CEREBRAL VENOUS SINUS THROMBOSIS
Diagnosis of cerebral venous sinus thrombosis
Updated on 08/05/2024, published on 07/04/2020
- establishing the diagnosis of Cerebral Venous Sinus Thrombosis (CVST) is often difficult in the early stages; the temporal course and clinical symptoms are variable and often nonspecific
- focal neurological symptoms typically occur in association with venous infarcts
- exclude CVST in the presence of:
- intracranial hypertension syndrome
- atypical ischemias – especially those with atypical localization, not respecting traditional arterial territories, and featuring a hemorrhagic component or edema
- first epileptic seizure (especially in young women)
- hyperdense sign on noncontrast CT
- if CVST is suspected, imaging modalities such as MR imaging and MR venography (MRV) or CT venography (CTV) can help confirm the diagnosis
Neuroimaging
- neuroimaging is essential for the diagnosis of cerebral venous sinus thrombosis
- CT is widely available and is the most commonly used baseline imaging modality, although MRI with venous TOF sequence is preferred (especially in pregnancy)
|
When should you think about cerebral venous sinus thrombosis?
|
|
| Direct signs of thrombus in the vein/dural sinus | |
|
Indirect signs
|
|
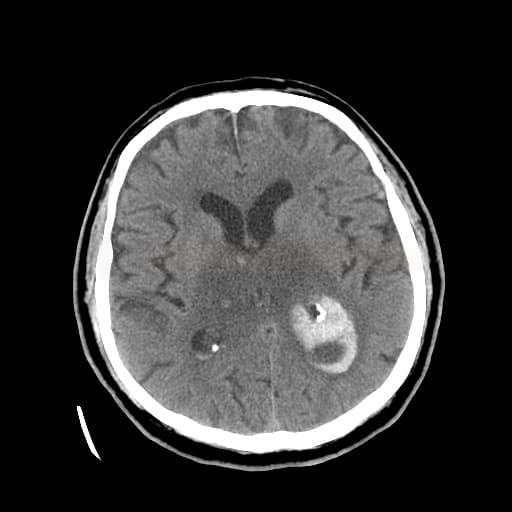
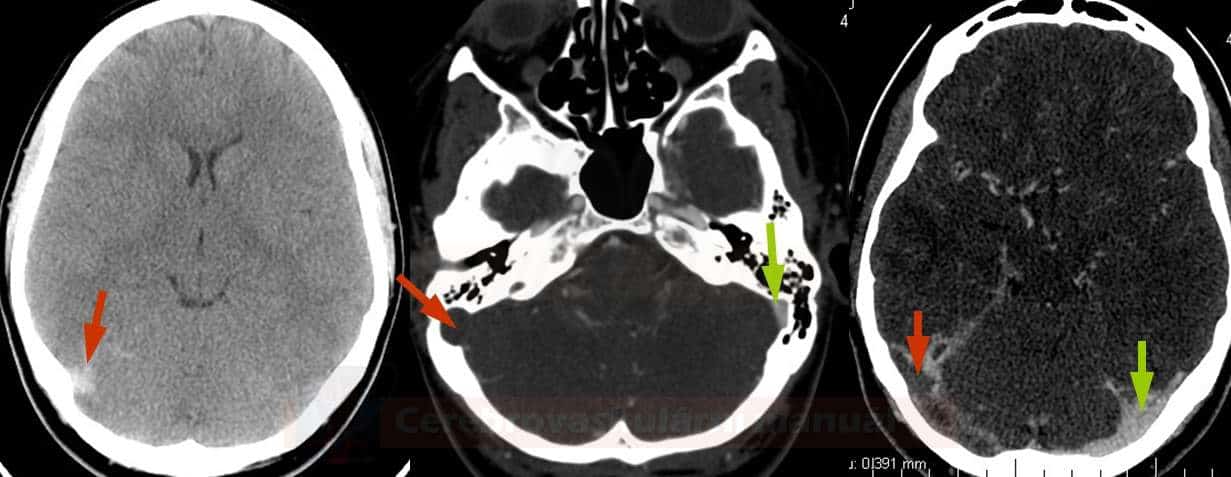
CT + CT venography
- non-contrast CT scan (NCCT) of the brain is normal in up to 30% of cases
- always evaluate separately
- non-contrast CT images (hyperdensity sign – cord sign, dense clot sign) – positive in 25% of cases
- contrast-enhanced CT images (empty delta sign) – positive in 16-46%
- indirect signs of thrombosis include edema, an atypically located infarct, often with a hemorrhagic component
- a hyperdense sign may be false-positive; additional signs are required for diagnosis
- a false-positive finding in cases of polyglobulia
- typical values with CVT are > 70 HU
[Black, 2011]
- a false-positive finding in cases of polyglobulia
- a CT scan may detect associated inflammatory changes (such as otitis, mastoiditis, sinusitis)
- CT venography (CTV) is a reliable alternative to MR venography (MRV) or digital subtraction angiography (DSA) (ESO guidelines 2017)
- a time delay of 25-45 seconds compared to CTA is recommended
