ISCHEMIC STROKE / PREVENTION / RISK FACTORS
Arterial hypertension
Updated on 09/07/2024, published on 20/02/2023
- hypertension negatively impacts the cerebral circulation and is a major risk factor for stroke and a leading cause of cognitive decline and dementia
- it may promote the formation of atherosclerotic plaques in cerebral arteries and arterioles
Definition of hypertension
- hypertension is defined as office SBP values ≥ 140 mmHg and/or diastolic BP (DBP) values ≥ 90 mmHg (ESC 2018)
- this is based on evidence from multiple RCTs that treatment is beneficial in patients with these BP levels
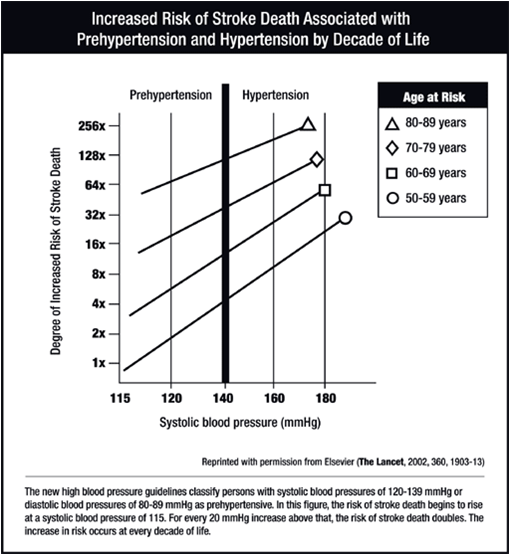
Hypertension and the risk of stroke
- arterial hypertension is the major cardiovascular risk factor
- treatment of hypertension reduces the risk of stroke and cerebrovascular mortality and slows the progression of potential carotid stenosis
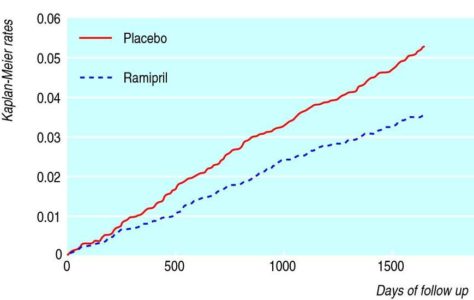
- the HOPE (Heart Outcomes Prevention Evaluation) trial demonstrated the effect of ramipril 10mg in preventing stroke – a 31%/5 year decrease in RR (156 vs. 226 events, ARR 1.5%, p = 0.0002). About 46% of the study population was hypertensive [Bosch, 2002]
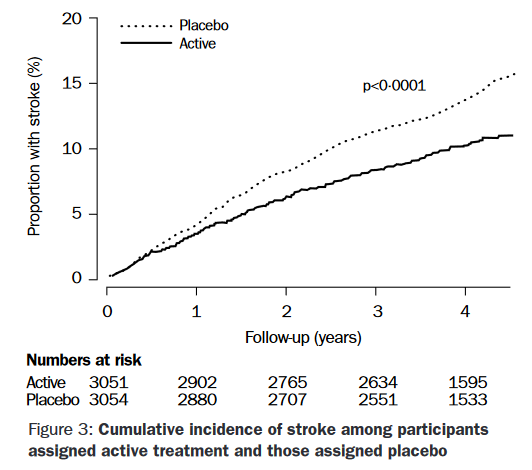
- PROGRESS (Perindopril protection against recurrent stroke study) – 28% rel. stroke risk reduction in 4 years, ARR 4%/4 years
- LIFE (losartan) – 21% stroke risk reduction [Dahlöf, 2002]
- SYST-EUR – 42% stroke risk reduction in elderly patients with systolic hypertension [Staessen, 1997]
- the benefit is also present in people > 80 years of age (HYVET trial)
- in stroke prevention, it is the absolute value of the blood pressure reduction that is important, not the type of antihypertensive drug
- BP control must be consistent to reduce the risk of vascular events [Towfighi, 2014]
- BP lowering in stroke prevention is also beneficial in normotensive patients (HOPE, PROGRESS trials)
- according to the SPRINT trial, CV risk reduction is more pronounced with a target SBP < 120 mm Hg compared to SBP < 140 mm Hg
- other recent trials also support target systolic BP < 120 mm Hg (ACCORD BP, RESPECT, and ESPRIT)
Blood pressure classification
