CONSEQUENCES OF STROKE
Vascular cognitive impairment (VCI)
Updated on 23/06/2024, published on 15/12/2023
- cerebral vascular disease can lead to the development of cognitive deficit (VCI) or vascular dementia (VaD), and it also influences the course of other dementias (AD)
Definition
- Vascular Cognitive Impairment (VCI) is a term used to describe a range of cognitive deficits resulting from cerebrovascular disease or other conditions that affect cerebral blood vessels
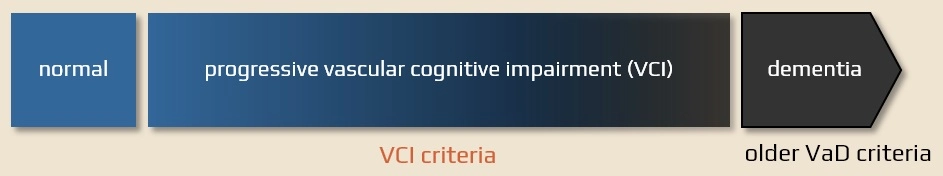
- it is currently preferred over vascular dementia (VaD) because classic criteria for dementia may not be present for a long time (dominant memory impairment + global and progressive impairment + noticeable functional
- the key features include:
- cerebrovascular disease – VCI is primarily associated with damage to the brain’s blood vessels, often due to conditions like stroke, small vessel disease, or other vascular disorders
- heterogenous cognitive deficits
- a wide range of cognitive changes that can vary in severity, from mild cognitive impairment (MCI) to more severe forms of cognitive impairment, including those meeting the criteria for dementia
- deficits occur in various domains, including memory, executive function, attention, language, and visuospatial skills
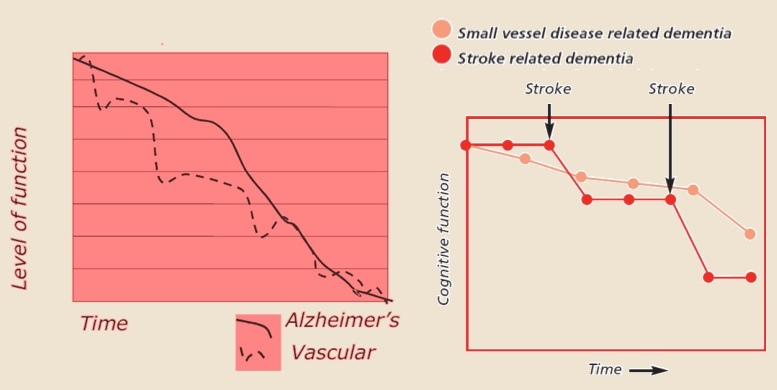
- course – VCI lacks a consistent clinical presentation and course (unlike, for example, Alzheimer´s disease)
- deficits may progress over time and lead to the development of vascular dementia
- presence of traditional vascular risk factors
- early detection and management of vascular risk factors are crucial for reducing the incidence and progression of VCI
Epidemiology
- VCI is one of the most common types of cognitive impairment, second only to Alzheimer’s disease (AD)
- the prevalence and incidence vary by geographic region and population (ethnicity, genetics); VCI is believed to be underdiagnosed, and it often coexists with other forms of dementia, such as Alzheimer’s disease. This can make it challenging to estimate its true prevalence accurately
- advanced diagnostic techniques, such as neuroimaging and CSF analysis, may help in distinguishing VCI from other forms of dementia
- it is more common in older adults
- the risk of dementia in patients after stroke is 5-fold compared to the healthy population of the same age
- individuals with a history of multiple strokes are at highest risk
- patients have a lower 5-year survival rate compared to the healthy population (39% versus 75%)
- cardiovascular and cerebrovascular diseases are the leading cause of premature death
Risk factors
- traditional cardiovascular risk factors
- most significant are:
- age
- diabetes mellitus
- undiagnosed or poorly controlled arterial hypertension
- hypercholesterolemia
- smoking
- atrial fibrillation
- a history of cerebrovascular events
Classification
- different classifications often use different designations for the same clinical entities
Diagnostic evaluation
Neuroimaging
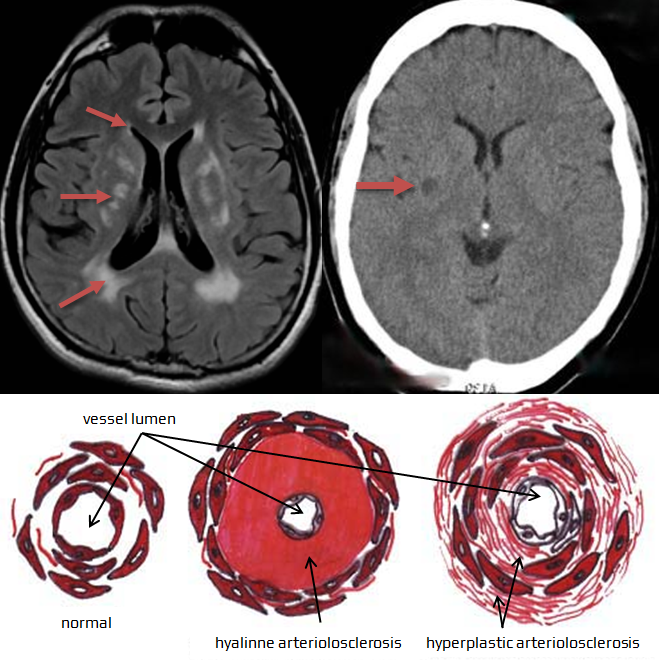
- brain CT or better MRI + vascular imaging with a demonstration of relevant vascular damage
Clinical evaluation
- to distinguish AD, a color perception test (Ishihara charts) could help – in AD, color perception is impaired
- sensitivity of 80.6%, a specificity of 87.5% for a cut-off value of 32.5 [Arnaoutglou, 2017]
Psychological evaluation and tests
- the purpose of any screening is to roughly differentiate between normal and pathological conditions; the results may be further refined through specialized neuropsychological testing
- in practice, the most commonly used screening tool is the Mini-Mental State Examination (MMSE)
- It is a brief and relatively easy-to-evaluate test, but it is important to ensure that it is administered correctly
