagnostic criteria
- typical clinical presentation
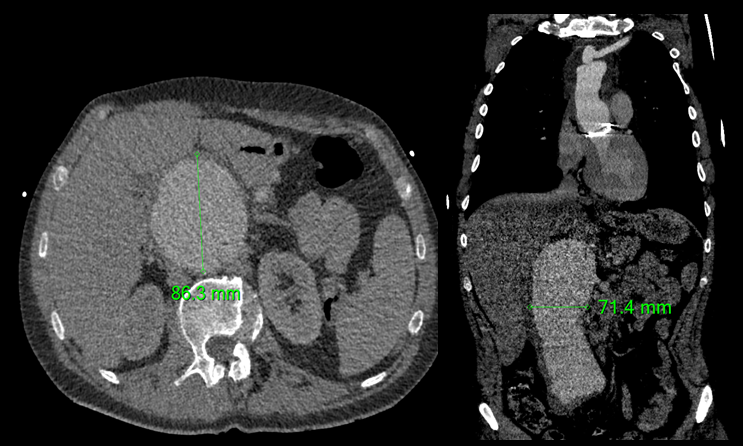
- cardiovascular imaging (TEE, CTA, MRA) – dilation of the aortic root, as well as the ascending and descending aorta
- skeletal imaging
- ophthalmologic exams to evaluate the lens and retina
- genetic testing
- exclude other conditions such as:
- homocystinuria (mental retardation is common)
- Ehlers-Danlos syndrome
- Shprintzen Goldberg syndrome
- Loeys-Dietz syndrome
| Diagnostic criteria for Marfan syndrome (Ghent criteria) |
| Negative family history |
|
| Positive family history |
|
Management
- causal therapy is not available; management is aimed at mitigating and monitoring the myriad manifestations
- continuous follow-up with a multidisciplinary team (including a cardiologist, ophthalmologist, orthopedist, and genetic counselor) ensures optimal management of all aspects of Marfan syndrome
- cerebrovascular management
- standard stroke treatment and prevention
- aortic dissection remains one of the absolute contraindications to IVT!
- cardiovascular management
- beta-blockers to reduce aortic wall stress by lowering blood pressure and heart rate
- angiotensin II receptor blockers (ARBs) may also be used
- periodic imaging to monitor aortic dimensions and valve function
- prophylactic aortic root replacement in cases of significant aortic dilatation to prevent dissection
- ocular management
- periodic ophthalmologic examinations are crucial for early detection and management of ocular symptoms to prevent vision loss and improve the quality of life
- manage myopia, astigmatism, or lens dislocation
- skeletal management
- physical therapy and orthotic devices to manage musculoskeletal symptoms
- surgery for severe spinal deformities
- pain management with appropriate analgesics for musculoskeletal discomfort
- genetic counseling
- family risk assessment + discussion of reproductive options (pregnancy is usually not recommended)
- lifestyle modifications
- avoidance of high-intensity and contact sports to prevent arterial dissection and skeletal injuries
- healthy lifestyle maintenance, including a balanced diet and regular, low-intensity exercise