ISCHEMIC STROKE / ACUTE THERAPY
Protocols for thrombolytic therapy
David Goldemund M.D.
Updated on 04/09/2024, published on 06/01/2023
- a complete thrombolytic protocol typically involves:
- confirming the diagnosis of ischemic stroke
- assessing eligibility criteria for IVT
- choosing a thrombolytic agent and the appropriate dose
- monitoring the patient and administering medications to prevent or treat complications
- this chapter focuses on preventing and treating IVT-related complications
- the initial stroke evaluation, thrombolysis procedure, agents used, and contraindications are discussed separately
Blood pressure management during and after thrombolysis
Maintain BP ≤ 180/105 mmHg before infusion and for the next 24 hours
- maintaining adequate blood pressure (BP) is an important preventive measure to minimize the risk of intracranial hemorrhagic complications
- antihypertensive drugs are allowed to achieve the target BP (< 180/110 mmHg)
- if parenteral medication is used, avoid rapid BP drops ( → hypoperfusion → failure of collateral supply)
- do not attempt full BP correction in the first 48 hours (initial target BP ~ 140-160/90-100 mmHg)
- especially with extensive ischemia or significant stenosis, higher BP is required to ensure adequate CPP
- first-line antihypertensive drugs: urapidil (EBRANTIL), enalapril (ENAP), and labetalol (TRANDATE)
- BP monitoring during the first 24-hour period:
- 0-2 hours: every 10-15 minutes, if BP is stable
- in decompensated patients, check BP every 5 minutes until the dose of the antihypertensive drug and BP are stable; consider continuous monitoring (either invasive or non-invasive)
- 2-24 hours: every 30 minutes
- increased frequency of measurement is recommended in case of decompensated hypertension and during parenteral antihypertensive therapy
- 0-2 hours: every 10-15 minutes, if BP is stable
- minimize the duration of parenteral therapy
- after 24 hours, (re)start oral medications (e.g., ACE-I, Ca-blockers, sartans, possibly in combination with diuretics) and gradually reduce parenteral medications → see here
- urapidil (EBRANTIL, TACHYBEN): coarctation of the aorta, grade II and III AV blocks, aortic stenosis. Combination with metoprolol (Betaloc) may enhance the bradycardic effect
- enalapril (ENAP): angioneurotic edema (history), porphyria
- Isosorbide dinitrate (ISOKET): use of phosphodiesterase inhibitors (sildenafil), hypertrophic obstructive cardiomyopathy, constrictive pericarditis
- metoprolol (BETALOC): bronchial asthma, grade II and III AV blocks, significant bradycardia (TF <60/min) before initiation of therapy, inadequately compensated heart failure, sick sinus syndrome
- sodium nitroprusside (NIPRUSS): aortic coarctation, Leber optic atrophy, tobacco amblyopia, vitamin B12 deficiency, metabolic acidosis, hypothyroidism, intrapulmonary AV shunts, severe hepatic failure, sildenafil therapy, hypotension, severe stenotic valve defects, hypertrophic obstructive cardiomyopathy
SBP 180-229 mmHg / DBP 105-139 mmHg
- urapidil (EBRANTIL, TACHYBEN), labetalol (TRANDATE), enalapril (ENAP), esmolol (BREVIBLOCK)
SBP > 230 mmHg / DBP > 140 mmHg
- in combination with the antihypertensive drugs listed above
- Isosorbide dinitrate (ISOKET 0.1%) or sodium nitroprusside (NIPRUSS)
- both drugs act immediately
- FUROSEMIDE
- the onset of action within 30 min
Management of thrombolysis complications
Hypofibrinogenemia
|
- usually, there is only a small decrease in the levels of fibrinogen and other clotting factors in the blood; it enables emergency surgery to be performed shortly after completion of IVT
- in cases of hypofibrinogenemia, there is little correlation between low fibrinogen levels (normal range 1.8-4 g/L) and the risk of intracranial hemorrhage (ICH)
- increased bleeding risk usually occurs at levels < 1 g/L
- spontaneous correction of hypofibrinogenemia within 24-48 hours is common
- in case of bleeding or persistent low levels (< 1 g/L), substitution may be required:
Minor bleeding (at the injection site, gingival bleeding, hematuria, etc.)
|
- patients treated with IVT should be monitored for any bleeding at the injection site, from the gums, gastrointestinal tract (GIT), urogenital tract (UGT), etc.
