ADD-ONS / MEDICATION
Statin intolerance
Updated on 11/05/2024, published on 14/11/2023
Abbreviations: ULN = upper limit of normal. CK = creatine kinase , LDL = low density lipoprotein, SAMS = statin associated muscle symptoms, EAS = European Atherosclerosis Society
- statins are competitive inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGCR), lowering the level of cholesterol and low-density lipoprotein and significantly reducing cardiovascular morbidity and mortality
- the use of statins to achieve LDL cholesterol target levels may be limited by adverse symptoms
- the term “statin intolerance” should be used with caution
- unjustified discontinuation of correctly indicated statin therapy may have consequences for the patient in terms of recurrence or primary manifestation of cardiovascular events
- the term “statin intolerance” should be used with caution
Definiton
- statin intolerance refers to the inability to tolerate statin therapy due to the occurrence of adverse effects
- intolerance leads to either the discontinuation of therapy or dose reduction
- intolerance is rarely life-threatening
- it is confirmed by:
- reversal of clinical symptoms and/or normalization of creatine kinase (CK) levels after discontinuation of statin therapy
- recurrence of myalgia or at least a 4-fold elevation of CK levels after resumption of therapy
- at least two different statins should be tested for a comprehensive assessment
- statins have been associated with a nocebo effect, whereby patients experience adverse effects based on the expectation of harm from a treatment
- the most common symptom of intolerance is statin myopathy
- asymptomatic CK elevation
- myalgia, cramps, muscle weakness
- rhabdomyolysis (up to 10% mortality)
- it usually occurs within the first year of therapy and is partially or completely reversible after discontinuation of statins
- an exception is statin-induced necrotizing autoimmune myopathy (SINAM) associated with autoantibodies against HMGCR, which usually appears years after the initiation of statin therapy and requires immunomodulatory treatment
- muscle problems are sometimes also referred to as SAMS (Statin Associated Muscle Symptoms) or SAM (Statin Associated Myopathy)
Definition of statin intolerance according to the EAS consensus
- the definition from the ODYSSEY ALTERNATIVE and GAUSS 2 studies is used ⇒ intolerance is defined as the inability to tolerate ≥ 2 statins at minimal doses
- complete statin intolerance – inability to tolerate any of the three major statins at their usual lowest starting doses (rosuvastatin 5 mg, atorvastatin 10 mg, simvastatin 20 mg)
- partial statin intolerance – inability to tolerate statins in the form and doses necessary to achieve target levels
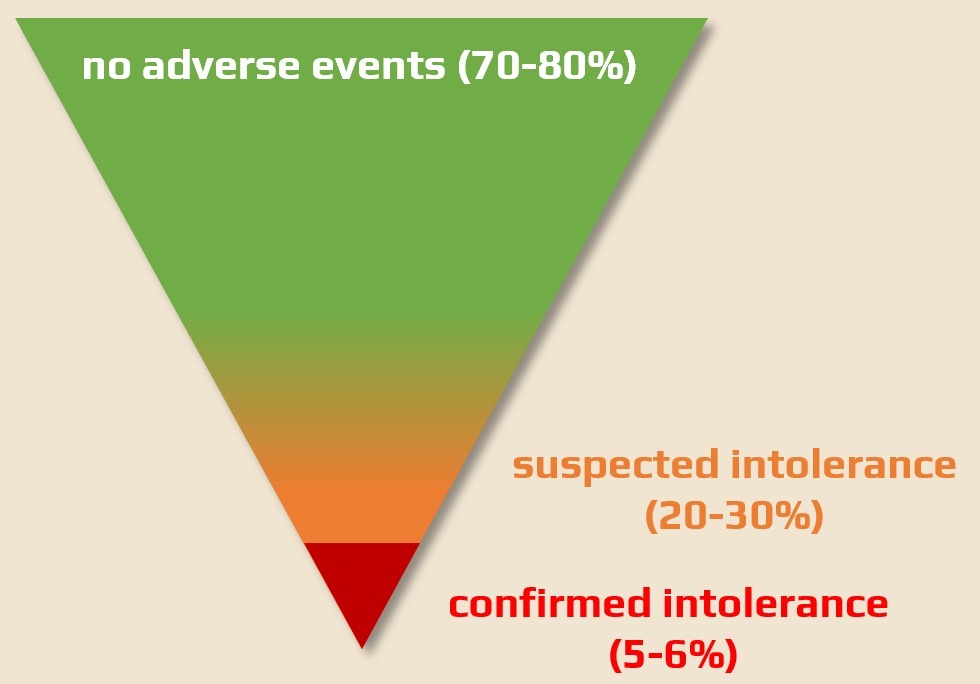
Epidemiology
- the incidence of statin myopathy is estimated to be 1-5% according to randomized trials, while observational studies suggest it could be as high as 30%
- severe statin myopathy is relatively rare, and in many cases, myalgia is unrelated to statin therapy
- smaller proportion of patients have complete statin intolerance (~5-6%)
- the incidence of rhabdomyolysis is reported to be 1-4 cases per 100,000 patients per year (in contrast, GI bleeding with ASA is 120/100,000 per year) [Derry, 2000]
- the highest incidence was seen with cerivastatin or with a combination of other statins and gemfibrozil
- the mortality rate for rhabdomyolysis is ~ 10% (e.g., 1 in a million)
Risk factors
- the risk of myopathy can be reduced by knowing the risk factors and basic and most common drug interactions (amiodarone, propafenone, verapamil, diltiazem, amlodipine, macrolides, azole antifungals) – see table
