SUBARACHNOID HEMORRHAGE
Nontraumatic convexal subarachnoid hemorrhage (cSAH)
Updated on 18/02/2024, published on 06/04/2021
Definition
- non-traumatic spontaneous subarachnoid hemorrhage at the convexity (non-traumatic convexal SAH – cSAH) is defined as a collection of blood in one or more adjacent sulci, in the absence of SAH in another localization
- it is relatively rare, but the etiological DDx is quite broad
- in patients ≤ 60 years of age, the most common cause is Reversible Cerebral Vasoconstriction Syndrome [Kumar, 2010]
- in patients > 60 years of age, the most common cause is Cerebral Amyloid Angiopathy (CAA)
Clinical presentation
- severe headache typical for classic SAH is usually not present [Beitzke, 2011]
- headaches are generally present in cerebral venous thrombosis, RCVS, and PRES
- transient focal symptoms (paresthesias, paresis) are frequent, which leads to suspicion of stroke/TIA (cSAH belongs to stroke mimics)
- the etiopathogenesis of transient symptoms is unclear; cortical spreading depression triggered by blood in the SA space is considered [Beitzke, 2011]
Diagnostic evaluation
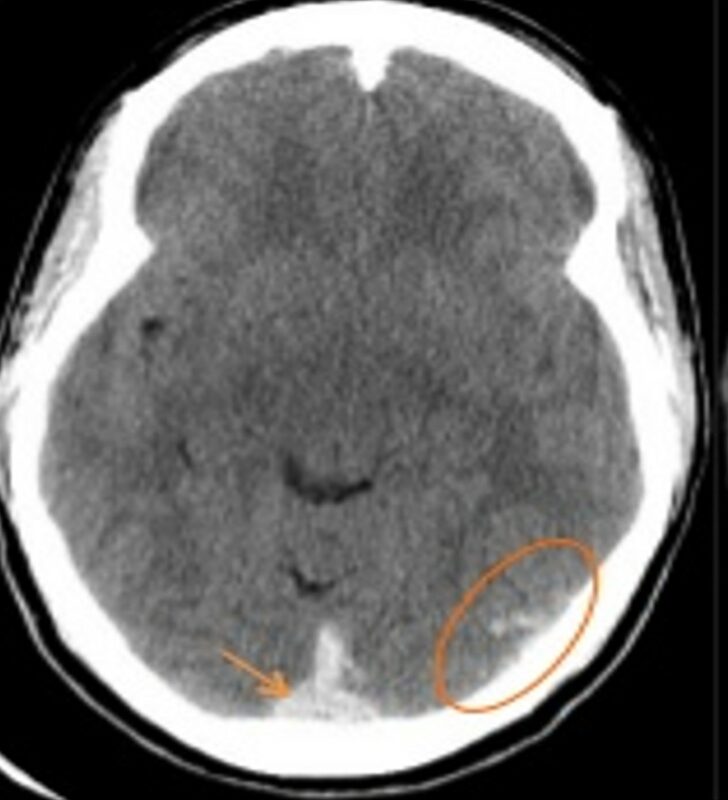
Computed tomography
- the primary diagnostic method
- a finding of sulcal hyperdensity leads to the indication of CTA (both arterial and venous phases)
- CT sensitivity is approx. 90% in the acute phase but decreases quickly with time (the lesion becomes isodense)
- given the wide DDx, it is advisable to add an MRI
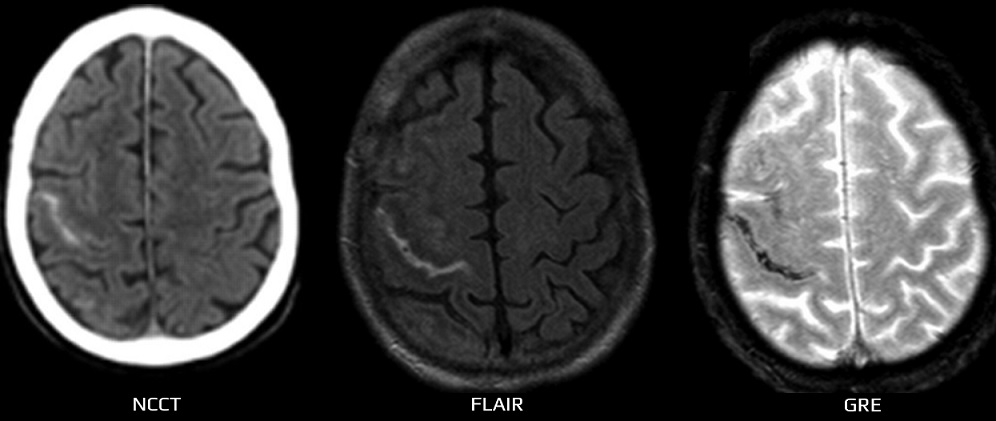
Magnetic resonance imaging
- perform the following sequences:
- FLAIR
- GRE or SWI
- DWI+ADC
- 3D TOF MRA + MR venography
- T1 and T1 C+
- FLAIR is highly sensitive to lesions in the subarachnoid space; cSAH appears as a hyperintense band
- in DDx of cSAH exclude:
- meningitis
- leptomeningeal metastases (LMM) and leptomeningeal melanosis
- post status epilepticus lesions
- previous contrast examination with gadolinium
- artifact
- FLAIR further reveals other typical structural changes in the parenchyma (e.g., PRES, etc.)
