SUBARACHNOID HEMORRHAGE
Brain aneurysm diagnosis
Updated on 09/03/2024, published on 30/03/2021
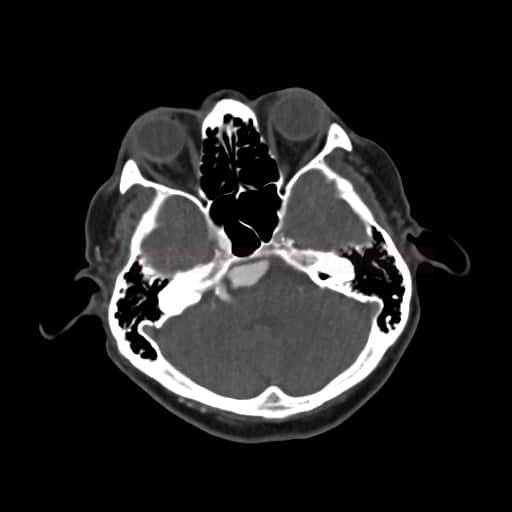
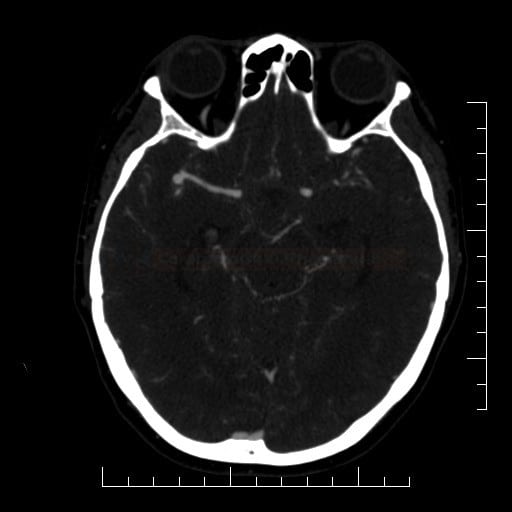
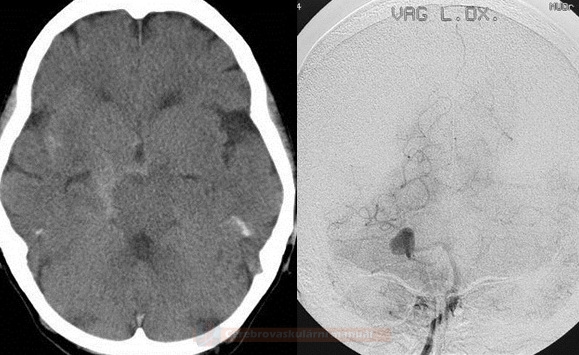
- in each patient with a subarachnoid hemorrhage (SAH), it is necessary to identify the source by examining the arterial circulation
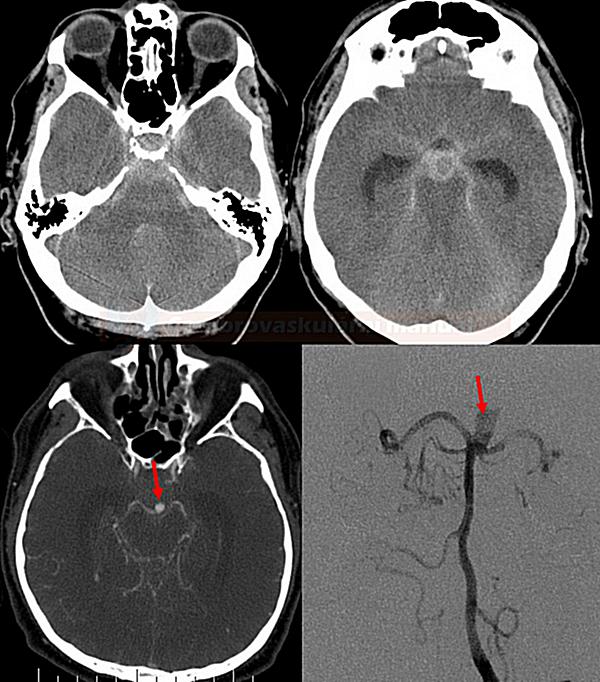
- CT angiography (as part of the usual baseline imaging) serves as the primary diagnostic modality for aneurysm detection in the acute setting; if negative, DSA is usually performed
- in isolated perimesencephalic SAH (PMSAH), the cost-effectiveness of subsequent DSA is questionable [Kalra, 2015]
- a potential source of bleeding in the spinal cord should be excluded when SAH is localized to the posterior fossa
| Clinical manifestation |
|
| Size |
|
| Neck width |
|
| Shape |
|
| Localization |
|
| Etiology |
|