- when present, start slow titration of the statin, preffering a drug with a lower risk of interactions
- the risk applies to all statins (“class effect”) and is dose-dependent
- the highest risk appears to be with simvastatin, the lowest with fluvastatin
- the risk of other statins (pravastatin, atorvastatin, rosuvastatin) is similar
- CYP3A4
- inhibition of CYP3A4 leads to slowed degradation and elimination of the statin, increasing the risk of adverse effects due to increased exposure
- strong inhibitors (e.g., macrolide antibiotics – especially clarithromycin, erythromycin, to a lesser extent roxithromycin), azole antifungals (ketoconazole, itraconazole), most protease inhibitors (antivirals) and cyclosporine A
- moderate inhibitors (amiodarone, propafenone, calcium channel blockers verapamil, diltiazem and amlodipine)
- CYP2C9
- a significantly smaller amount of drugs are metabolized this way
- CYP2C9 is significantly inhibited by fluconazole and partially by amiodarone; omeprazole is a weak inhibitor of 2C9
Classification and clinical presentation of myopathies
- various classifications and definitions of individual items
Myotoxic myopathies (statin-associated myopathy – SAM)
|
|
Immune-mediated myopathy
|
|
Diagnostic evaluation
- diagnosing SAM is difficult because there is no highly reliable biochemical marker to confirm or rule out the diagnosis
- increased creatine kinase and myoglobin is a non-specific findings – it can be caused by myopathy of any etiology and also by recent muscle activity (48-72 hours), alcohol abuse, hypothyroidism, malignancy, and a variety of other conditions
- in some individuals, chronic elevation of CK may be observed without an apparent cause, known as idiopathic hyperCKemia
- to assess the causal relationship between statin treatment and myalgia, the most important factors are the temporal relationship and the nature of the myalgia
- symptoms can be attributed to statins if they occur during the first month of treatment and improve within 4 weeks after discontinuation or reappear after resumption of treatment
- statin myalgia tends to be symmetrical, affecting the proximal large muscle groups (thighs, arms), with diffuse pain or cramping, stiffness, or muscle weakness and inefficiency. On the other hand, muscle pain in small isolated areas, paresthesias, twitching, or pain localized to tendons and joints are not indicative of statin-induced pain
- symptoms can be attributed to statins if they occur during the first month of treatment and improve within 4 weeks after discontinuation or reappear after resumption of treatment
| Clinical symptoms (new or newly worsened) score | score |
| Regional distribution | |
| symmetrical hip flexor pain | 3 |
| symmetrical calf pain | 2 |
| symmetrical proximal muscle pain | 2 |
| nonspecific asymmetric intermittent pain | 1 |
| Time factor | |
| onset of symptoms in < 4 weeks | 3 |
| onset of symptoms in 4-12 weeks | 2 |
| onset of symptoms after 12 weeks | 1 |
| Change after statin discontinuation | |
| improvement in < 2 weeks | 2 |
| improvement in 2-4 weeks | 1 |
| improvement after 4 weeks | |
| Change after statin reintroduction | |
| same symptoms in < 4 weeks | 3 |
| same symptoms in 4-12 weeks | 1 |
| Probable association with statin | 9-11 |
| Possible association with statin | 7-8 |
| Unlikely association with statin | < 7 |
| SAMS less likely |
SAMS likely |
| Nature of symptoms | |
| unilateral
nonspecific distribution tingling , twitching, joint pain |
bilateral
large muscle groups musclke ache, weakness, stiffness, cramps, general fatique |
| Timing of symptoms | |
| onset before statin initiation
onset > 12 weeks after statin initiation |
onset 4-6 weeks after statin initiation
