ADD-ONS / SCALES AND SCORES
ROPE score
(Risk of Paradoxical Embolism)
Updated on 04/07/2024, published on 01/06/2023
- the prevalence of the patent foramen ovale (PFO) in the general population is approximately 25%
- PFO is overrepresented in the population with cryptogenic stroke (CS) ( (prevalence of approx. 50%)
- the discovery of a PFO in an individual stroke patient with an otherwise occult etiology is not synonymous with a diagnosis of paradoxical embolism
- the RoPE score has been proposed to help establish the relationship between cryptogenic stroke and PFO
- validation indicates that the RoPE score identifies cryptogenic stroke patients who are likely to have a pathogenic PFO
- the relationship between the RoPE score and the effect of PFO closure was evaluated in 3 randomized trials (Kent, 2020)
- in the low RoPE score group (<7), the rate of recurrent strokes per 100 person-years was 1.37 in the device arm versus 1.68 in the medical arm (hazard ratio, 0.82 [0.42-1.59] P=0.56) compared with 0.30 versus 1.03 (hazard ratio, 0.31 [0.11-0.85] P=0.02) in the high RoPE score group (≥7)
- PFO causality cannot be proven with 100% certainty; other causes of stroke may still require investigation
- the score does not predict the benefit of PFO closure; the benefit depends on the likelihood that the PFO was causally related to the stroke and and the probability of stroke recurrence
- patients with a high RoPE score are more likely to have a ‘pathogenic’ PFO but they also appear to have a lower risk of stroke recurrence
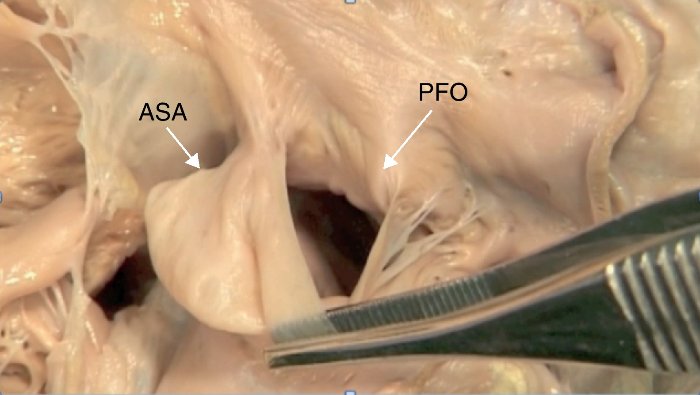
- the RoPE score that does not reflect anatomical characteristics of the PFO ((e.g., shunt size, presence of atrial septal aneurysm); these variables were included in the modified AF-RoPE score
- patients with a high RoPE score are more likely to have a ‘pathogenic’ PFO but they also appear to have a lower risk of stroke recurrence
- ⇒ the score should not be used in isolation to determine which patients with a PFO should undergo a closure procedure
- step 1 – use the RoPE score to predict which patients are likely to have experienced cryptogenic strokes attributable to PFO
- step 2 – incorporate additonal factors to decide whether to proceed with PFO closure
| Characteristic | Points |
| no history of hypertension | 1 |
| no history of diabetes | 1 |
| no history of prior stroke or TIA |
1 |
| non-smoker | 1 |
| cortical infarct on imaging | 1 |
| Age | |
| 12-29 | 5 |
| 30-39 | 4 |
| 40-49 | 3 |
| 50-59 | 2 |
| 60-69 | 1 |
|
≥ 70
|
0 |
| Points (0-10) | |
- maximum score 10 – a patient < 30 years of age without vascular risk factors, no history of stroke/TIA, and with a cortical infarct
- minimum score 0 – a patient ≥ 70 years of age with vascular risk factors, a history of stroke, and no cortical infarct
| RoPE score | The probability that PFO is the cause of stroke (95% CI)) | Estimated stroke/TIA recurrence at 2 years |
| 0-3 | 0% (0–4) | 20% (12–28) |
| 4 | 38% (25–48) | 12% (6–18) |
| 5 | 34% (21–45) | 7% (3–11) |
| 6 | 62% (54–68) | 8% (4–12) |
| 7 | 72% (66–76) | 6% (2–10) |
| 8 | 84% (79–87) | 6% (2–10) |
| 9-10 | 88% (83–91) | 2% (0–4) |