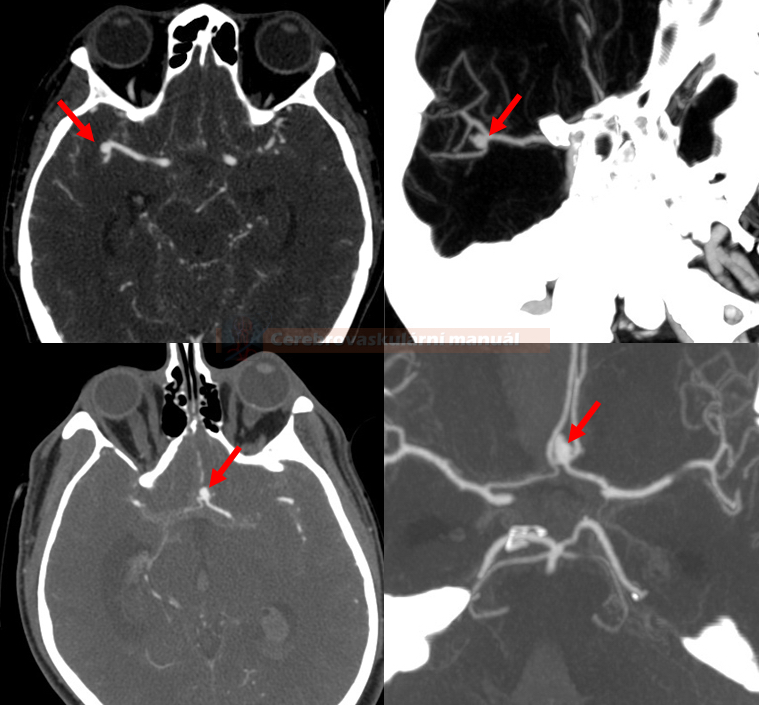
CT Angiography
- CTA sensitivity is ~ 95% for aneurysms > 5mm
- sensitivity decreases with smaller aneurysms (< 5mm ~ 64-83%)
- always evaluate MIP projections, 3D reconstructions, and source images
- evaluation near the skull base (e.g., intraosseous part of the ICA) can be tricky
- adjust the window parameters (width/level) accordingly
- utilize methods to remove bone, such as subtraction (matched mask bone elimination) ) and manual or automated bone editing
- CTA is suitable for screening at-risk groups and for monitoring asymptomatic or treated aneurysms (AHA guidelines 2020)
- in diffuse SAH with negative CTA, always proceed with DSA
- with negative CTA, aneurysm detection on subsequent DSA is reported in 5% of cases
- according to some reports, false-negative findings on CTA occur in up to 20% of cases [Agid, 2009]
- in convexial SAH, search for signs of vasculitis and perform DSA if CTA is negative
