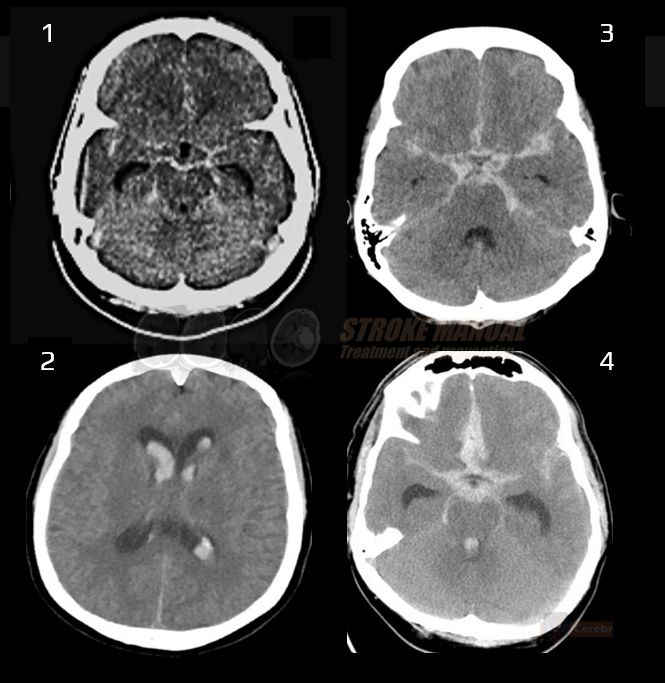
SUBARACHNOID HEMORRHAGE
Definition and etiology of subarachnoid hemorrhage
Updated on 29/04/2024, published on 29/03/2021
Definition, epidemiology
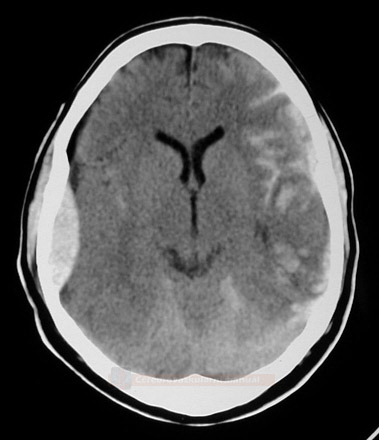
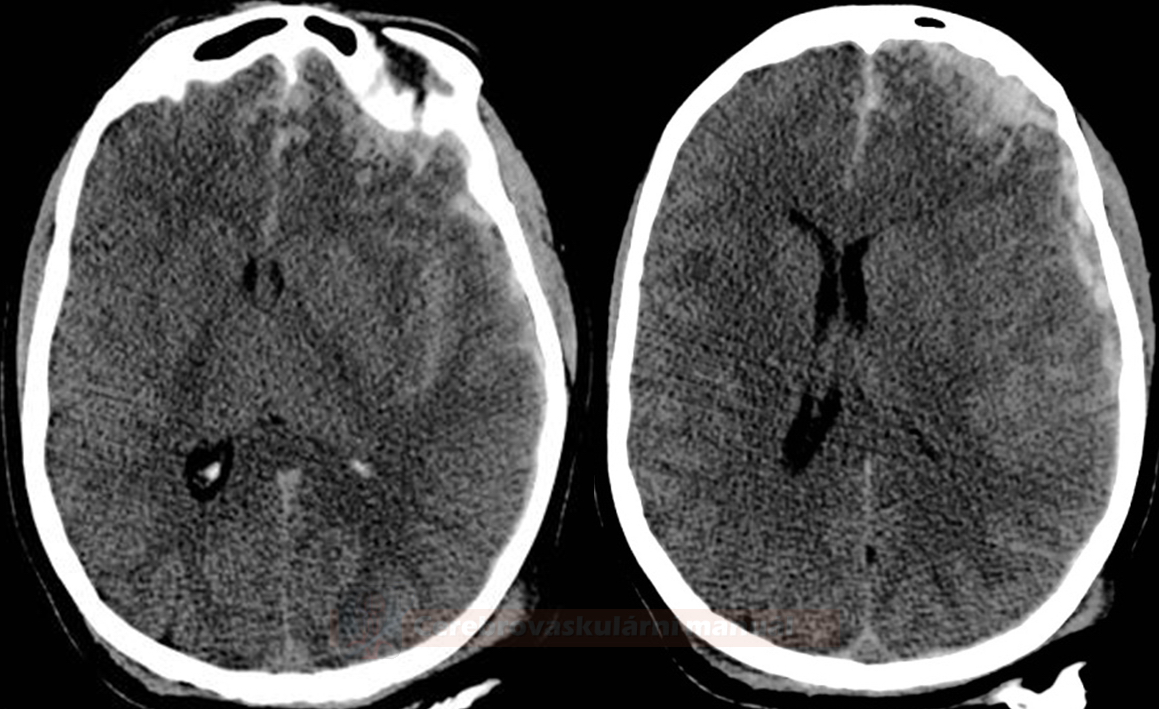
- subarachnoid hemorrhage (SAH) is a clinical syndrome caused by bleeding into the subarachnoid space (located between the arachnoid membrane and the pia mater surrounding the brain)
- traumatic SAH occurs due to traumatic brain injury (TBI)
- non-traumatic SAH often results from the rupture of a cerebral aneurysm (~75-80% of cases) or, less frequently, from arteriovenous malformation (AVM)
- aneurysms are acquired lesions related to hemodynamic stress on the arterial walls at bifurcations and bends
- aneurysmal SAH accounts for 3-8% of all strokes; aneurysms measuring 5-15 mm are most likely to rupture
- unruptured aneurysms are found in 0.3-5% of the population, with 15-20% of these individuals having multiple aneurysms
- about 20% of patients with one aneurysm will have an additional aneurysm
- the annual incidence of aneurysmal SAH varies by race, sex, and age
- reported rates ~ 10-26 cases per 100,000 population
- the incidence of SAH is higher in women than in men (ratio 3:2)
