NEUROIMAGING / NEUROSONOLOGY
Physical principles of ultrasound
Updated on 12/12/2023, published on 28/03/2022
The key physical principles needed to understand and optimize the ultrasound examination are included
Basic ultrasound variables and parameters
- ultrasound = acoustic waves (pulses of sound) with a frequency of > 20 kHz
- generators of ultrasound for medical applications are piezoelectric crystals
- crystals in a transducer (probe) are excited by electrical pulses (piezoelectric effect); one type of energy is converted into another (electrical ⇒ mechanical)
- the probe (transducer) emits ultrasound pulses that propagate through tissues and then return to the transducer as echoes (reflections)
- reflected echoes are converted back into electrical impulses by the transducer crystals and then are transformed into the ultrasound image
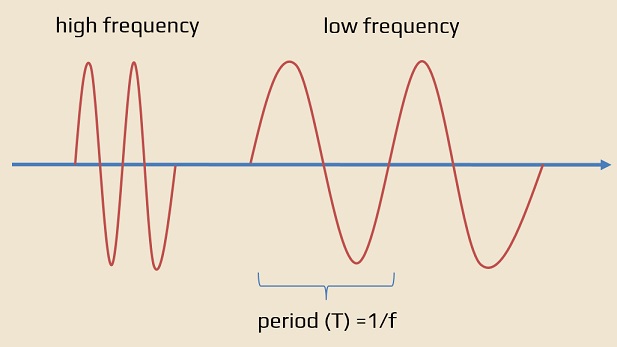
- period of an ultrasound wave is the time that is required to complete one cycle – the time from the beginning of one cycle till the beginning of the next cycle (period = 1/frequency)
- frequency – the number of periods (oscillations) per second, measured in hertz (Hz)
- 1/sec = 1 Hertz (Hz)
- frequency is environmentally independent
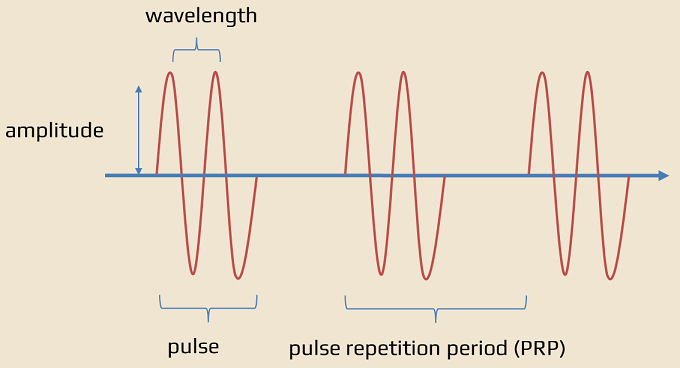
- wavelength – describes the length of a single cycle or the distance that a wave travels in one period
- unlike frequency and period, wavelength depends not only on the frequency but also on the speed of sound through the environment = it is determined by both the source and the medium
- it affects the longitudinal image resolution and, consequently, image quality
- wavelength (mm) = propagation speed in tissue (mm/microsecond) / frequency (MHz) ⇒ higher frequency means the shorter wavelength
- amplitude – refers to the strength of the sound wave, defined as the difference between the peak value and the average value of the waveform
- expressed in decibels (dB), which is a logarithmic scale
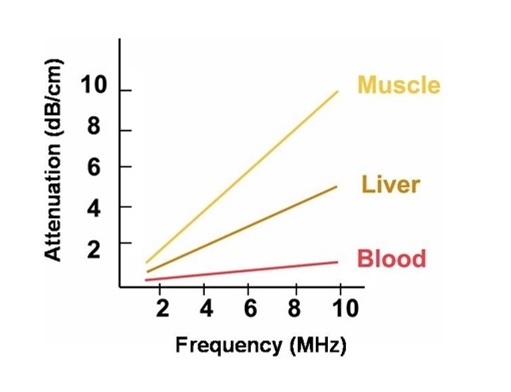
- the amplitude decreases as the ultrasound moves through tissue (attenuation)
- amplitude usually decreases by 1 dB per 1 MHz per 1 centimeter traveled (back and forth)
- with a 9 MHz probe examining the target at 4 cm (8 cm total distance), the amplitude attenuation will be 1 dB x 9 MHz x 8 cm = 72 dB
- power (W) – the total amount of energy in the ultrasound beam
- determined by the sound source
- decreases as the beam propagates through tissues
- power and amplitude are closely related, with power being proportional to the square of the amplitude
- most of the energy carried by high-intensity ultrasound in tissue is converted to thermal energy
- intensity (W/cm2) of the ultrasound beam is defined as the concentration of energy in the beam; it decreases as the ultrasound propagates through tissue
- intensity = Power (W) / beam area (cm2)
- intensity is a key variable in ultrasound safety
- propagation speed – says how fast the ultrasound can travel through the tissue
- in the human soft tissue, the average speed is 1540 m/s
- speed is determined by the medium only; the denser the medium, the slower the speed of the ultrasound