- minor bleeding (e.g., gingival bleeding) does not require discontinuation of IVT
- should bleeding progress, check the hemocoagulation and platelet count and proceed to the next section
- to assess whether the thrombolytic effect persists, assess:
- thrombin time (TT) and plasma fibrinogen levels
- fibrin degradation product (FDP) levels
- euglobulin fibrinolysis (time-consuming test, short version takes ~ 60 minutes)
Massive extracerebral hemorrhage, suspected intracerebral hemorrhage |
- immediately stop tPA infusion
- check blood samples (CBC, coagulation, fibrinogen)
- perform head CT scan
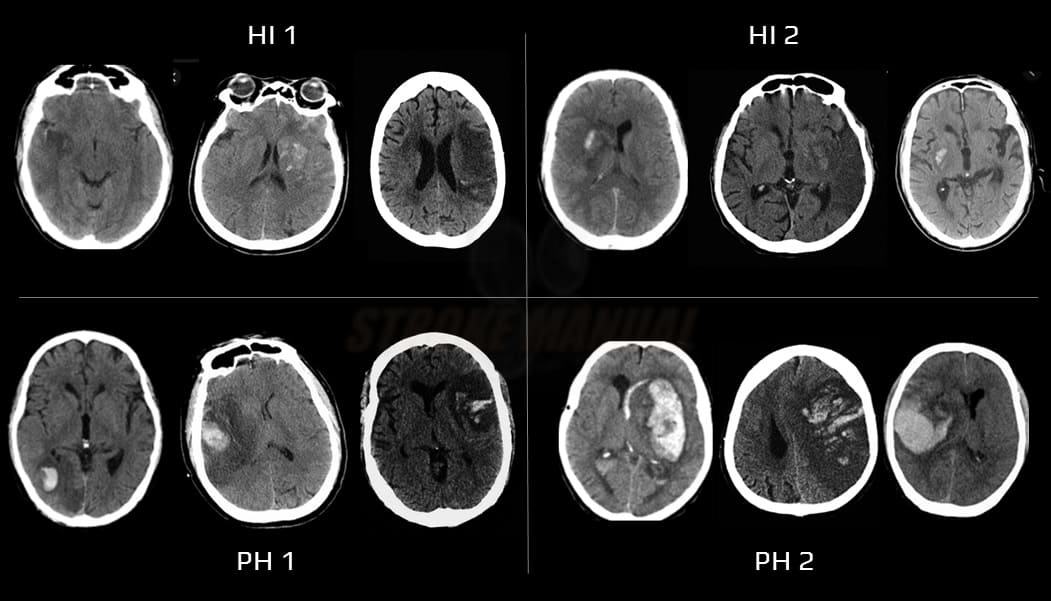
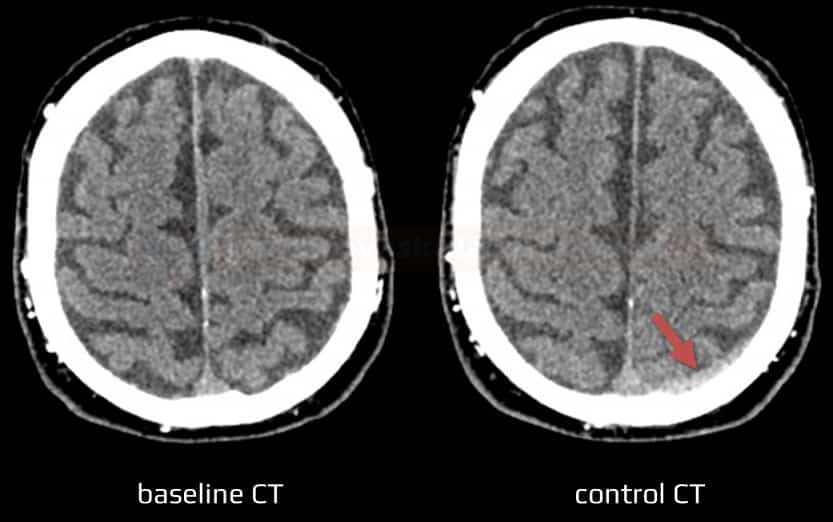
- hemorrhagic infarction → classification of IC bleeding after TL
- SAH, SDH/EDH
- substitution of clotting factors is usually not necessary due to the short biological half-life of alteplase
- the following drugs may be administered if needed:
Clotting factors substitution
Syntetic antifibrinolytics
(Exacyl / Traxyl / Transamin) usually 1ml/100mg
- slow IV injection 10mg/kg (vial=5mL/500 mg) over 10 min every 8 hours (infusion speed < 100mg/min to avoid hypotension)
- cardiac surgery – 10-20 mg/kg bolus + continuous IV infusion 1-2 mg/kg/h
- reduce dose in nephropathy
- no dosage adjustment is required for hepatic impairment
(Trasylol / Antilysin)
- vial = 10 000 TIJ (trypsin inhibitory units) / 1 mL
- a bolus of 100 000 TIJ (10 mL) IV followed by infusion of 200-300 000 TIJ (diluted in 5% glucose) within 3-4 hours
- non-specific inhibitor – interferes with the active center of serine proteases, inhibits kallikrein, trypsin, urokinase, and elastase, interferes with the contact system (f.X), inhibition of f.XII and thrombin
(Amicar)
tPA-related orolingual angioedema
|
- t-PA-related orolingual angioedema is more common in patients who take ACE inhibitors (ACEIs) (RR 13.6!) and in patients with frontal lobe and operculo-insular lesions (RR 9) [Hill, 2003] [Fröhlich, 2019]
- incidence ~1-5%
- often, half of the tongue (contralateral to the lesion) or only the lip is affected
- it is likely to be an anaphylactoid (not anaphylactic) reaction triggered by the activation of the complement system and the kinin cascade by plasmin
- complement activation causes mast cell degranulation with histamine release, leading to vasodilation
- the activation of the kinin cascade leads to increased levels of bradykinin, which also causes vasodilation (the higher prevalence in patients taking ACEIs may be due to the inhibition of plasma kinases responsible for removing bradykinin) [Gauberti, 2018
| Content available only for logged-in subscribers (registration will be available soon) |
