CEREBRAL VENOUS SINUS THROMBOSIS
Endovascular and surgical treatment of cerebral venous thrombosis
Updated on 27/07/2024, published on 20/11/2022
- in the clinical trials, 10-15% of the patients treated with heparin had a poor outcome
- patients with extensive thrombosis may benefit from recanalization treatment:
- if no improvement is observed with anticoagulation treatment
- in patients with rapidly deteriorating consciousness due to extensive thrombosis and/or involvement of the deep venous system
- if no improvement is observed with anticoagulation treatment
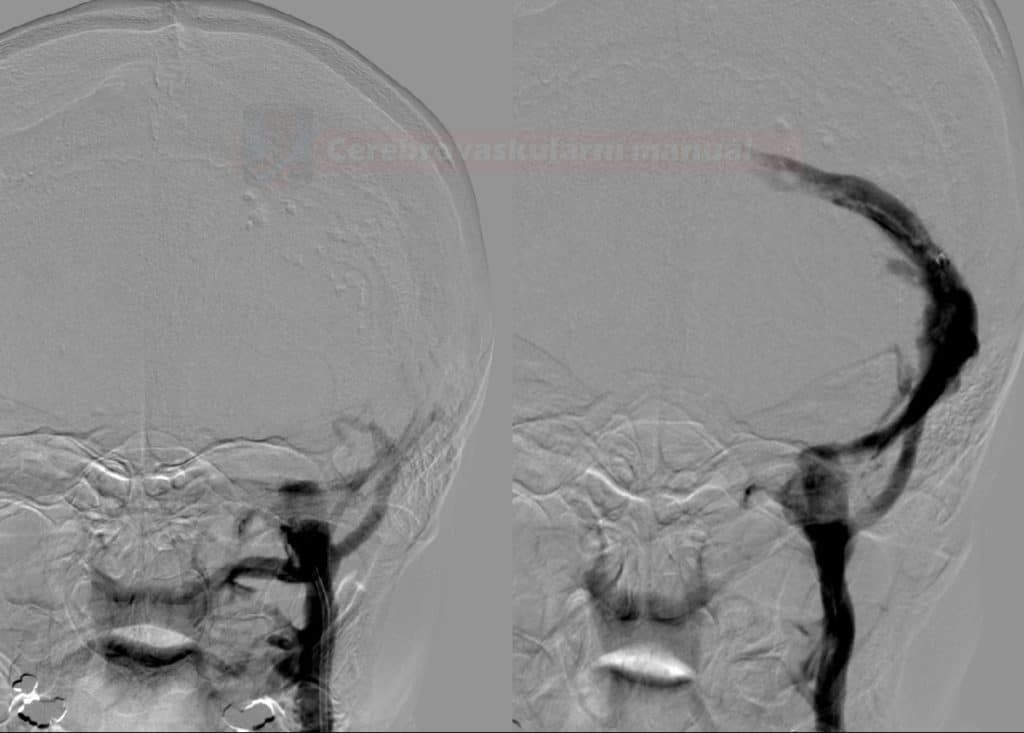
- endovascular therapy aims to re-establish anterograde venous outflow in the targeted sinus and alleviate malignant venous congestion
- recanalization (complete or partial) is associated with an improved outcome compared to those without recanalization
- however, the randomized TO-ACT trial did not demonstrate a significant benefit of interventional therapy over standard medical therapy
Intravenous thrombolysis
- intravenous thrombolysis (IVT) is rarely used; treatment results are inconclusive, and IVT seems to increase the risk of bleeding
- dosage is not standardized (and is not even discussed in recent guidelines)
- according to small studies, a continuous infusion of 1-2 mg/h is used
- the duration of thrombolysis is unclear ⇒ 24-48 h may be considered
- insufficient data exist to recommend this treatment, particularly in patients expected to have a favorable prognosis (ESO guidelines 2017)
Local thrombolysis / mechanical recanalization
- local intra-sinus therapy should be performed in centers with expertise in endovascular treatment
- advisable in extensive venous thromboses where no significant effect of anticoagulation is seen or can be expected
- in a systematic review including 10 studies comprising 339 patients who underwent EVT for CVT, the authors found a complete and partial postoperative recanalization in 90.0% of patients (Paybast, 2022)
- in a systematic review including 10 studies comprising 339 patients who underwent EVT for CVT, the authors found a complete and partial postoperative recanalization in 90.0% of patients (Paybast, 2022)
- the theoretical advantage of local thrombolysis is that the drug is delivered where needed and downstream from cerebral venous—often hemorrhagic—infarcts
- mechanical methods result in more rapid recanalization and increase the surface of the thrombus exposed to thrombolytics
- there is no current evidence to determine which EVT technique (e.g., stent retriever, microcatheters, aspiration catheters, aspiration pump systems) is superior to other
therapeutic strategies - guidelines do not address endovascular treatment in depth (no indication criteria or technical implementation are stated) (ESO guidelines 2017) (AHA guidelines, 2024)
Intrasinus therapy may be offered in these cases:
- symptoms have not improved significantly or have worsened during anticoagulation treatment
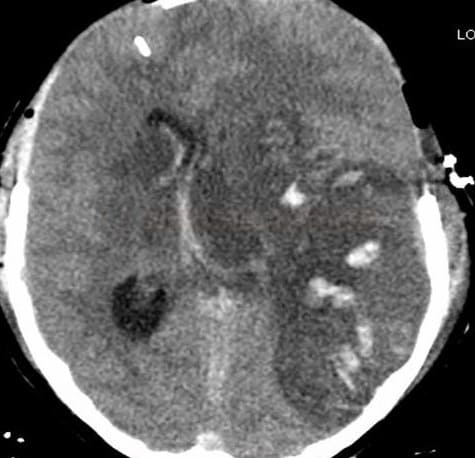
- extensive thrombosis on baseline imaging (especially affecting the deep venous system) with severe neurological deficit
- assumed poor prognosis because of altered mental status (cognitive disturbances including abnormal alertness and orientation or coma)
Local (intra-sinus) thrombolysis (LIST)
- randomized trials are lacking, but the efficacy of endovascular therapy is supported by case series
- analysis of several cohorts of 235 patients [Llyas, 2017]
- a review encompassed 185 patients undergoing mechanical recanalization, achieving partial or complete recanalization in 95% of cases (AngioJet was used in 40% of cases) [Siddiqui, 2015]