- speed enables the calculation of the approximate distance to the examined object
Tissue propagation
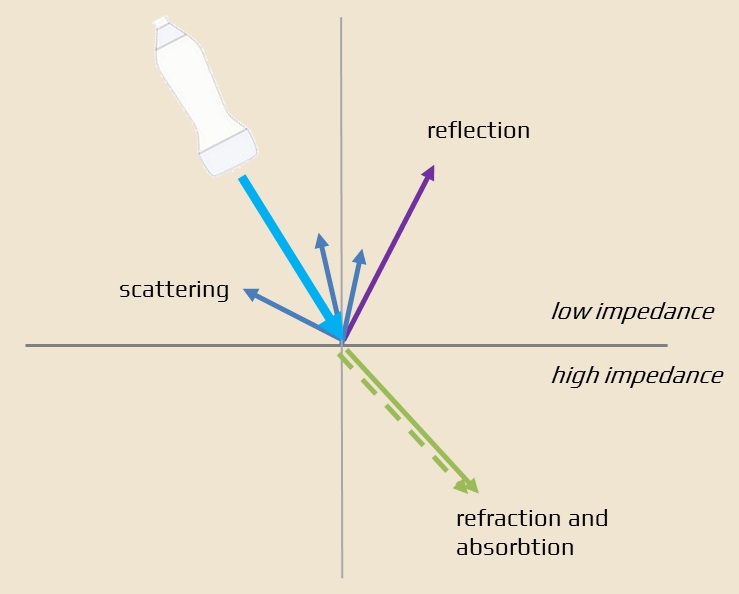
- as ultrasound propagates through the tissue, its intensity (attenuation) decreases because of reflection, scattering, and absorption of ultrasound energy at the surfaces between tissues of different densities
- attenuation depends on the frequency: attenuation (dB)= 0.5 x propagation length x frequency
- reflection (the greater the difference between the impedance, the greater the amplitude of the reflected echo and the lower the intensity of the transmitted ultrasound)
- scattering (at a relatively small, uneven interface or with particles in suspension)
- absorption
- there are two main effects of ultrasound on tissue
- thermal (caused by the friction of oscillating particles and the absorption of sound waves)
- non-thermal
- mechanical (e.g., cavitation)
- chemical
- biological
Doppler effect
- describes the change in frequency and wavelength of the received versus transmitted signal caused by the non-zero mutual speed of the transmitter and receiver
- the frequency increases or decreases as the reflector approaches or moves away from the US transmitter
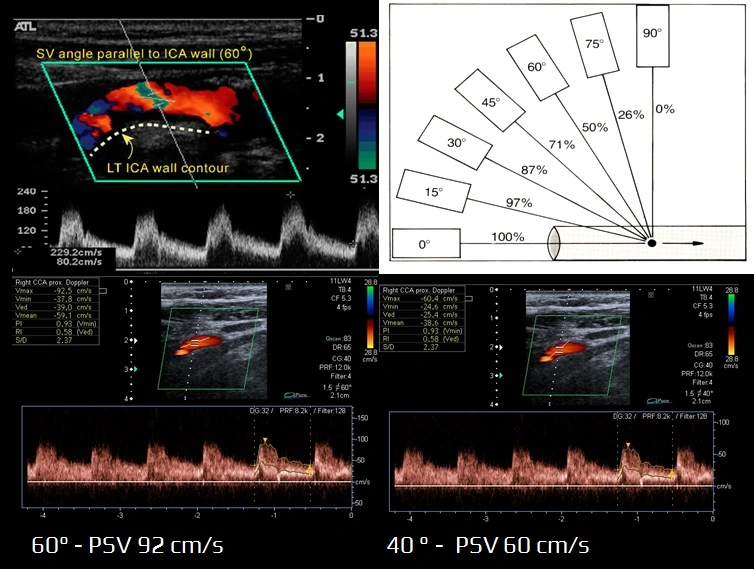
- ∆F=2 x v x frequency x cos α / propagation speed
- frequency shift – the difference between the transmitted and reflected frequency
Pulsed wave (PW) and continuous wave (CW) Doppler
- CW (continuous wave) Doppler transmits US waves and detects a frequency-shifted signal. CW Doppler probes contain two electroacoustic transducers – transmitter + receiver. The sampling volume is fixed by the overlap of the ultrasound beam emitted by the transmitter and the area from which the receiver can detect scattered or reflected waves. The main disadvantage is the existence of a relatively large fixed sampling volume, which makes it virtually impossible to choose the depth at which the velocity is measured
- PW (pulsed wave) Doppler system sends short pulses of US waves. By selecting the time for which the signal is then detected, both the depth and the size of the sampling volume can be adjusted
- the time between the transmission of the pulse and the start of reception determines the distance of the sampling volume from the probe
- the time for which the signal is received defines the size of the sampling volume
- a single electroacoustic transducer is sufficient to transmit and receive ultrasonic waves (PW alternates between transmitting and receiving data)
- the major disadvantage of PW Doppler is aliasing ⇒ change the scale or select a lower frequency of the transducer
Pulse duration, Pulse Repetition Period (PRP), and Pulse Repetition Frequency (PRF)
- pulse duration – the time that the pulse is on; it is determined by the number of cycles and the period of each cycle
- Pulse Duration = (number of cycles x wavelength) / propagation speed
- Pulse Repetition Period (PRP) is the time between the onset of one pulse and the onset of the next one
- Pulse Repetition Frequency (PRF) – the number of ultrasound pulses the device emits and receives per second (PRP/s)