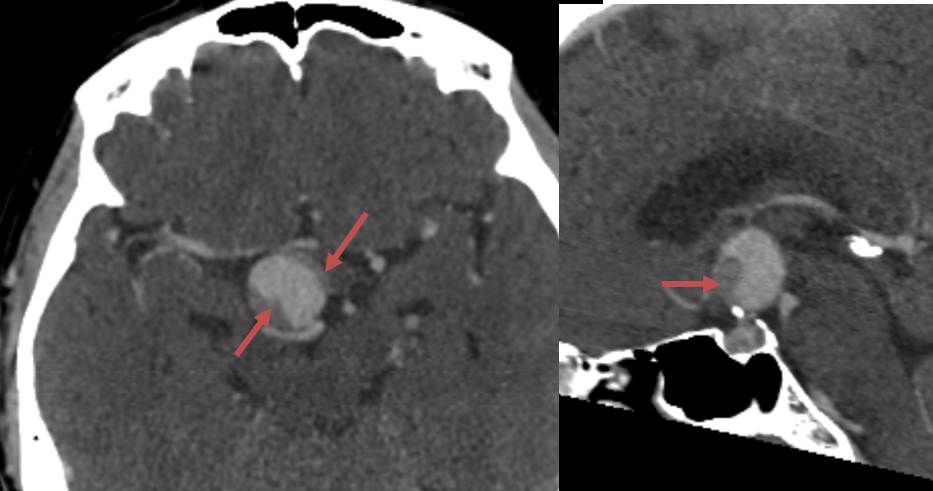
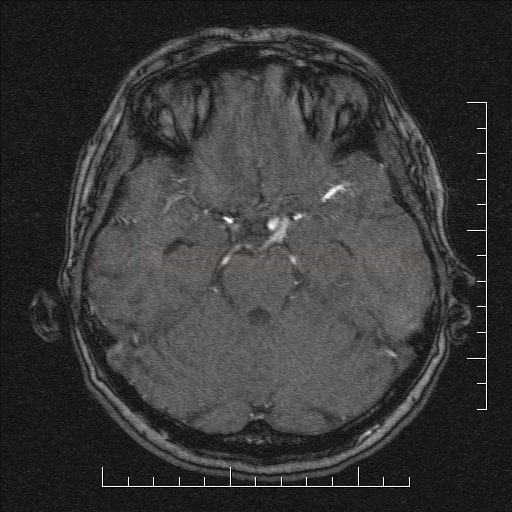
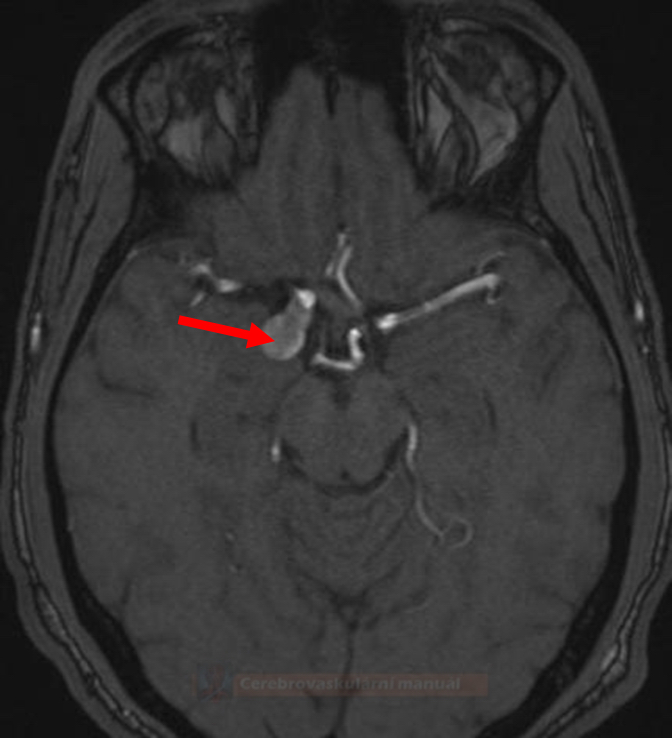
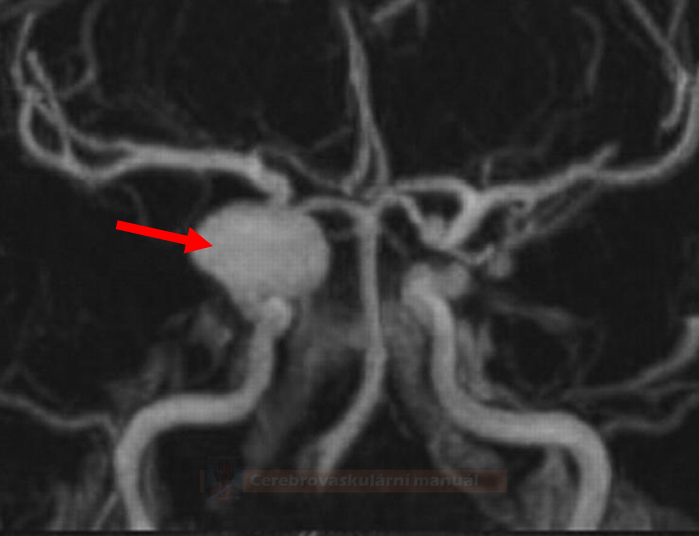
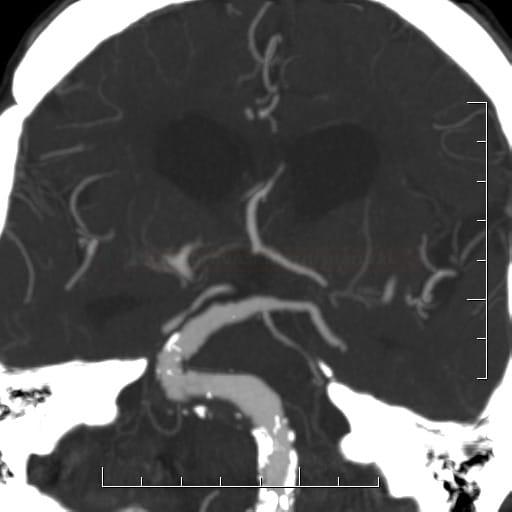
MRI and MR Angiography
- intracranial MRA uses the time-of-flight (TOF) method; 3T scanners have higher sensitivity
- sensitivity 85-100% for aneurysms > 5mm [Sailer, 2013]
- sensitivity decreases with aneurysms < 5mm (56%)
- MRA is a suitable method for screening and follow-up (though, compared to CTA and DSA, MRA is less sensitive for detecting subtle changes in aneurysm size)
- MRI + MRA can identify thrombosed aneurysms that DSA may miss and can help to assess the extent of thrombosis)
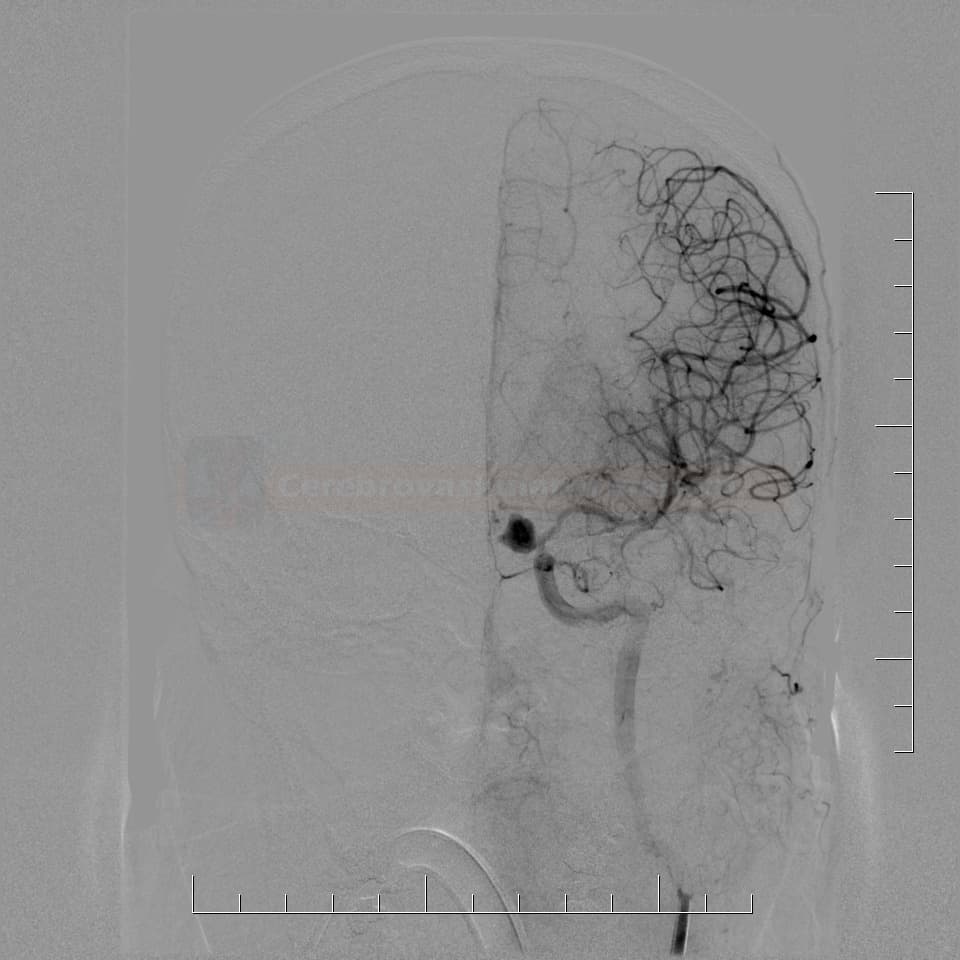
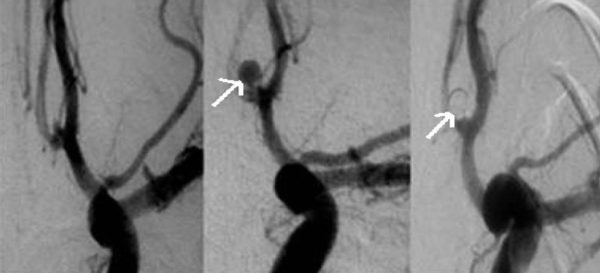
Digital Subtraction Angiography (DSA)
Technique
| Content available only for logged-in subscribers (registration will be available soon) |
