GENERAL NEUROLOGY
Papilledema
Updated on 19/06/2024, published on 20/01/2024
Definition
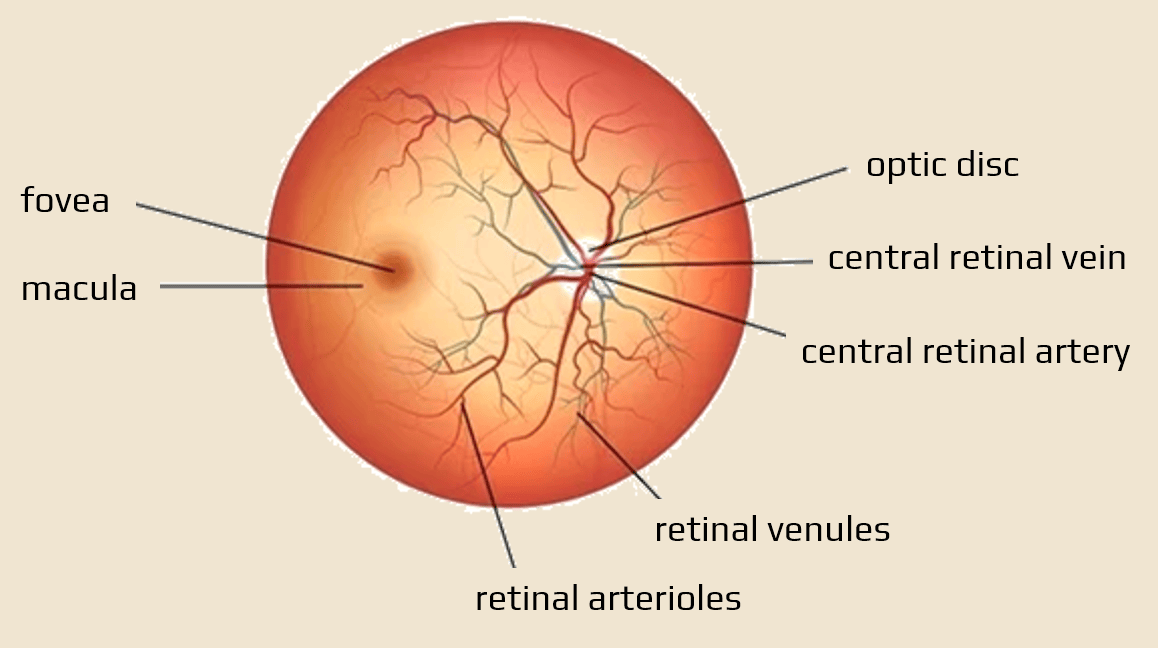
- the optic nerve disc (optic nerve head) is the area of the retina where the optic nerve (optic nerve, CN II) originates
- small, circular, slightly raised area in the retina on ophthalmoscopic examination
- this area lacks light-sensitive photoreceptor cells
- this is where blood vessels enter and exit the retina
- small, circular, slightly raised area in the retina on ophthalmoscopic examination
- papilledema is swelling (edema) of the optic nerve disc due to increased intracranial pressure
- typically bilateral, the disc is ill-defined and prominent; prominence is measured in diopters (3 mm ~ 1D)
- prolonged edema may result in permanent nerve fiber layer loss, leading to progressive visual field loss and central vision loss.
- it is crucial to identify and treat the underlying condition promptly to prevent permanent vision loss and other neurological complications
- it is important to note that ICP can be elevated even in the absence of papilledema
Papilledema x optic disc swelling
Etiopathogenesis
- the optic nerve is sheathed in all three meningeal layers and is continuous with the subarachnoid space of the brain
- intracranial CSF is by this way contiguous with the cerebrospinal fluid (CSF) surrounding the optic nerve, and elevated ICP can be transmitted directly to the optic nerve
- the pathogenesis of papilledema involves compression of nerve fibers by increased CSF pressure in the subarachnoid space
- normal pressure gradient across the intraocular and orbital optic nerve is disrupted, causing retrograde axoplasmic flow across the optic disc, which results in disc edema and optic neuropathy (Trobe, 2011)
- venous stasis, telangiectasia, and hypoxia in the nerve fiber layer are secondary
- generally, papilledema may be caused by any condition leading to intracranial hypertension
- brain tumors
- severe traumatic brain injury
- venous sinus thrombosis
- large ischemic stroke or ICH
- idiopathic intracranial hypertension (pseudotumor cerebri)
- inflammation, etc.