- sensitivity for dural sinus thrombosis is up to 95% compared to DSA
- alternative to MRV – MRI offers superior visualization of thrombus and parenchymal changes
- disadvantages:
- difficulty distinguishing between sinus hypoplasia and aplasia (5-20% of cases)
- exposure to radiation and contrast media
- limited diagnostic value in cortical vein thrombosis
- a time delay of 25-45 seconds compared to CTA is recommended
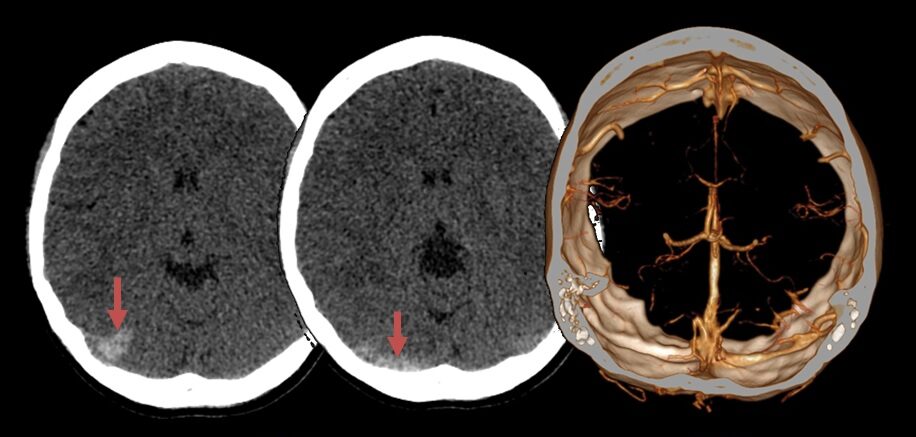
MRI + MR venography
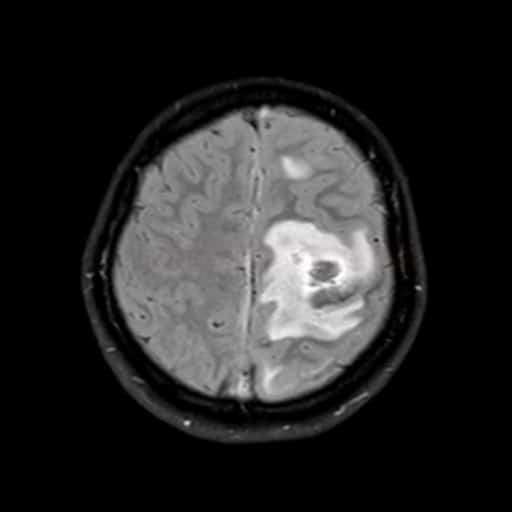
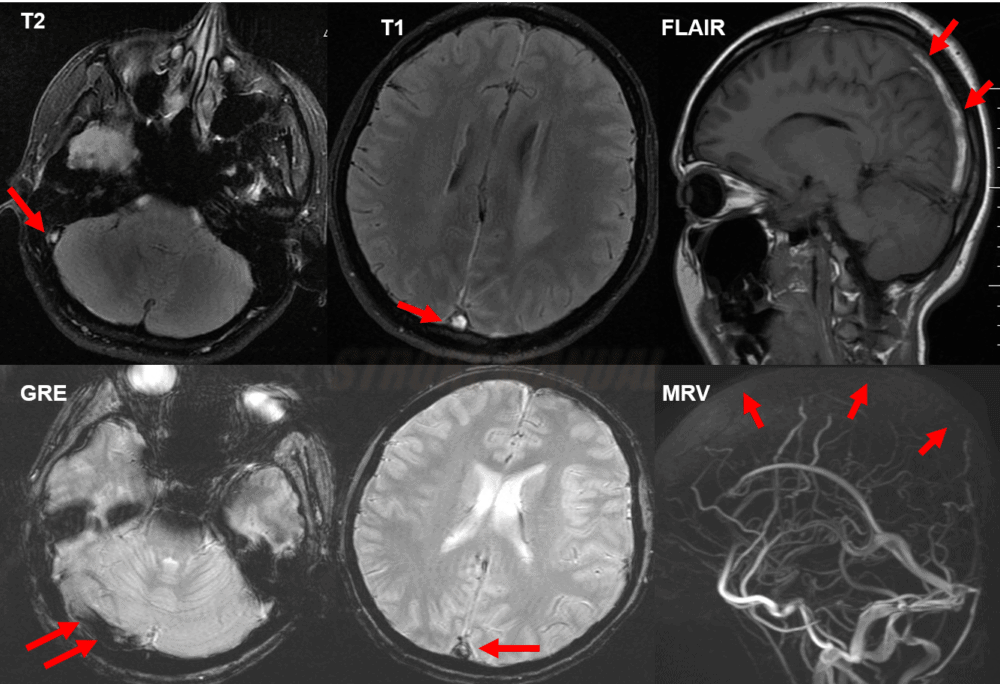
- hyperintense venous infarct in an atypical location, often with a hemorrhagic component and edema
- typically found in parasagittal and temporal regions
- DWI may show decreased, normal, increased, or a mixture of diffusivity in areas of venous infarction
- hemorrhage may vary from large hematomas to petechial hemorrhages within edematous tissue
- T2 and FLAIR sequences typically demonstrate the absence of a flow void (sinuses are usually hypointense)
- thrombosis < 24h or > 3 days
- thrombus in the acute stage (within 3 days) can be confused with normal flow void, as it is T1/T2 hypointense during this period
- from day 4, the thrombus should become hyperintense (bright)
- beware of potential confusion with hypoplasia (assess the size of the jugular foramen for differentiation)
- on GRE/SWI, the thrombus appears hypointense in the vein or sinus (DDx of a small SAH)
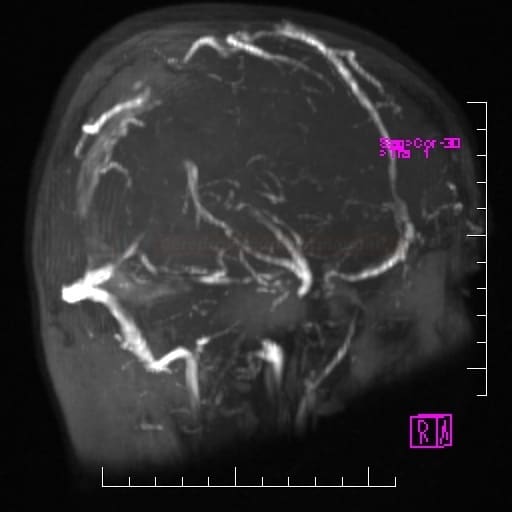
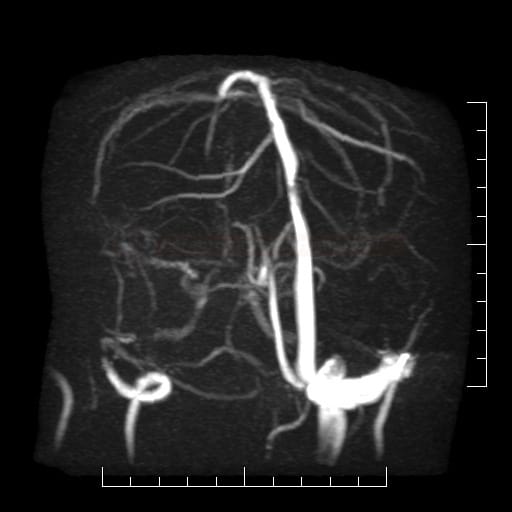
- MR venography (MRV) uses the time-of-flight (TOF) technique; the assessment may be complicated by sinus hypo- or aplasia or asymmetric flow
- MRV is considered a reliable alternative to DSA for diagnosing cerebral venous sinus thrombosis (ESO guidelines 2017)
Digital subtraction angiography
- consider possible anatomical variants of the venous system, including hypoplasia or the absence of some vessels
- a specific indicator for CVST diagnosis is the presence of a “stop sign” (abrupt termination of a sinus or vein) accompanied by collateral circulation and congestion of cortical veins (characterized by dilation, tortuosity)
- DSA may show associated cortical vein thrombosis and possibly arterio-venous fistula as well as deep vein thrombosis
- in addition, DSA shows the dynamics and drainage pattern in the occluded area