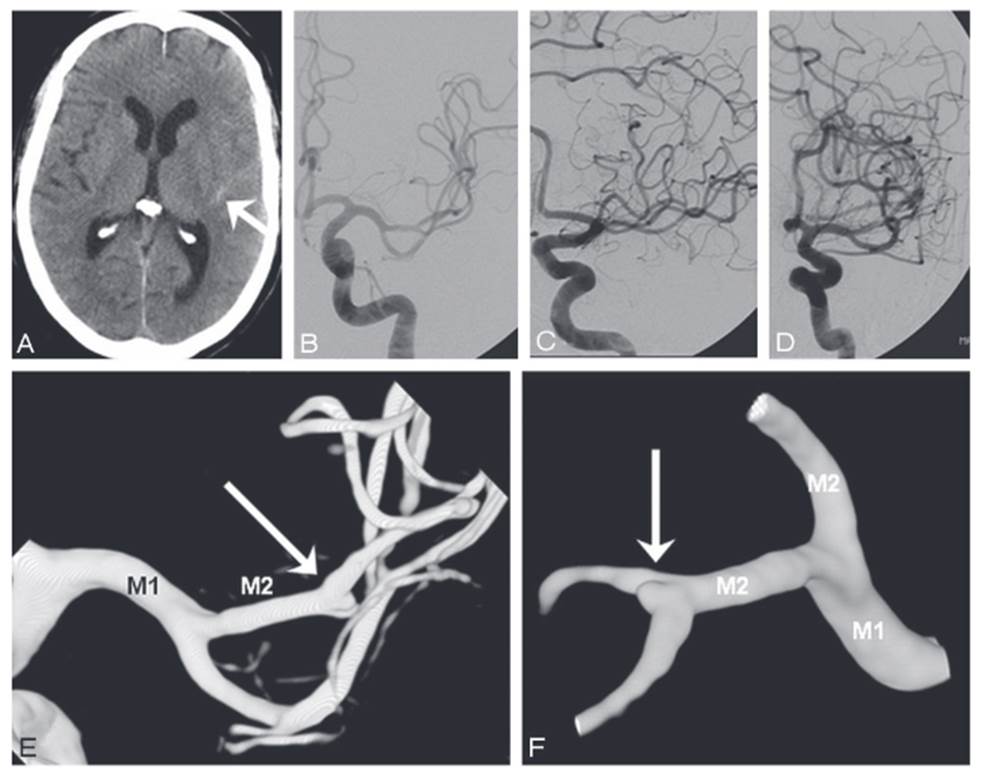
Images assessment
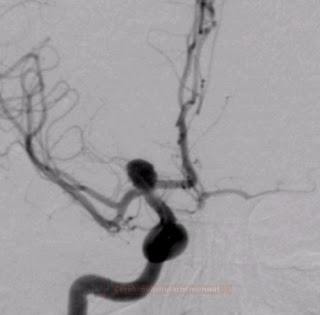
- look for aneurysm(s) or other sources of bleeding
- assess the type and location of the aneurysm (shape and size of the sac, type and width of the neck, vessel geometry, and relationship to the parent artery and surrounding branches)
- exclude multiple aneurysms and other concomitant vascular malformations
- with multiple aneurysms (present in up to 15% of cases), estimate which aneurysm was the probable source of the current bleeding
- assess the overall intracranial vascular status:
- the presence of vasospasms
- the patency of the circle of Willis (is the collateral circulation sufficient if occlusion of the feeding artery is required?)
- the general condition of the intracranial circulation (atherosclerotic changes and stenoses in the access route and the feeding artery)