Clinical Presentation
Ophthalmologic Findings
- typically bilateral, usually symmetrical ophthalmoscopic findings (asymmetry may occur in the early stages)
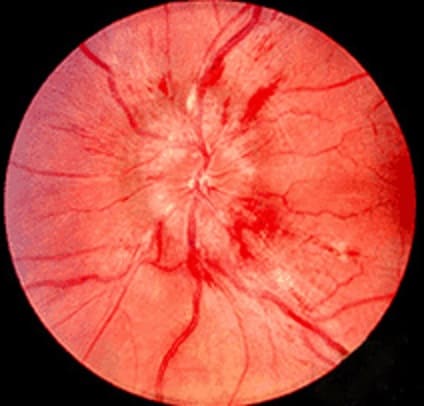
- edema with indistinct disc margins, obliteration of the physiologic excavation, venous stasis, and occasional peripapillary flame-shaped hemorrhages
- dilated and tortuous veins and narrowed arteries
- if the cause is not resolved and the papilledema progresses, hemorrhages and soft exudates become more prominent, and concentric or radial folds (Paton lines) may be observed on the retina
- hemorrhages and exudates are resorbed during the transition to the chronic phase
- in long-term hypertension, papilledema leads to optic nerve atrophy, edema, and hyperemia recede, the disc changes color to greyish white, and the vessels constrict
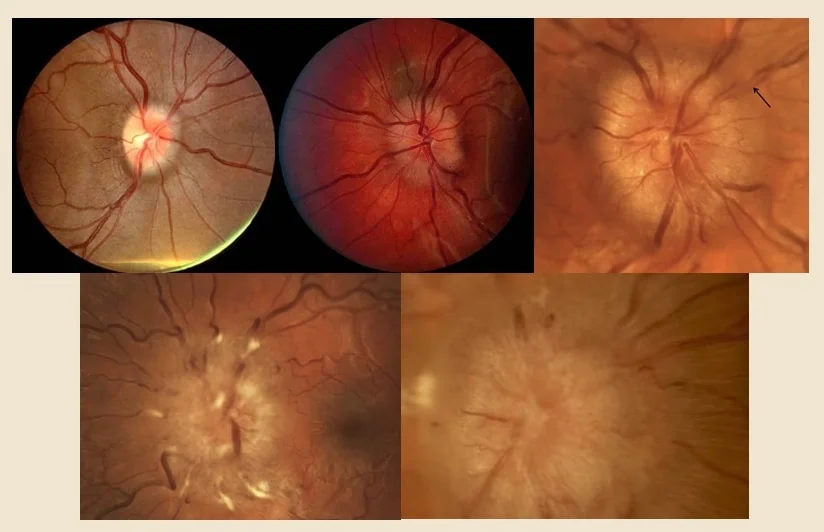
Papilledema can be graded using the Frisén scale but remains subjective
- Grade 0 – a normal optic disc
- Grade I – a C-shaped halo with with preservation of the temporal disc
- Grade II – the halo becomes circumferential
- Grade III – papilledema is characterized by the loss of major vessels as they leave the disc
- Grade IV – papilledema is characterized by the loss of major vessels in the disc
- Grade V – criteria of grade IV + partial or total obscuration of all vessels of the disc
Signs and symptoms
- visual disturbances (early stages of papilledema may be asymptomatic)
- intracranial hypertension syndrome
- headache (commonly in the morning, worsened by coughing and sneezing)
- nausea and vomiting
- double vision (due to the sixth nerve palsy)
- transient blurred vision (usually with eye movements or changes in posture)
- photopsia (flashes of light, often unilateral)
- visual field defects (usually an enlarged blind spot)
Foster-Kennedy Syndrome (FKS)
Diagnostic evaluation
The evaluation is focused on detecting papilledema (including DDx of of conditions that may mimic papilledema) and identifying the underlying etiology
- ophthalmologic examination to confirm papilledema (Frisén grading)
- fluorescein angiography and B-scan ultrasound can also be used to identify other causes for disc edema or conditions that may mimic papilledema
- medical history + physical and neurological examination
- brain and vascular imaging – brain and orbit imaging with CT or preferably MRI + angiography (including venous phase to exclude cerebral venous thrombosis)
- neurosonology
- measurement of the optic disc elevation


- dynamic measurement of the optic nerve sheath diameter (ONSD)
- papilledema takes time to develop + ophthalmoscopy requires skill for accurate identification [Hansen, 1997]
- dilatation of the optic nerve sheath has been shown to be a much earlier and reliable sign of intracranial hypertension
- papilledema takes time to develop + ophthalmoscopy requires skill for accurate identification [Hansen, 1997]
- measurement of the optic disc elevation
- if an intracranial expansive process is ruled out, lumbar puncture with measurement of opening pressure should follow to rule out neuroinfection
- normal opening pressure is < 25 cm H20)
- perform if deemed safe after imaging (assess the risk of herniation)
- analyze protein, glucose, cell count and differential, and cultures
Differential diagnosis of papilledema
The differential diagnosis (DDx) of papilledema involves two steps:
- differentiate papilledema from optic disc edema
- papilledema is bilateral, with increased intracranial pressure (ICP) as the main etiology
- optic disc edema can be unilateral or bilateral, caused by various conditions like optic neuritis, ischemic optic neuropathy, or local eye diseases (see table)
- papilledema is bilateral, with increased intracranial pressure (ICP) as the main etiology
- establish the cause of intracranial hypertension (tumor, infection, stroke, etc.)