- after applying the contrast agent, the venous system is completely visualized within 7-8 seconds
- in cases of thrombosis, the filling of the veins is delayed or absent
- currently, MRV and CTV dominate the diagnostic workup, and DSA is reserved for interventional procedures when conservative therapy fails
Neurosonology
- the method has low sensitivity and specificity
- indirect signs are mostly evaluated: flow acceleration (> 40 cm/s) due to collateral circulation
- sigmoid sinus (SS) thrombosis may be monitored by examining flow in the ipsilateral internal jugular vein (IJV)
- more information on TCCD examination of cerebral veins and sinuses is here
Additional diagnostic studies
D-dimers
- normal D-dimer levels: 0.068-0.494 mg/L
- may serve as an important screening tool (with sensitivity > 95%); testing D‐dimer together with fibrinogen may increase specificity
- the sensitivity and specificity using D-dimer alone were 94·1% and 97·5%, whereas those for D-dimer + fibrinogen were 67·6% and 98·9% [Meng,2013]
- elevated levels can occur in various conditions, including infection, trauma, or malignancy
- a normal D-dimer level makes the diagnosis of acute thrombosis unlikely but does not definitively exclude it (AHA/ASA 2011 IIb/B) [Kosinki, 2005] [Lalileve,2003]
- positive in ~ 94% of patients with CVT (ESO guidelines 2017)
- a false-negative result may be seen in cases of isolated headache and prolonged thrombosis (lasting > 1 week)
- on the other hand, false-positive results are common (see below)
- after anticoagulation therapy, D‐dimer levels gradually normalize; fibrinogen levels may remain elevated for several weeks
| Content available only for logged-in subscribers (registration will be available soon) |
Lumbar puncture
- perform a lumbar puncture to rule out an infectious etiology (if suspected)
- drainage of ∼ 20-30 mL of cerebrospinal fluid (CSF) may alleviate pain or prevent vision loss
- typical signs of venous thrombosis include increased opening pressure, proteinorhachia, and occasionally mild pleocytosis
- mild pleocytosis may lead to misdiagnosis of neuroinfection
- lumbar puncture is contraindicated in the presence of an expansive parenchymal lesion
Other laboratory studies