onset after statin dose increase |
| Other considerations | |
| hypothyroidism, polymyalgia rheumatica
vitamid D deficiency medicines heavy physical activity |
presence of risk factors (see table above) |
| CK levels | |
| elevated
elevated CK levels decrease after statin ceased |
|
Prevention and management of statin myopathy
Precautions
- look for preexisting muscle disease and myalgia
- identify risk factors and dangerous concomitant medications (see table above)
- carefully review drug contraindications (e.g., reduce rosuvastatin dose in renal insufficiency)
- consider a hydrophilic statin (fluvastatin, rosuvastatin) for patients with polypharmacy
- In the presence of risk factors, choose a lower dose and titrate gradually with frequent clinical and laboratory monitoring
- include CK and TSH in the initial testing (to exclude asymptomatic hypothyroidism)
- CK elevation <5 times the normal value does not exclude statin therapy
- repeatedly educate patients about possible adverse effects of medication and drug interactions
Monitoring of therapy
- monitor symptoms – check regularly for muscle pain or weakness that may indicate side effects, especially during the first 12 months
- monitor drug interactions – always ask about new medications.
How to proceed with an asymptomatic elevation of CK
- exclude causes other than statin myotoxicity
- ↑CK >10 x ULN or rhabdomyolysis – discontinue treatment
- ↑CK 5-10 x ULN – medication can be continued, possibly reduce the dose, monitor CK and muscle difficulties
- ↑CK <5 x ULN normal – continue statin medication, monitor for muscle symptoms, recheck CK in one month
- classify symptoms:
- myalgia
- cramps
- muscle weakness (degree, distribution)
- examine the serum creatine kinase and myoglobin levels
- exclude hypothyroidism, hepatopathy, and nephropathy
- review and adjust concomitant medication if necessary
- exclude other causes
- rhabdomyolysis or 10-fold elevation of creatine kinase: discontinue statin
- myalgia not significantly affecting quality of life and without markedly elevated CK: reduce or maintain current dose
- regular and careful monitoring is required
- adjust dose or switch statin:
- reduce the dose
- try alternate-day dosing (some patients may tolerate statins if taken less frequently)
- coenzyme Q10 supplementation – some evidence suggests that it may help with muscle-related side effects
- if muscle symptoms are related to statin myotoxicity, symptoms should improve within 2-3 months after discontinuation of statins
- if muscle symptoms occur > 6 months after initiation of statin therapy and persist or worsen despite discontinuation of statin, consider immune-mediated necrotizing myopathy (SINAM) or other autoimmune myositides ⇒ test for anti-HMGCR antibodies and consider muscle biopsy
- wait for the disappearance of symptoms and/or CK normalization
- start the same statin at a lower dose with very slow titration or alternative dosing (e.g., every other day, 1-2 times a week) or switch to another statin (preferably hydrophilic fluvastatin or rosuvastatin)
- LDL reduction can also be achieved with rosuvastatin 5-10 mg daily or by administering this dose every other day or even 1-2 times a week [Gadarla , 2008]
- up to 80% of patients with previous intolerance will tolerate this alternative dosing
- LDL reduction can also be achieved with rosuvastatin 5-10 mg daily or by administering this dose every other day or even 1-2 times a week [Gadarla , 2008]
- use or add a non-statin hypolipidemic agent → see here
- ezetimibe – alone or ideally (in terms of preventive effect) in combination with at least a minimal statin dose
- evolocumab – PCSK9 inhibitor (proprotein convertase subtilisin/kexin type 9)
- inclisiran (LEQVIO)