- the presence of ischemic and/or hemorrhagic lesions is not a contraindication to LIST
- retrograde access, mostly via the femoral vein, is used; a microcatheter is inserted into the affected sinus for continuous infusion
- patients are usually heparinized throughout the procedure, but no standardized protocol exists (local or systemic? UFH or LMWH? what dose?)
- different tPA dosing regimens exist (total dose 8-300 mg, median dose 78.4±64.7mg, median therapy duration 41±49h) [Canhao, 2003]
(Actilyse / Activase)
- bolus 2-10 mg into the thrombus, then continuous infusion of 1-2 mg/h (Mathukumalli, 2016) [Lee, 2018]
- bolus 10 mg into the thrombus, followed by 15 mg/h for 3 hours and then 5 mg/h (max 100mg/day) [Kim, 1997]
- usually given for 24-48 h (max. 200 mg in total)
- 200-1000 IU/h administered together with tPA serves to flush the catheter and prevent pulmonary embolism
- alternatively, systemic heparin/LMWH administration may be continue (no data are available on safety/efficacy) (Stam, 2008)
- repeat angiography every 12-24 hours to monitor response to local thrombolysis
- thrombolysis may be combined with thrombectomy (see below)
- continue standard anticoagulant therapy after completion of the procedure
Mechanical thrombectomy
- thrombolysis can be combined with mechanical methods such as thrombus disruption, thrombectomy, or angioplasty
- thrombectomy can also be performed as a standalone primary procedure, notably in cases with extensive bleeding [Lee, 2018]
- several devices are used:
- AngioJet
[Curtin, AJNR 2004]
- balloon thrombectomy (Fogarty)
- direct aspiration [Jankowitz, 2012]
- stent retrievers [Chen, 2017]
- Penumbra aspiration thrombectomy [Mammen,2017]
- promising were results reported even without thrombolysis
- AngioJet
Surgery
External ventricular drainage (EVD)
- consider in patients with developing obstructive hydrocephalus; however, data are insufficient to make a formal recommendation (ESO guidelines 2017)
- consider carefully as surgery requires temporary interruption of anticoagulant/thrombolytic therapy
Decompressive craniectomy
- decompressive craniectomy, with/without hematoma evacuation, is typically reserved for patients with acute severe CVT and parenchymal lesions with impending herniation
- it is considered a life-saving procedure that increases the chance of a favorable outcome even in the most severe CVT cases
- DECOMPRESS2 trial showed that 2/3 of patients with severe CVT survived, and more than one-third were independent 1 year after decompressive surgery
- better results can be expected in:
- non-comatose young patients with unilateral lesions
- surgery within 48 hours of admission
- factors associated with poor outcome:
- age >50 years
- midline shift >10 mm
- total effacement of basal cisterns
- there is insufficient data to determine the preferred method between hemicraniectomy and endovascular treatment, as well as how and when to combine them
Optic nerve decompression
- indicated in case of substantial papilledema and imminent blindness
- optic nerve sheath fenestration (ONSF) alleviates intraneural pressure and facilitates venous outflow
- the procedure requires interruption of anticoagulation/thrombolytic therapy
- intervention may result in visual improvement and resolution of papilledema [Murdock, 2014]


![Endovascular treatment modalities in cerebral venous thrombosis [Lee, 2018] Endovascular treatment modalities in cerebral venous thrombosis [Lee, 2018]](https://www.stroke-manual.com/wp-content/uploads/2021/04/endovascular_therapy.jpg)