| Content available only for logged-in subscribers (registration will be available soon) |
EEG
- pathological findings are predominantly associated with parenchymal lesions
- if mental status is altered, nonconvulsive status epilepticus (NCSE) should be excluded
Differential diagnosis
- high-flow dural A-V fistula can lead to venous congestion and subsequent hemorrhagic infarction (which can be difficult to distinguish from a venous thrombosis)
- headache and encephalopathy are less common in ischemic stroke
- compared to ischemic stroke, infarct lesions in CVST differ in shape and location
- in CVST, hemorrhagic transformation and collateral edema are commonly observed on baseline imaging
- look for signs of inflammation – fever, leukocytosis with elevated CRP and ESR
- positive CSF findings (pleocytosis, elevated protein level)
- consider a combination of venous thrombosis and neuroinfection (in such instance, thrombosis is likely triggered by the infection)
- typical symptoms and signs of IIH include
- headache
- abducens palsy
- papilledema, visual disturbances (e.g., transient visual obscurations)
- venous thrombosis should be excluded via MR venography (MRV) or CT venography (CTV)
- lumbar puncture rules out infection and confirms elevated CSF pressure (through direct measurement of the opening pressure)
- symptoms atypical for IIH:
- encephalopathy
- focal neurological deficits
- seizures
FAQs
- common symptoms include headache, often severe and persistent, especially if worsening over time
- other symptoms may include focal neurological deficits (such as visual disturbances), seizures, altered mental status, and other signs of intracranial hypertension
- the clinical presentation can be varied and depends on the location and extent of thrombosis; a high index of suspicion is necessary, especially in patients with risk factors such as pregnancy, oral contraceptive use, prothrombotic conditions, or recent head injury
- diagnosis is typically confirmed through imaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) venography, which can visualize the thrombosed veins and sinuses
- MRI combined with MRV is the diagnostic imaging of choice for CVST as it provides detailed visualization of cerebral veins and sinuses and brain parenchyma