- GRE/SWI – confirms the hemorrhagic nature of sulcal hyperintensities and may also help in the detection of older hemorrhages or venous thrombosis
Etiology
- typical parenchymal abnormalities in ~ 50% of cases (edema, cortical infarction with/without a hemorrhagic component)
- cSAH has been described in thromboses of both dural sinuses and superficial veins
- it most likely results from cortical vein rupture due to venous hypertension
- MRI GRE helps detect hemorrhagic lesions and thrombosis itself, including smaller superficial veins (GRE directly displays the thrombus)
→ see here
- hemorrhages occur in approx. 5-17% of PRES cases:
- parenchymal hematoma
- minor hemorrhages
- cSAH
- AVMs can be a source of ICH with SAH; isolated cSAH is rare
- AVM is reliably detected on CTA
- superficially localized cavernous malformations can rarely be the source of cSAH
- extra-axial cavernous malformations are more vascularized and frequently show signs of bleeding on GRE/SWI
- extra-axial cavernous malformations are more vascularized and frequently show signs of bleeding on GRE/SWI
- CAA tends to occur in patients > 60 years of age [Beitzke, 2011]
- it is a degenerative angiopathy characterized by amyloid deposits in the walls of small and medium-sized vessels
- in addition to lobar hematomas and microbleeds, superficial hemosiderosis due to cSAH has also been described
- cSAH is most likely caused by the rupture of amyloid-attenuated leptomeningeal arteries
- clinically, there is no headache but rather focal symptoms, including epileptic seizures
- MRI GRE/SWI is optimal for hemorrhage detection
- RCVS typically presents with headache, variable neurological deficit, and reversible vascular changes
- headache is the most frequent and prominent symptom (often described as a “thunderclap” headache)
- detection of vascular abnormalities on CTA/MRA/TCCD is essential for diagnosis
- MRI shows parenchymal lesions, including cSAH
- the diagnosis is confirmed by the regression of vascular changes within three months
| RCVS |
PACNS |
|
| gender | F > M | M > F |
| onset | sudden onset |
gradual |
| course | monophasic |
chronic with fluctuations or fulminant |
| CSF | commonly normal |
pathologic finding |
| vascular imaging |
always a pathological finding with severe vasospasms resolution within a few weeks (< 3 months) |
negative in up to 50% of cases |
| parenchymal imaging |
usually normal ICH, SAH, or edema (similar to PRES) |
multiple ischemic lesions possible leptomeningeal enhancement |
| vessel wall imaging (T1C+ dark or black blood high-res images) |
negative |
positive [Obusez, 2014] [Mandell, 2012] |
- cSAH can be caused by the rupture of an infectious aneurysm (meningitis, endocarditis) or due to focal arteritis
- rarely, cSAH has been described as a consequence of abscess (again due to focal arteritis)
- clinical presentation: headache, general signs of infection (anorexia, fatigue, fever, etc.), or focal signs (caused by the mass effect of an abscess or ischemia and microhemorrhage)
- typical for Moyamoya disease or moyamoya syndrome is intraparenchymal or intraventricular bleeding
- cSAH is rare, most likely due to a rupture of dilated cortical arterioles
- a typical angiographic findings confirm the diagnosis
- in cases of hemodynamically significant extra- or intracranial stenosis, collateral circulation becomes involved
- the rupture of a dilated, congested pial artery may lead to cSAH (Hacein-Bey, 2014)
- FLAIR imaging shows serpiginous hyperintense structures, similar to the “ivy sign” described in moyamoya patients
- cSAH due to malignancy can be provoked by coagulopathy, venous thrombosis, PRES, or RCVS (potential side effect of chemotherapy)
- leptomeningeal metastases are a major consideration in DDx of cSAH
- both conditions share similar findings on CT and FLAIR imaging
- a sudden headache favors the diagnosis of SAH; however, it is often missing in cSAH
- leptomeningeal dissemination is characterized by a gradual development of cranial nerves paresis and postcontrast enhancement of the meninges (on T1 or FLAIR)
- in the subacute stage, cSAH appears hypointense on GRE
Differential diagnosis
- traumatic SAH
- history of trauma
- usually, a more significant extent of SAH in imaging methods
- concurrent contusions, sometimes only seen on a follow-up CT scan
- skull bone trauma is visible in the bone window
- cortical laminar necrosis
- associated with hyperintense lesions on MR DWI
- leptomeningeal metastases