ADD-ONS
Pseudotumor cerebri
Updated on 16/03/2024, published on 15/03/2024
Definition
- pseudotumor cerebri (idiopathic intracranial hypertension – IIH) is a clinical condition characterized by an increase in intracranial pressure without evidence of intracranial space-occupying lesion, infection, hydrocephalus, or other demonstrable cause
- the term benign intracranial hypertension is not appropriate as the condition can lead to vision loss in some patients
- idiopathic intracranial hypertension – IIH is reserved for patients with NO demonstrable cause
- imaging may reveal conditions (e.g., dural sinus stenosis, VJI compression) that are either causative or aggravate the symptoms; in such patients, the term pseudotumor cerebri or secondary intracranial hypertension should be used instead of IIH
- the diagnosis of IIH is based on the following criteria:
- subjective and objective signs of increased intracranial pressure
- bilateral papilledema
- increased CSF pressure (>250 mm H20 measured in the supine position)
- normal neurological findings (except for CN VI involvement)
- exclusion of space-occupying lesions or other obvious etiology on neuroimaging
- subjective and objective signs of increased intracranial pressure
- pseudotumor cerebri is a diagnosis by exclusionem
- in addition to headache, visual disturbances may occur – these are initially reversible with adequate therapy, but with a prolonged course, vision loss may become permanent
Epidemiology
- the approximate incidence of this disease in the general population is 0.5 – 1.7/100,000 per year
- the disease is probably more common than statistics indicate, as many patients are oligosymptomatic and resolve without treatment
- affects patients of all ages but most commonly occurs in young, obese women (Bezerra, 2018)
- pseudotumor cerebri is rare in the pediatric population (usually in the 12-17 year age group)
Etiopathogenesis
- the exact cause is unknown (as its name implies), but it is associated with some diseases or the use of certain drugs
- it is necessary to distinguish secondary forms of intracranial hypertension
- the increase in intracranial pressure is a consequence of, e.g., scarring after previous meningitis or subarachnoid hemorrhage, obstruction of cranial venous drainage in venous thrombosis, etc.
- proposed mechanisms:
- reduced CSF absorption (as evidenced by the findings of radioisotope cisternography and other studies)
- reduced venous outflow from the brain due to truncal obesity (due to an increase in intra-abdominal pressure and an increase in cardiac filling pressure)
- stenosis in the venous system is increasingly recognized as an important factor
- it is not entirely clear whether it is the primary cause or whether it is a potentiating factor
- the efficacy of venous stenting suggests a causal link
- most common risk factors:
- obesity/weight gain
- female gender, pregnancy, menstrual cycle irregularities, and their hormonal treatment or use of oral contraceptives
- termination of corticosteroid therapy
- treatment of acne with tetracycline and its derivatives and/or vitamin A or its analogues
- obesity
- postthrombotic conditions
- hematological disorders
- sideropenic anemia
- hypercoagulable states
- systemic diseases
- systemic lupus erythematosus (SLE)
- chronic renal failure
- sarcoidosis
- AIDS
- Behcet’s disease
- systemic lupus erythematosus (SLE)
- disorders of vitamin A metabolism
- “empty sella” syndrome
- pharmacological treatment
- tetracyclines
- indomethacin
- amiodarone
- thyroid hormones
- lithium
- growth hormone
- discontinuation of corticosteroid therapy
- endocrine conditions
- adrenal insufficiency
- Cushing disease
- hypothyroidism
- hypoparathyroidism
- pregnancy
Clinical Presentation
- headache (90%) with dizziness, occasional nausea, and vomiting
- headache lacks specific features, and commonly resembles migraine or tension type headache
- it tends to be more severe on awakening
- headache is more intense in the supine position and during Valsalva maneuver
- visual disturbances
- transient, brief episodes of blurred vision
- visual field disturbances in advanced stages
- pulsatile tinnitus (in ~ 60%)
- eye pain
- objective findings:
- papilledema
- typically bilateral but rarely unilateral or even absent
- initially, only a slight blurring of the disc margin is seen
- when the congestive papilla is fully developed, the borders of the papillae are completely obliterated
- distinguishing congestive papillae from other affections causing target edema can be difficult in some cases (pseudopapilledema)
- neurological examination is usually normal, except for visual field deficit or abducens nerve palsy (bilateral in ~ 10-20% of cases)
- papilledema
- typically, the patient appears well despite significant papilledema
Diagnostic evaluation
- brain CT or better MRI + CTV/MRV exclude space-occupying lesions, venous sinus thrombosis, hydrocephalus, etc.