- it is recommended that BP be classified as optimal, normal, high–normal, or grades 1–3 hypertension, according to office BP (ESC 2018 I/A)
| Content available only for logged-in subscribers (registration will be available soon) |
Diagnostic evaluation
- the purpose of the clinical evaluation is to:
- determine the diagnosis and grade of hypertension
- screen for potential secondary causes of hypertension
- identify factors potentially contributing to the development of hypertension (lifestyle, concomitant medications, or family history),
- identify concomitant CV risk factors (including lifestyle and family history)
- identify comorbidities
- establish whether there is evidence of hypertension-mediated organ damage (HMOD) or existing cardiovascular, cerebrovascular, or renal disease
Cut-offs for diagnosis of hypertension
| Definition of hypertension according to different methods of BP measurement | ||
| Category | Systolic BP (mmHg) | Diastolic BP (mmHg) |
| Office BP |
≥ 140 | ≥ 90 |
| ABPM, daytime mean |
≥ 135 | ≥ 85 |
| ABPM, nighttime mean |
≥ 120 | ≥ 70 |
| ABPM, 24h mean | ≥ 130 | ≥ 80 |
| HBPM (home measurement) |
≥ 135 | ≥ 85 |
| all hypertensive patients |
in selected patients |
| medical history and physical examination |
HBPM, ABPM |
| office BP measurement |
ABI |
| urine analysis: microscopic examination; urinary protein by dipstick test or, ideally, albumin: creatinine ratio | fundoscopy |
|
fasting blood glucose and glycated HbA1c
|
microalbuminuria detection |
| Na, K, urea, uric acid |
echocardiography |
| liver function tests | carotid ultrasound |
| creatinine and eGFR | abdominal ultrasound and Doppler studies |
| CBC | cognitive function testing |
| lipids (total cholesterol, LDL, HDL, triglycerides) |
|
| 12-lead ECG |
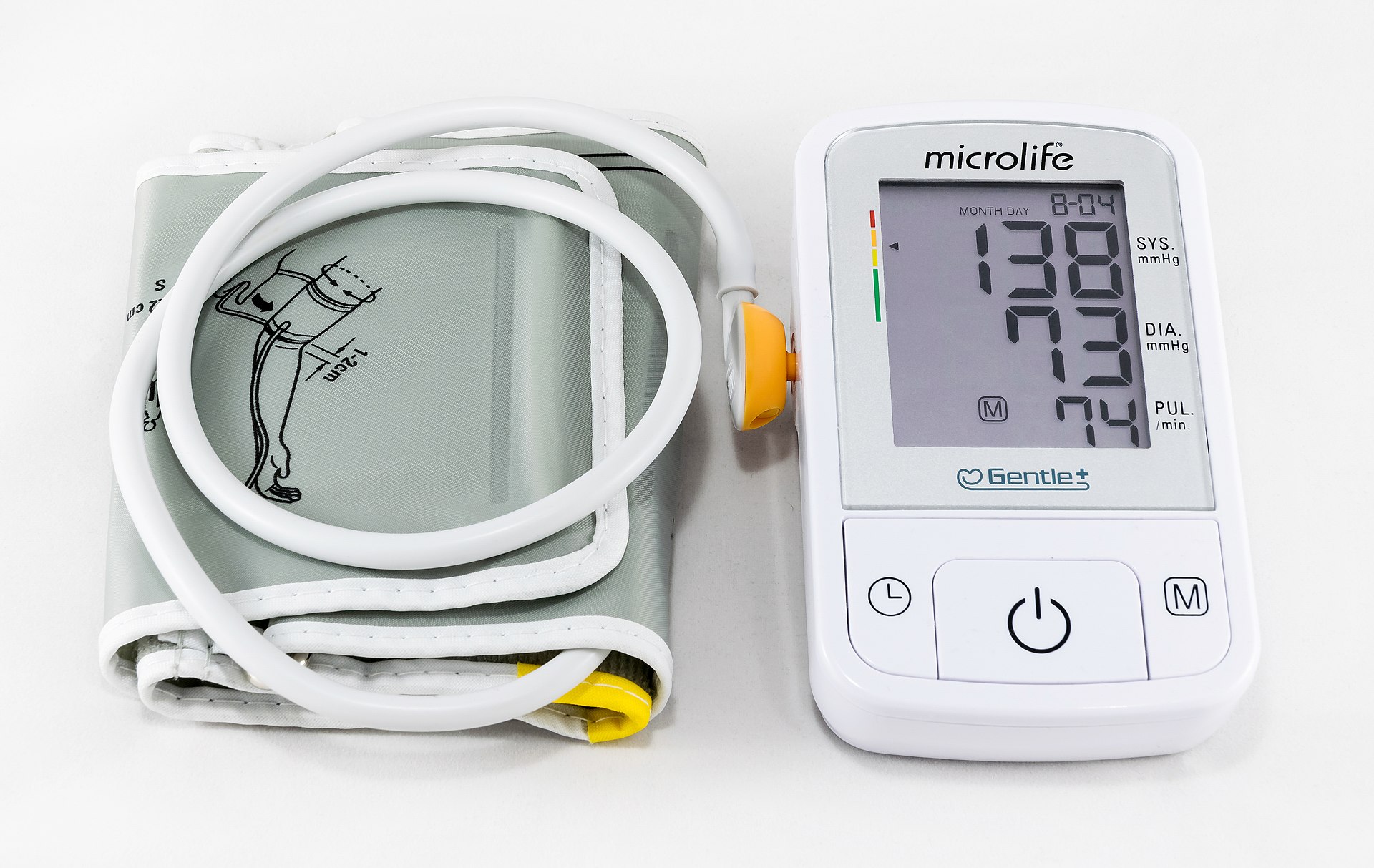
Blood pressure measurement techniques
- a sphygmomanometer is a device used to measure blood pressure
- it consists of:
- an inflatable rubber cuff (of proper size)
- the machine that records the pressure
- the mechanism for inflation (manually operated bulb+valve or an electrically operated pump)
- manual vs. digital
- manual (stethoscope using the auscultatory technique)
- aneroid (mechanical types with a dial) – may require calibration checks
