SUBARACHNOID HEMORRHAGE
Management of asymptomatic intracranial aneurysm
Updated on 12/06/2024, published on 25/11/2022
- the prevalence of unruptured intracranial aneurysms (UIA) is ~ 0.5-5%
- modern and widely used imaging methods increase the rate of detection of incidental intracranial aneurysms
- multiple aneurysms are found in 20-30% of cases
- modern and widely used imaging methods increase the rate of detection of incidental intracranial aneurysms
- management of unruptured asymptomatic aneurysms is controversial
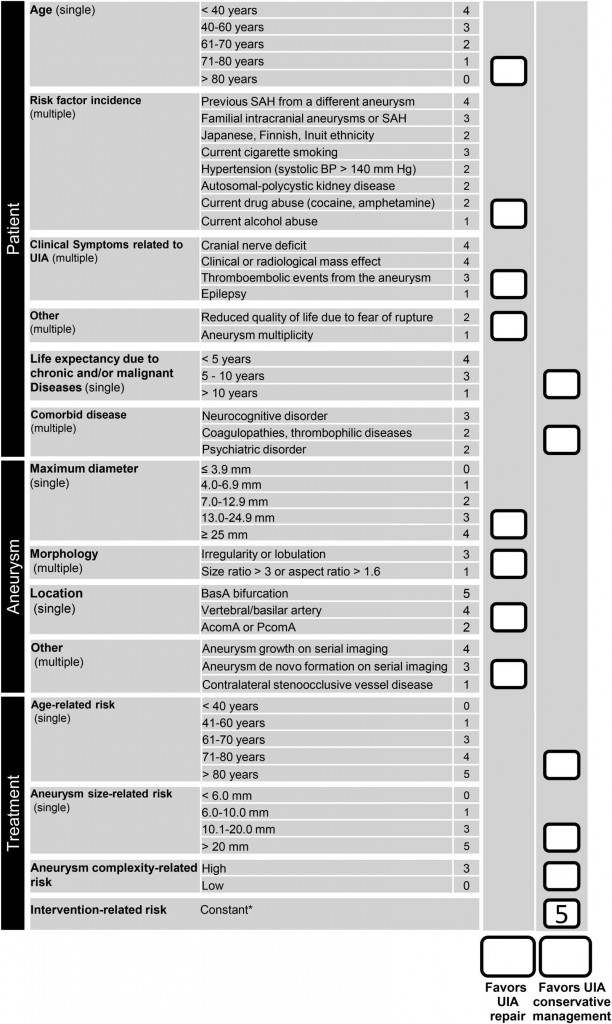
- the decision-making process involves weighing the individual risks of conservative management versus intervention, considering several prognostic factors
- distinguish:
- incidental aneurysm + personal history of SAH from another aneurysm – the highest risk of bleeding (up to 10-fold compared to true incidental aneurysm)
- incidental aneurysm + positive family history of SAH
- incidental aneurysm + negative family and personal history of SAH
Risk factors
| Risk factors for aneurysm formation | |
| Congenital | Acquired |
| AD polycystic kidney disease Fibromuscular dysplasia (MD) hereditary hemorrhagic telangiectasia neurofibromatosis type 1 tuberous sclerosis coarctation of the aorta Ehler-Danlos type IV Pheochromocytoma Marfan syndrome α1-antitrypsin deficiency |
age > 50 years smoking alcohol abuse cocaine or amphetamine abuse atherosclerosis head trauma |
Prognostic factors
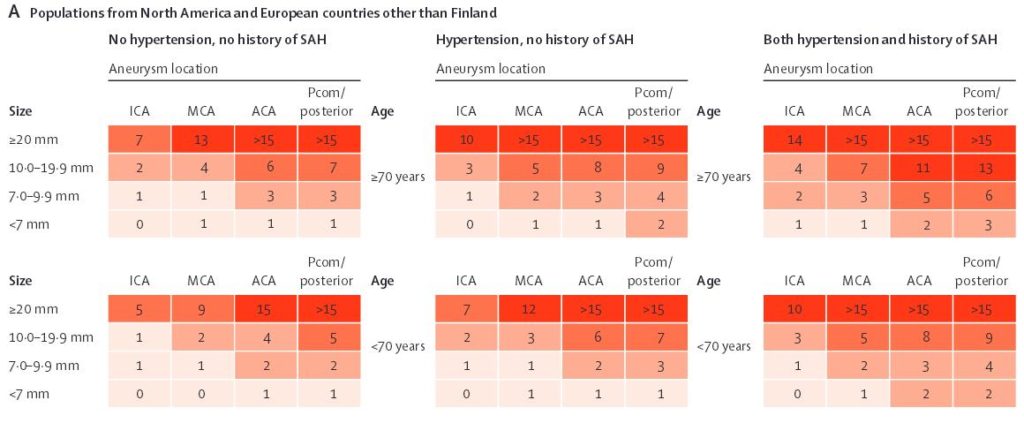
- several factors significantly influence surgical outcome, and these factors should be considered when evaluating treatment alternatives (AHA guidelines 2020)
- these factors can be grouped into patient characteristics (age, symptoms, and medical condition), aneurysm characteristics (size, location,
and morphology), and other factors (hospital and surgical team experience)
Aneurysm characteristics
| Content available only for logged-in subscribers (registration will be available soon) |
Patient characteristics
- age, gender, and comorbidities (⇒ higher surgical risk)
- according to ISUIA, the mortality/morbidity rate was 6.5% for patients < 45 years, 14.4% for patients 45-65 years, and 32% for those over 65 years
- ↑ risk of rupture in decompensated hypertension
- ↑ risk for smokers (up to 4-fold in women) [Ogilvy, 2020]
- ↑ risk in women
- according to ISUIA, the mortality/morbidity rate was 6.5% for patients < 45 years, 14.4% for patients 45-65 years, and 32% for those over 65 years
- race
- history of SAH due to another aneurysm (~10-fold risk)
- family history of SAH (highest risk with ≥ 2 relatives are affected)