- incidence increases with age
- peaking at 40-65 years (80% of SAH cases)
- only 15% occuring in individuals aged 20-40 years and 5% in those < 20 years
- SAH is rare in children
- SAH may have an unfavorable prognosis (percentages vary in the literature):
- 5-15% of patients die before reaching hospital
- 30% present with severe initial deficits (Hunt-Hess 4-5)
- about 2/3 have mild deficit initially; 50% deteriorate soon due to spasms, rebleeding, surgery, and other complications
- 10-20% of hospitalized patients die within 24 hours due to rebleeding
- 5-15% of patients die before reaching hospital
- risk factors
- smoking, oral hormonal contraceptives, alcohol, hypertension, stimulants
- genetic predisposition – the risk increases with the number of family members involved or with a family history of adult polycystic kidney disease
Etiology
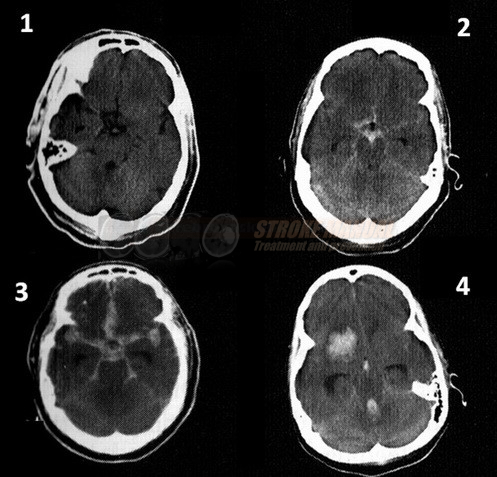
- there are three distinct SAH patterns, each with specific etiologies, treatments, and prognostic implications:
- suprasellar cisterns with peripheral extension
- perimesencephalic SAH (pmSAH)
- convexal SAH (cSAH)
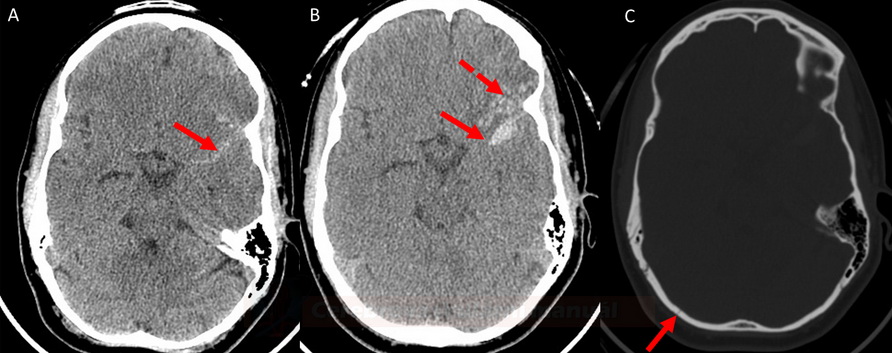
Traumatic SAH
- history of trauma (fall, car accident, etc.)