- mercury (gold standard) – the pressure is indicated by a column of mercury; it does not require recalibration and has high accuracy
- digital (oscillometric)
- may use manual or automatic inflation, but both types are electronic, easy to operate without training, and can be used in noisy environments
- calibration is also a concern
- manual (stethoscope using the auscultatory technique)
Cardiovascular risk assessment
- hypertension rarely occurs in isolation and often clusters with other CV risk factors such as dyslipidemia and glucose intolerance (metabolic syndrome)
- the metabolic risk factor clustering has a multiplicative effect on CV risk
- CV risk assessment with the SCORE system (i.e., the likelihood of a person developing a CV event over a defined period) is recommended for hypertensive patients who are not already at high or very high risk due to established CVD, renal disease, or diabetes, a markedly elevated single risk factor (e.g., cholesterol), or hypertensive LVH
Management
Target BP values
- the general principle is to initiate pharmacologic antihypertensive treatment in all patients with SBP ≥140 mmHg or DBP ≥90 mmHg
- target BP value for people at particular risk (including a history of stroke/TIA, diabetes, CKD): < 130/80 mmHg (shift to< 120 mm Hg can be expected)
- supported by data from a large meta-analysis of RCTs [Katsanos, 2016]
- in patients with increased vascular risk, initiate therapy at BP > 130 mmHg!
- in patients with steno-occlusive carotid disease or advanced arteriolopathy, BP should be lowered slowly and cautiously because of the increased risk of hypoperfusion (individual BP target around 135-139/85-89 mmHg )
- the effect of therapy does not depend on the antihypertensive agent but on the blood pressure achieved
- when choosing a drug, consider comorbidities, interactions, and patient preferences
| ESC guidelines 2018 |
|
| WHO guidelines 2022 |
Lifestyle modification and treatment of other vascular risk factors
→ screening and management of other modifiable vascular risk factors
Antihypertensive drugs
| Content available only for logged-in subscribers (registration will be available soon) |