- when used alone, it has limited diagnostic value regarding the nature of cognitive deficit
- It is not sensitive to executive function impairments (which are common in VCI) – It is advisable to include at least the Clock Drawing Test (CDT)
- It is a brief and relatively easy-to-evaluate test, but it is important to ensure that it is administered correctly
- during specialized examinations, it is important to consider the patient’s current capabilities and the increased fatigue of cognitively impaired patients. Adjust the testing duration and the selection of tests accordingly
|
Examples of neuropsychological testing methods suitable for detecting cognitive function decline
|
|
|
Intellect (global status)
|
Wechsler Intelligence Tests (WAIS-R, or WAIS-III)
|
|
Memory
|
Wechsler Memory Scale (WMS-III)
Rey-Osterrieth Complex Figure |
|
Executive abilities
|
Trail Making Test – Part B
Stroop Test Cognitive Estimation Test Wisconsin Card Sorting Test |
|
Language
|
Verbal Fluency Tests
Token Test alternatively, Western Aphasia Battery |
|
Visuospatial and constructional abilities
|
|
|
Psychomotor speed
|
Symbols from WAIS-R
Trail Making Test – Part A |
|
Attention
|
Trail Making Test – Part A
Repeating Numbers from WAIS-R |
|
Symbolic abilities
|
Reading, counting, writing + drawing a person
|
|
Emotionality and depression
|
Beck Depression Inventory
|
|
Behavior
|
Instrumental Activity of Daily Living
Neuropsychiatric Inventory Neurobehavioral Rating Scale |
Diagnostic criteria
Pitfalls of existing criteria
- diagnostic criteria for vascular dementia were based on the model of cognitive changes in Alzheimer’s disease (AD), with dominant damage to the hippocampus and, therefore, memory. However, vascular disease can lead to widespread cognitive deficits, while memory may remain intact
- the course may not be a distinguishing factor either – not all vascular cognitive deficits progress in a stepwise manner. For example, subcortical ischemic disease has a course that is more similar to AD, but clinically, it is characterized by a predominance of executive dysfunction rather than memory impairment
- it is questionable whether it is even possible to create universally applicable diagnostic criteria for a condition with a broad etiopathogenic basis and diverse clinical presentations
- some experts, therefore, prefer to create diagnostic criteria for individual subtypes of VCI (see, for example, the diagnostic criteria for subcortical ischemic disease proposed by Erkinjuntti)
Hachinski ischemic score (HIS)
Hachinski Ischemic Score (HIS)
- a simple and easy-to-use tool used since 1974 for a rough differentiation between multiinfarct dementia and Alzheimer’s dementia, but it is not suitable for distinguishing mixed forms
- a higher score is generally indicative of a higher likelihood of vascular dementia
- 0-4 points – suggestive of Alzheimer’s dementia
- 7 or more – suggestive of Vascular Dementia (VaD)
| abrupt onset of dementia | 1 |
| stepwise progression of dementia | 1 |
| fluctuating cognitive symptoms (symptoms vary in severity from day to day) |
1 |
| nocturnal confusion | 1 |
| relative preservation of personality despite cognitive impairment | 0 |
| emotional incontinence (outbursts or tearfulness) | 1 |
| gait disturbance | 1 |
| history of one or more strokes | 1 |
| hypertension | 1 |
| evidence of multi-infarct dementia on CT or MRI | 1 |
NINDS-AIREN criteria
- these criteria were created specifically for research purposes (highly specific, but with low sensitivity)
- to establish a diagnosis of probable VCI according to the NINDS-AIREN criteria, three fundamental conditions must be met:
- presence of cognitive deficit – defined as a decline in memory and two or more other cognitive abilities.
