ISCHEMIC STROKE / CLASSIFICATION AND ETIOLOGY
CARASIL
(Cerebral Autosomal Recessive Arteriopathy with Subcortical Infarcts and Leukoencephalopathy)
Updated on 18/06/2024, published on 12/05/2023
Definition
- CARASIL is a very rare (probably underdiagnosed) hereditary disease affecting the small cerebral vessels, spine, and hair follicles
- caused by a mutation in the HTRA1 gene on chromosome 10q (10q25.3-q26.2)
- high-temperature requirement protein A1, a highly conserved serine protease (Clausen, 2002)
- there are 2 forms (Onodera, 2010)
- classic CARASIL – associated with biallelic pathogenic variants (AR inheritance)
- HTRA1-CSVD – associated with heterozygous HTRA1 pathogenic variant (AD inheritance)
- classic CARASIL is characterized by early-onset white matter changes and associated neurologic symptoms (early-onset gait disturbance, cognitive impairment) and scalp alopecia
- HTRA1-CSVD may be oligosymptomatic or asymptomatic (with positive neuroimaging only)
Clinical presentation
CLASSIC CARASIL
- premature alopecia (starting in the teenage years; one of the initial symptoms)
- musculoskeletal symptoms (before the age of 30)
- deforming spondylosis (cervical spine and/or thoracolumbar spine), disc herniation
- knee or elbow osteoarthritis
- deforming spondylosis (cervical spine and/or thoracolumbar spine), disc herniation
- spastic gait (between 20 and 40 years of age)
- recurrent ischemic stroke-like episodes (typically before age 40) with gradually progressive vascular dementia and mood changes (apathy)
- symptomatic poststroke epilepsy
- unlike CADASIL, migraine is not a feature of classic CARASIL
HTRA1-CSVD
- slowly progressive gait disturbance and stroke-like episodes (typically occur after the age of 40)
- may be followed by mood changes and cognitive dysfunction
- spondylosis and alopecia are less common
Diagnostic evaluation
CARASIL should be suspected if the combination of diffuse vascular leukoencephalopathy, alopecia, and disk herniations occurs at a young age
Neuroimaging
- CT shows nonspecific hypodensities in the white matter (leukoaraiosis)
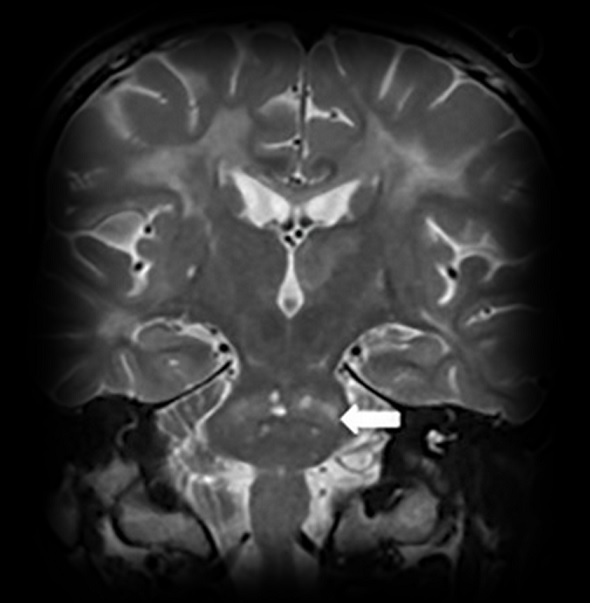
- MRI detects hypointensities on T1 and hyperintensities on T2
- white matter lesions (WML)
- U-fibers are relatively preserved
- it is not clear whether the anterior temporal pole and external capsule lesions are observed in the early stages of CARASIL
- lacunar infarcts in the basal ganglia, thalamus, and pons
- arc sign – increased T2 signal across the pons at the level of middle cerebellar peduncles (Röben, 2016)
- cerebral microbleeds (CMBs) → see here
- white matter lesions (WML)
Laboratory tests
- genetic testing – considered the gold standard for a definitive diagnosis
- mutation affects the HTRA1 gene located on chromosome 10q (10q25.3-q26.2
- once HTRA1 pathogenic variant(s) have been identified in family members, prenatal and preimplantation testing is possible
- a skin biopsy is not useful for establishing a diagnosis
Differential diagnosis
- Binswanger´s disease
- occurs in elderly individuals with multiple vascular risk factors
- absence of typical temporal lobe lesions
- CADASIL
- symptoms appear 10-15 years earlier in patients with classic CARASIL
- migraine and depression are not present in CARASIL
- Susac syndrome
- no temporal lobe involvement
- prominent retinopathy and hearing impairment
- MELAS
- primary angiitis of the CNS (PACNS)
- an inflammatory disorder affecting the cerebral blood vessels
- progressive multiple sclerosis
- COL4A1 cerebral small-vessel disease
- COL4A1 refers to a gene that encodes one of the collagen proteins, specifically collagen type IV alpha 1
- mutations in the COL4A1 gene have been associated with various medical conditions, particularly those related to abnormalities in the blood vessels, kidneys, and the nervous system
- the effects of COL4A1 mutations can vary widely among individuals, and the severity of symptoms can differ
- CARASAL (cathepsin A-related arteriopathy with strokes and leukoencephalopathy) – an extremely rare condition
- mutations in the CTSA gene, which encodes the enzyme cathepsin A; these mutations lead to abnormal blood vessel development and function in the brain
- individuals with CARASAL typically experience recurrent strokes or stroke-like episodes + leukoencephalopathy on MRI
- CARASAL usually becomes apparent in adulthood, typically during the third to fifth decades of life
- RVCL-S
Management
- no causal or disease-modifying treatment is available for CARASIL
- therapy is similar to that of traditional small-vessel diseases
- management of modifiable vascular risk factors
- antiplatelets in secondary stroke prevention
- no data on primary prevention
- no data on primary prevention
- risk/benefit ratio of tPA and anticoagulation is uncertain
- symptomatic treatment of psychiatric disorders and spasticity
- there is no specific treatment, but memantine or donepezil may be helpful
- physical therapy, walking aids, cognitive training
- standard treatment of spondylosis and mood disorders
- genetic counseling is recommended for individuals and families affected by CARASIL to provide guidance and support regarding the genetic aspects of the disease