- commonly localized at the convexity between the gyri
- exclude usual concomitant traumatic changes (e.g., contusions, subdural/epidrual hematoma, skull bone fissure, subcutaneous hematoma)
- ! contusions may not be apparent for several hours ⇒ perform a control CT scan after a sufficient delay
- ! contusions may not be apparent for several hours ⇒ perform a control CT scan after a sufficient delay
Spontaneous (non-traumatic) SAH
|
60–80%
|
|
10–20%
|
|
|
Arteriovenous malformations → see here
|
5–10%
|
|
Other causes of SAH (mainly DDx of non-traumatic cortical SAH)
|
~ 5%
|
|
| Content available only for logged-in subscribers (registration will be available soon) |
Prognosis
- prognosis depends on the severity of the initial insult and our ability to prevent complications, specifically rebleeding (by early detection and treatment of the source)
- overall mortality up to 50%
- 10-15% of patients die before reaching the hospital
- another 10-15% die within the first 24 hours
- the most common causes of death are rebleeding or brainstem dysfunction due to a massive intraventricular hemorrhage or decompensated intracranial hypertension
- 10-15% of patients die before reaching the hospital
- 1/3 of survivors have significant functional deficits (motor and/or cognitive)
- cognitive deficits are present in numerous patients considered to have a good outcome
- SAH patients commonly experience deficits in memory, executive function, and language; these symptoms are accompanied by depression, anxiety, fatigue, and sleep disturbances
- 1/3 return to their normal function
| Factors influencing morbidity and mortality in SAH |
|
FAQs
- SAH is a type of stroke characterized by bleeding into the subarachnoid space (the area between the brain and the tissues covering it)
- this condition is often accompanied by a sudden, severe headache and can be life-threatening
- the most common causes of SAH are traumatic brain injury and a ruptured cerebral aneurysm (~ 75-80%)
- other causes include arteriovenous malformations (AVMs) and blood disorders; in some cases, the cause remains undetected
- a cerebral aneurysm is a weak spot in a brain artery that bulges and fills with blood
- when an aneurysm ruptures, it causes bleeding into the subarachnoid space, leading to SAH
- yes, genetic factors may play a role, especially in familial cases of brain aneurysms
- conditions such as polycystic kidney disease and certain connective tissue disorders are also associated with a higher risk of aneurysm and SAH
- yes, head injuries can cause SAH
- traumatic SAH usually occurs at the site of impact or where the brain moves against the skull during the injury and is typically associated with contusion, subdural or epidural hematoma
- yes, the use of certain drugs, particularly stimulants like cocaine and methamphetamine, can increase the risk of SAH due to their effects on blood pressure and arterial integrity
- smoking is a major risk factor for the formation and rupture of cerebral aneurysms, thereby significantly increasing the risk of SAH
- the risk is dose-dependent and decreases after smoking cessation
- the prognosis of SAH depends on the cause, severity, and presence of complications
- in severe cases, 50% die before reaching the hospital
- of those who make it to the hospital:
- 1/3 die in the hospital
- 1/3 survive with a disability
- 1/3 return to normal function