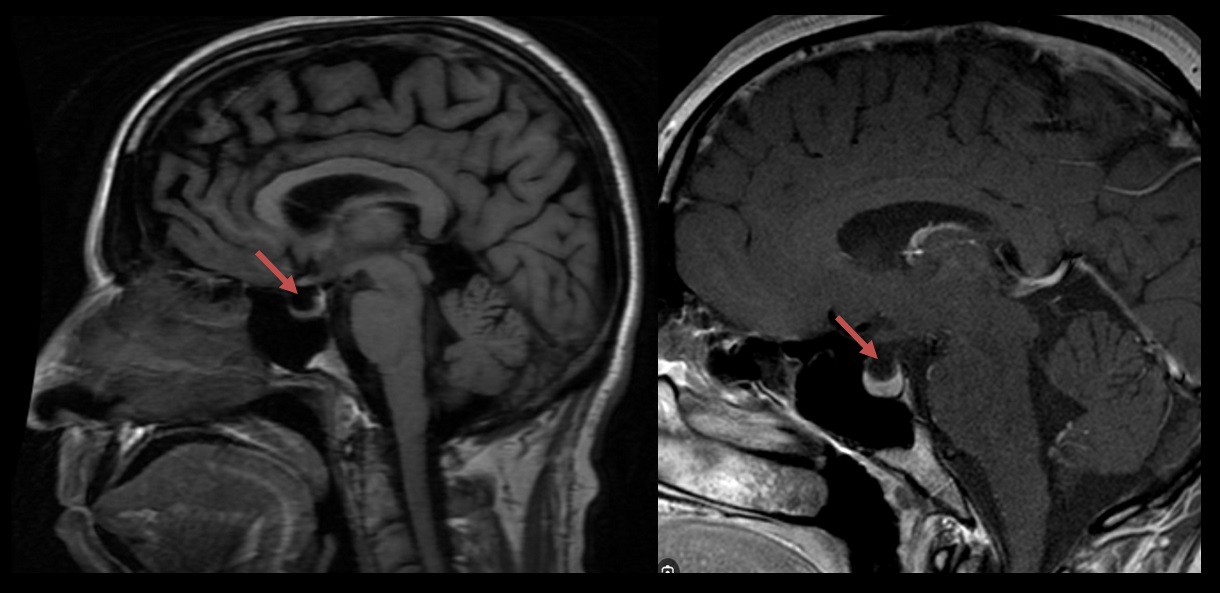
- findings supporting the diagnosis of pseudotumor cerebri include:
- papilledema (intraocular protrusion of the optic nerve disc)
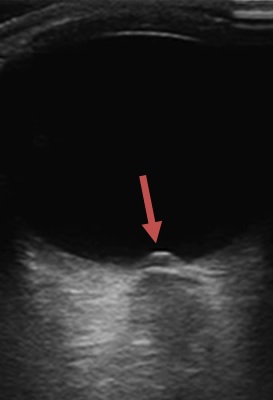
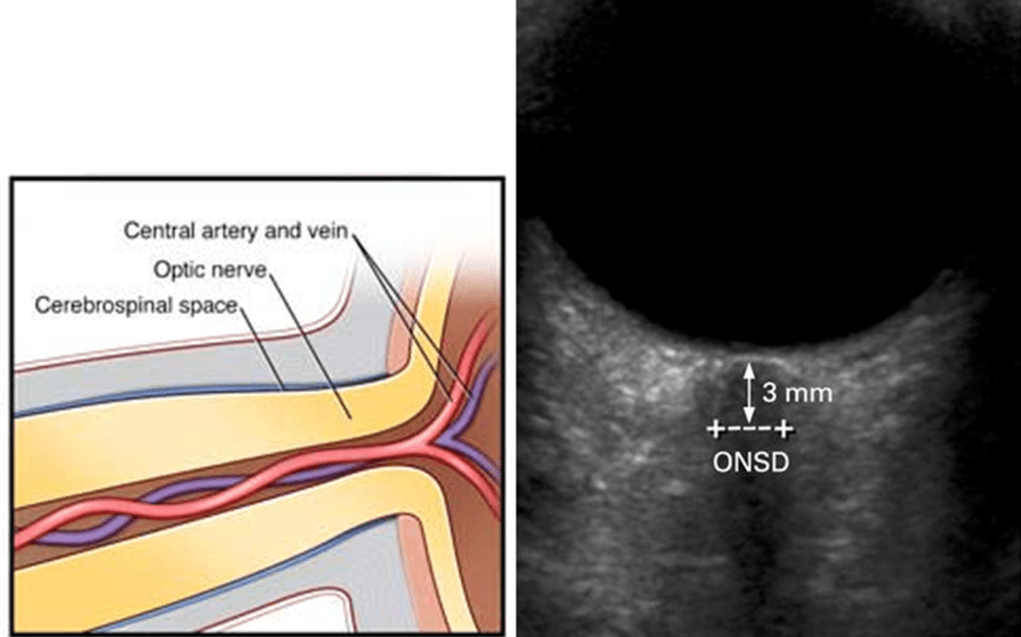
- enlarged subarachnoid spaces around the optic nerves (enlarged ONSD), enhancement of the intraocular segment of the optic nerve
- (partially) empty sella turcica, enlarged Meckel cave (cavum Meckeli), enlarged subarachnoid spaces, abnormal arachnoid granulations
- narrow ventricles
- tonsillar ectopia (exclude Chiari I)
- venous outflow obstruction
- stenosis is most commonly found in the lateral segment of the transverse sinus
- no evidence of recent thrombosis
- compression of the IJV, e.g., by the styloid process
- stenosis is most commonly found in the lateral segment of the transverse sinus
- examination of the fundus ⇒ bilateral papilledema
- detection of the visual field defects in advanced stages
- opening CSF pressure > 25 cm H2O in the supine position
- CSF pressure should be measured in the absence of treatment to lower intracranial pressure
- CSF pressure may be measured by lumbar puncture performed in the lateral decubitus position without sedative medications or by epidural or intraventricular monitoring
- in obese patients, borderline values of 15-25cm H2O cannot be considered clear proof of intracranial hypertension
- if the opening pressure is 20-25 cm H2O, additional findings are needed to make the diagnosis
- opening pressure may fluctuate throughout the day (repeated or prolonged lumbar or intraventricular pressure monitoring may detect these fluctuations)
- CSF composition is normal (which excludes inflammation, meningeal carcinomatosis, etc.)