- the chance of having an aneurysm correlates with the number of affected first-degree relatives (higher risk for siblings rather than parents or children)
- aneurysms in familial SAH cases are more frequently large and multiple compared to sporadic cases
- patients with familial SAH tend to be younger than those with sporadic cases
Experience of a surgeon/interventional radiologist
- combined morbidity/mortality
Prognostic scores
Diagnostic evaluation
Management
- patients should be informed about the risks and benefits of conservative treatment, clipping, and coiling (AHA/ASA 2009 IIa/B)
- procedure risks:
- post-craniotomy epilepsy
- periprocedural stroke
- aneurysm rupture
- wigh the risk of rupture per year against the patient’s life expectancy
- a randomized trial comparing surgical and conservative management of unruptured aneurysms is not available and cannot be expected in the neart future
- there is a paradox between the fact that, according to ISUIA, the risk of bleeding is low for small aneurysms (<7 mm ⇒ 0.7% per year) and the observation that most bleeding aneurysms in routine practice are in the 7-10 mm range
- it is assumed that some aneurysms undergo a period of higher risk of rupture after their formation, followed by stabilization and transition to a period of low risk – some of these aneurysms are likely to bleed shortly after their formation
- therefore, it makes sense to treat only incidental aneurysms that grow or change their shape
- long-term stable aneurysms have a low risk of bleeding
ISUIA (International Study of Unruptured Intracranial Aneurysms) study is the largest and most widely discussed trial
- n= 4060, three groups: no surgery x clipping x coiling
- the larger the aneurysm, the greater the risk of rupture
- higher risk for aneurysms in PComA, PCA, and basilar artery
- higher risk in patients with previous SAH from another source (approx. 10-fold)
- the prospective arm (1991-1998) had an overall higher incidence of bleeding than the retrospective arm (1970-1991) – 0.8% vs. 0.3%
- according to the prospective data, the risks of clipping and coiling are comparable, but coiling achieved complete obliteration in only 51% of cases
- patients with aneurysms in the anterior circulation (MCA, AComA) had better outcomes when they underwent clipping rather than coiling
- the differences in the results between the retrospective and prospective arms make the generalization of the results problematic
- some authors believe that the ISUIA study underestimates the risk of bleeding, as most ruptured aneurysms fall within the 7-10 mm diameter range
| The 5-year cumulative risk of rupture | ||
| anterior circulation |
posterior circulation (incl. PCoA) | |