- the limit of the highest measurable speed at a given PRF is often referred to as the Nyquist limit
- The Nyquist frequency corresponds to the value of the Doppler shift frequency (= speed) that is not yet distorted at a given PRF
- it is necessary to adjust the PRF in proportion to the velocity and depth of the vessel under examination
- a disproportionately high PRF rarely allows the display of slow flows, both in color and spectral recording
- the greater the depth of insonation, the lower the maximum PRF can be set
Insonation angel
- if the direction of the ultrasound beam and flow are identical, the angle is 0°, and the Doppler shift corresponds directly to the flow velocity
- the smaller the angle, the more accurate the actual velocity measurement
- with the angle of 90 degrees, the velocity cannot be measured
- when investigating extracranial arteries, an angle of < 60° is usually used
Ultrasound artifacts
- information from the B-mode image or Doppler does not correspond to the anatomical or functional state of the imaged tissue
- depiction of a non-existent structure
- failure to reproduce an existing structure
- failure to display flow
- flow misrepresentation
- artifacts result from limitations of the ultrasound equipment or its incorrect settings; those found in neurosonology include:
- reverberation
- when sound waves bounce back and forth between two highly reflective surfaces
- common examples of tissues where reverberation artifacts can occur include air-filled structures, such as the lungs or the gastrointestinal tract
- mirror image
- occurs when the ultrasound beam encounters a highly reflective structure or interface within the body, such as bone or another strongly reflective tissue, and creates a false, duplicate image
- one common example of a mirror image artifact is seen when imaging the subclavian artery. The ultrasound beam may encounter the ribcage, which reflects the sound waves back to the transducer. The ultrasound system then interprets this reflected signal as coming from a deeper structure, creating a mirror image of the subclavian artery
- occurs when the ultrasound beam encounters a highly reflective structure or interface within the body, such as bone or another strongly reflective tissue, and creates a false, duplicate image
- acoustic shadow
- in cases of extensive tissue density difference, the sound is completely reflected, resulting in acoustic shadowing (typically seen with calcified plaques, bones, or air)
- wrong angle/steering
- aliasing
- artifact that occurs when the frequency shift of the reflected sound waves (Doppler shift) exceeds the Nyquist limit
- this effect causes an incorrect representation of the flow direction
- relative-flow artifact
- it occurs when there is a significant difference in blood flow velocity between two adjacent segments being imaged
- poorly adjusted PRF (scale)
- blooming artifact
- colors are displayed outside the vessel; this is usually caused by an incorrect gain setting, which can be adjusted
- decreasing the Doppler gain minimizes the blooming artifact, but the weakest signal from the smallest vessels may not be detected
- reverberation