- CTV is an alternative, especially when MRI is contraindicated or unavailable, but it is less sensitive in detecting acute thrombosis in smaller veins.
- there is no specific laboratory test confirming the diagnosis
- elevated D-dimer levels can suggest thrombosis, they are not specific for CVST and can be elevated in various conditions
- normal D-dimer levels may help exclude CVST in patients with a low pre-test probability, but due to its limited sensitivity, a normal D-dimer level cannot definitively rule out CVST
- lumbar puncture is not primarily used to diagnose CVST
- it may be performed to analyze the cerebrospinal fluid (CSF) for signs of inflammation, infection or subarachnoid hemorrhage and to confirm increased intracranial pressure
- proceed with caution due to the risk of herniation if significant mass effect is present
- imaging may reveal absence of flow within affected veins or sinuses, filling defects representing thrombi, and signs of venous congestion such as engorgement of cortical veins or dilated deep veins
- the “empty delta sign” on contrast-enhanced CT is a characteristic finding, representing a non-opacified thrombosed sinus surrounded by contrast
- key radiological signs of CVST on MRI/MRV include the absence of flow void in the affected sinuses, the presence of a filling defect, and evidence of venous infarction or hemorrhage
- transcranial Doppler ultrasound may be used to assess cerebral blood flow velocity and detect abnormal flow patterns suggestive of venous obstruction
- however, it is less sensitive than imaging modalities such as MRI or CT venography and may not reliably visualize the thrombosed veins or sinuses
- while clinical suspicion is important, the diagnosis typically requires confirmation through imaging studies
- in rare cases where imaging is inconclusive, further evaluation with repeat imaging or digital subtraction angiography may be necessary
- understanding the location and extent of CVST is fundamental for predicting clinical outcomes, guiding management strategies, assessing treatment response, and monitoring for potential complications
- while anticoagulation is the cornerstone of treatment, extensive or strategically located thromboses (such as deep venous system) may warrant more aggressive interventions, including endovascular procedures or neurosurgical interventions