| < 7 mm | 0% | 2.5% |
| 7-12 mm | 2.6% | 14.5% |
| 13-24 mm | 14.5% | 18.4% |
| ≥ 25 | 40% | 50% |
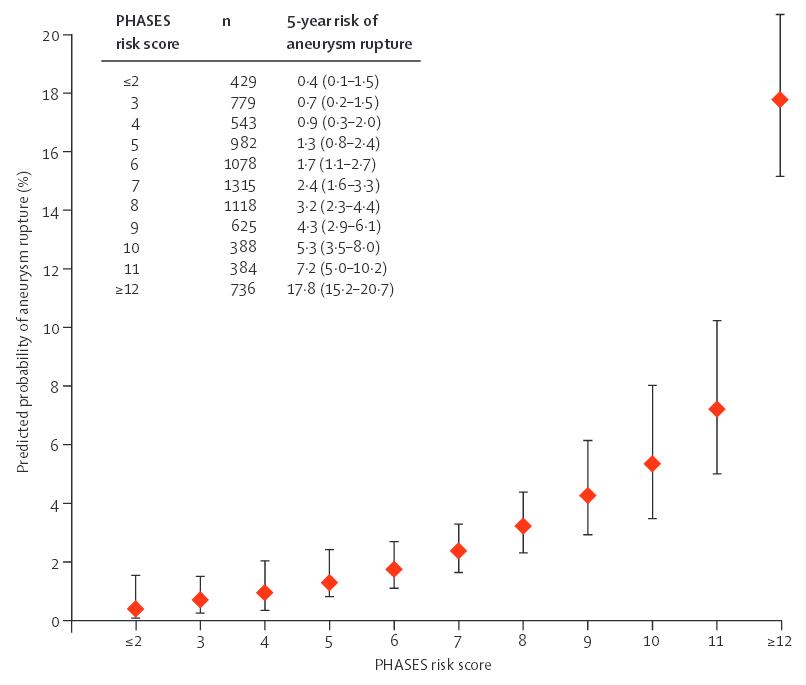
A rather conservative approach
- unruptured, asymptomatic aneurysms < 7mm (especially in the anterior circulation) with no history of SAH
- low PHASES score
- UIA score favoring conservative management
- older age and severe comorbidities
- for large asymptomatic intra-cavernous ICA aneurysms, management is individualized
- monitor patients with 3D TOF MRA → procedure is recommended if aneurysm growth or daughter aneurysm formation is detected
Rather surgical/interventional procedure
| Content available only for logged-in subscribers (registration will be available soon) |
Follow-up
- the first follow-up (MRA/CTA) should be done in 6-12 months after the procedure, then every 1 or 2 years
Screening for asymptomatic aneurysms
- generally not recommended (only grade C recommendations; cost-effectiveness is unknown)
- screening is not recommended in the general population, including smokers and alcoholics (AHA guidelines 2020)
- may be considered in female smokers aged 30-60 years [Ogilvy, 2020]
- no indication for patients with Ehlers-Danlos syndrome type IV (high risk of treatment), neurofibromatosis, or Marfan syndrome
- screening with noninvasive methods is recommended for:
- patients with a history of aneurysmal SAH (↑ risk of new aneurysm formation)
- first-degree relatives of patients with aneurysmal SAH (especially siblings)
- individuals with autosomal dominant polycystic kidney disease (ADPKD)
- choice of screening method
- MRA is preferred (no contrast injection and radiation exposure)
- both CTA and MRA have a risk of missing very small aneurysms (which are typically not treated)
- in patients with previously clipped aneurysms, CTA is preferred (extensive artifacts caused by clips on MRA)
- MRA is preferred in patients who have undergone coiling (as coils produce minimal artifacts on MRA)
- more data are needed to help identify patients who would benefit from screening
Development of new aneurysms
- intracranial aneurysms are not congenital lesions but develop (grow) during life
- patients who have survived an episode of SAH are at increased risk of having a new bleeding episode from:
- treated aneurysm
- already existing, known aneurysm
- new aneurysm
- the annual rate of new aneurysm formation in patients treated for aneurysmal SAH is reported 1-2%
- risk factors include multiple aneurysms at the time of SAH, smoking, and hypertension
- recurrent or de novo aneurysms are found in up to 30% of patients with SAH ⇒ screening should be repeated in a high-risk population with negative baseline imaging