Management
-
discontinue tPA infusion and administer:
- H1-antihistamines
- H2-blockers (such as famotidine) can be used in conjunction with H1-antihistamines to provide additional control of histamine-mediated symptoms
- steroids (IV methylprednisolone)
- epinephrine in severe cases
- H1-antihistamines
(Benadryl) 25-50 mg IV, repeated every 4-6 hours as needed
(Prothiazine, Phenergan) 1 amp/25mg IV injection
(Famosan, Famox, Quamatel) 20 mg IV injection
(Solumedrol)
-
- steroid dose: 125-250 mg (1-2 mg/kg) initially IV, followed by 40-60 mg orally every 6 hours, tapered over several days as symptoms resolve
(Adrenalin)
-
- adult dose: 0.3-0.5 mg (0.3-0.5 mL of a 1:1000 concentration) IM or SC
- may be repeated every 5-15 minutes for up to 3 doses
(Firazyr)
-
- a selective bradykinin B2 receptor antagonist that may be used for angioedema associated with ACE-I
- dose: 30 mg/3mL SC in the abdominal area; can be repeated at 6 and 12 hours
- airway management
- perform orotracheal intubation (OTI) or tracheostomy if conservative treatment fails
- edema extending to the larynx and pharynx increases the risk of severe respiratory distress
- supportive care – oxygen, IV fluids, and monitoring in an intensive care setting
Thrombolysis after previous angioedema
- thrombolysis after a prior episode of TPA-related angioedema requires caution due to the potential risk of recurrence but is not absolutely contraindicated
- if thrombolysis is deemed necessary, close monitoring for signs of angioedema is essential; have medications (such as antihistamines, corticosteroids, epinephrine) and airway management equipment readily available
- some guidelines suggest pretreatment with corticosteroids and antihistamines
- direct mechanical thrombectomy may be considered if the patient has a large vessel occlusion and the procedure is readily available
- if possible, discuss the risks and benefits with the patient and/or family members
- key considerations
- time elapsed since the previous angioedema attack – > 1 year ago might be associated with lower risk
- severity of previous reaction – mild angioedema may pose less risk than life-threatening reactions
- cause of angioedema – known allergen vs. unknown cause (possibly tPA)
- stroke severity – potential benefits of thrombolysis might justify the risk in moderate-severe stroke
- are alternative treatment options available?
Less frequent adverse events
|
- nausea, vomiting, chills, fever, urticaria, headache, confusion
- treatment is symptomatic; the decision to discontinue tPA infusion depends on the severity of the adverse events