- malignant hypertension with retinopathy
- bilateral findings similar to papilledema
- visual field is normal, but visual acuity may be decreased
- vascular changes throughout the retina, crossing phenomenon
- yellow-white exudates
- retinal hemorrhages
- macular star formation (exudates around the fovea)
- central retinal vein occlusion
- unilateral edema
- dilated and tortuous veins
- retinal hemorrhages extending far into the periphery; may be diffuse
- rapid but not sudden decrease in visual acuity
- simultaneous bulbar pain
- unilateral edema
- intraocular neuritis (papillitis)
- difficult to distinguish from papilledema – papillary hyperemia, leakage, radial hemorrhages
- prominence usually < 2D, veins are less dilated
- in neuritis, lesions of the maculopapular bundle and central scotoma occur early
- visual worsening over several days, recovery within a few weeks
- in papilledema, visual acuity remains preserved for a long time
- the lesion is usually unilateral, but bilateral involvement can co-occur or with latency
- often associated with bulbar pain, especially during movement
- etiology is related to infection or multiple sclerosis (MS)
- optic disc appears normal in retrobulbar neuritis
- CN II perineuritis
- inflammation of the optic nerve sheath
- possible disc edema
- pain with eye movement
- possible visual field defects with relative sparing of central visual acuity
- benign papillitis (diabetic papillopathy)
- usually mild decrease in visual acuity; patients often have no complaints, and the finding is incidental
- occasionally, Gunn’s phenomenon (afferent pupillary defect) may be present
- bilateral in ~ 50% of cases
- optic disc findings vary from mild diffuse edema with venous dilation to significant papilledema with cotton-wool spots and hard exudates
- absence of optic disc hemorrhages
- visual field is intact, sometimes with an enlarged blind spot and very rarely with an altitudinal visual field defect
- prognosis is good; visual acuity improves within 2-6 weeks
- pseudopapilledema
- elevated optic nerve disc appearance and blurred margins resulting from congenital variations, optic disc drusen, or tilted optic disc
- retinal nerve fiber layer thickness is normal
Papilledema therapy
- therapy is based on the identified etiology
- papilledema due to intracranial hypertension should address the cause of raised ICP (antiedema medications, surgery)
- venous sinus thrombosis requires anticoagulation or local intrasinus therapy
- if no structural or other causes of intracranial hypertension are detected, the term idiopathic intracranial hypertension (pseudotumor cerebri) is used
- acetazolamide is administered + weight loss is recommended; venous sinus stenting is considered in patients with IIH who have significant transverse venous sinus stenosis
- acetazolamide is administered + weight loss is recommended; venous sinus stenting is considered in patients with IIH who have significant transverse venous sinus stenosis
- symptomatic surgical procedures
- optic nerve sheath fenestration (ONSF) is considered when vision is thought to be severely threatened
- ventriculoperitoneal and lumboperitoneal shunts
- ONSF is an attempt to preserve visual function in patients with vision-threatening papilledema who have failed or are intolerant to maximal medical therapy
- a crucial tool in the acute setting for patients with “malignant” pseudotumor cerebri (extremely high opening pressure +papilledema + poor prognosis with medical therapy alone)
- CSF diversion procedures, such as ventriculoperitoneal shunt (VPS) or lumboperitoneal shunt (LPS), may also be used to lower ICP. While they can be effective in reducing papilledema and preventing vision loss, they carry the risk of brain and spinal surgery and complications related to shunt failure
- unilateral ONSF can result in the resolution of papilledema in both eyes; however, most cases of severe papilledema and vision loss require bilateral ONSF
- the unfenestrated eye typically shows less reduction in papilledema than the operated eye
- some patients may also experience an improvement in headaches
- repeat ONSF may be necessary in patients with recurrent visual disturbance or further visual deterioration after surgery; a ventriculoperitoneal shunt is preferred in such cases
Prognosis
- the prognosis for papilledema varies depending on the underlying cause and duration of the edema
- timely intervention can lead to resolution; delayed treatment may result in permanent visual impairment