- existence of corresponding cerebrovascular brain damage (on imaging methods):
- multiple territorial infarcts or hemorrhages
- strategically located single infarct.
- extensive white matter involvement
- multiple lacunar infarcts in the basal ganglia and white matter
- causal relationship between the two above-mentioned conditions:
- for example, the onset of cognitive deficit within 3 months after a recognized stroke
- sudden deterioration of cognitive functions or gradual progression of cognitive deficit with progressive findings on imaging examinations
- definitive (certain) diagnosis of vascular dementia is established when the criteria for probable vascular dementia are met, there is histopathological evidence of cerebrovascular brain disease (from biopsy or autopsy), and other causes of dementia have been ruled out.
- on the other hand, the vascular etiology is questioned in cases of early onset and progressive worsening of memory deficits and other cognitive abilities in the absence of corresponding lesions on CT or MR
| NINDS-AIREN Diagnostic Criteria |
I. Possible
II. Probable
III. Definite – histopathological evidence |
Classification of Subcortical Ischemic Vascular Dementia/Disease (SIVD)
- I. Cognitive deficit
- executive dysfunction
- memory impairments (especially retrieval difficulties)
- II. Cerebrovascular disease (CVD)
- typical CT or MRI findings (see table)
- neurological deficit
-
“frontal” gait, pyramidal, and pseudobulbar syndrome
-
- onset between 44-75 years
- history of arterial hypertension, diabetes (often subclinical)
- progression over 5-10 years
| CT/MRI criteria of SIVD |
|
Management
- early detection is crucial as it can help in managing underlying conditions and potentially slow or stop the progression of cognitive decline
Causal therapy of cerebrovascular disease
Symptomatic therapy
Cholinesterase Inhibitors and NMDA Antagonists
- studies have demonstrated the effectiveness of cholinesterase inhibitors and NMDA receptor antagonists
- donepezil, galantamine, rivastigmine
- memantine
- they slow the progression of cognitive deficit, have a positive effect on behavioral and psychological symptoms of dementia (depression, anxiety, etc.), and on the performance of daily activities
Treatment of associated depression → poststroke depression
Other medications
- the effect of other drugs (e.g., nootropics, extracts from ginkgo biloba) has not been convincingly demonstrated by studies, but it cannot be ruled out
Cognitive training, psychotherapy, rehabilitation, caregiver support, diet → Stroke rehabilitation
- training tailored to the specific deficits that the individual patient is experiencing
- a diet rich in fish, seafood, vegetables, citrus fruits, and olive oil, as well as a diet high in folic acid, vitamins B6 and B12, and antioxidants
FAQs
- a cognitive decline that ranges from mild cognitive impairment to more severe dementia
- primarily caused by vascular problems (atherosclerosis, arteriolopathy, etc.) that alter blood flow and lead to brain damage (ischemia or hemorrhage)
- symptoms vary but often include difficulties with problem-solving, focusing, organizing thoughts, and memory
- changes in mood, such as depression, and physical symptoms, like difficulty walking, can also occur
- vascular dementia is a more severe form of VCI; while VCI can range from mild to severe, vascular dementia specifically refers to cases where cognitive impairment is global and interferes with daily living
- diagnosis involves a medical history review, neurological exams, cognitive tests, and brain imaging studies
- No, they are different. Alzheimer’s is primarily caused by neurodegenerative processes, while VCI is due to blood flow issues in the brain. However, symptoms can overlap, and a person can have both conditions.
- treatment focuses on managing the underlying vascular conditions, slowing progression, and alleviating symptoms
- this includes controlling vascular risk factors (blood pressure, cholesterol levels, lifestyle changes like diet, exercise, etc.)
- early detection is crucial as it allows for early treatment of underlying conditions and potentially slows the progression of cognitive decline