- if occlusion of the feeding artery is considered, add functional tests
- Matas test – manual compression of the artery with simultaneous injection of the contralateral ICA or ipsilateral vertebral artery to assess the functionality of the collateral circulation
- Balloon Test Occlusion (BTO) is more reliable because manual external compression is usually inadequate
- should not be performed in acute SAH as heparinization is required during the procedure
- Matas test – manual compression of the artery with simultaneous injection of the contralateral ICA or ipsilateral vertebral artery to assess the functionality of the collateral circulation
Further procedures after negative initial examination
Perimesencephalic SAH
- if CTA and DSA are negative, then repeat DSA is not needed
[Huttner,2006]
Non-perimesencephalic SAH
- source of bleeding is not found in 15-30% of SAH patients
- in Sylvian and interhemispheric fissure SAH, the presence of an aneurysm is highly probable – false-negative initial examination may have the following reasons:
- poor imaging quality, motion artifacts
- incomplete examination
- failure to detect aneurysm on standard projections
- thrombotic occlusion of the aneurysm
- vasospasms (VSP)
- human error
- indication and number of DSA examinations are discussed
- the rate of aneurysm detection on repeat DSA is about 4-20%, and it is higher in cases with VSP on initial DSA [Yu, 2012] [Ringelstein, 2013]
- the risk of false-negative DSA can be reduced using 3D DSA and oblique projections
- indications for repeat DSA:
- detection of vasospasms on the initial DSA or poor quality of the initial study
- second DSA should be performed after 2-6 weeks (use TCD/TCCD to rule out vasospasms before DSA)
- perform CTA/MRA (+ GRE sequence) instead of the third DSA
- consider the potential source of bleeding in the spinal canal (in posterior fossa SAH cases)