- relief of the headache after cerebrospinal fluid (CSF) removal is supportive of the diagnosis but not on its own diagnostic: it may be seen in patients with other headache types
- catheter venography allows the detection of stenosis in the outflow venous system, venous manometry, and stenting of intrasinus stenosis
- measurement of the pressure gradient from the superior sagittal sinus to the internal jugular vein and right atrium allows detection of the focal pressure difference across the stenosis (transstenotic gradient)
- an endocrinological or rheumatological examination
IHS classification ICHD-3
Headache attributed to idiopathic intracranial hypertension (IIH) → ICHD-3
- new headache, or a significant worsening of a pre-existing headache, fulfilling criterion C
- both of the following are present:
- idiopathic intracranial hypertension (IIH) has been diagnosed
- cerebrospinal fluid (CSF) opening pressure exceeds 25 cm CSF (or 28 cm CSF in obese children) in the absence of treatment to lower intracranial pressure
- either or both of the following are present:
- headache has developed or significantly worsened in temporal relation to the IIH or led to its discovery
- headache is accompanied by either or both of the following:
- pulsatile tinnitus
- papilloedema
- it is necessary to distinguish pseudopapilledema or optic disc edema (e.g. neuritis, drusen, etc.)
- IIH should be diagnosed with caution in patients without this sign – medication-overuse headache should be excluded in such patients
- no other ICHD-3 diagnosis better explains the headache
Modified Dandy criteria (Friedman, 2002)
- signs and symptoms of intracranial hypertension
- increased lumbar puncture opening pressure (> 25 cm H20)
- normal cerebral spinal fluid contents
- normal neurological findings except for papilledema and/or CN VI palsy, normal mental status
- absence of ventricular enlargement/displacement or space-occupying or vascular lesion on CT+CTV/MRI+
- other causes of increased ICP identified
Differential diagnosis
- space-occupying lesion
- tumor (primary or metastatic)
- abscess
- SDH
- dural sinus or jugular vein thrombosis (septic, aseptic)
- Chiari malformation type I (Fukuoka, 2017)
Management
- management is based on the elimination of triggering factors and symptomatic medication
- if this is not effective and vision deteriorates, surgical/endovascular treatment is indicated
Causal therapy
- the primary task is lifestyle modification and weight reduction in obese patients (for BMI >30 kg/m2, a weight reduction of ∼10-15% is recommended)
- discontinue risky medications (see above)
- compensate diseases that may be associated with increased intracranial pressure (e.g., Addison’s disease or SLE)
- address rare causes or comorbidities within the outflow venous system (see interventional procedures)
Medication
- acetazolamide
- first-line treatment; as a carbonic anhydrase inhibitor, it reduces the production of CSF
- initial dose is 500 mg 2-3 times daily PO., with the total amount increasing up to 2-3 g/day
- common adverse effects include paresthesia of the fingers and lips, nausea, vomiting, decreased attention, renal impairment, or metabolic acidosis; in these cases, the dosage should be adjusted individually according to tolerability
- in most patients, acetazolamide acts quickly and effectively, with resolution of the optic disc edema and stabilization of the perimeter finding in ~2-4 months
- furosemide
- 20-100 mg PO daily with careful monitoring of potassium levels
- possible side effects of furosemide therapy include hyponatremia, hypocalcemia, hypocalcemia, and ototoxicity
- topiramate
- If the condition does not improve, mannitol infusion
- administration of corticosteroids has no sustained therapeutic effect; on the contrary, their rapid discontinuation may worsen the condition
- interventional and surgical treatment should be considered in refractory patients
Endovascular and surgical treatment
- invasive treatment is used when visual impairment progresses despite medication
- optic nerve sheath fenestration
- hard sheaths in the ampullary portion of the optic nerve are
- this alleviates drainage of the cerebrospinal fluid and reduces axonal compression
- the disadvantage is the limited duration of the effect; a relapse may be observed within ~ 3 months; in these patients, neurosurgical intervention is then indicated
- hard sheaths in the ampullary portion of the optic nerve are
- lumboperitoneal or ventriculoperitoneal shunt
- sinus and jugular vein stenting
- reserved for severe cases with transstenotic gradient >8 mmHg
- good results
- internal jugular vein decompression (removal of the external compression – muscle, bones, etc.)
- serial lumbar puncture
- post-puncture discomfort may include headache and blurred vision, which may mimic the worsening of IC hypertension