NEUROIMAGING / DSA
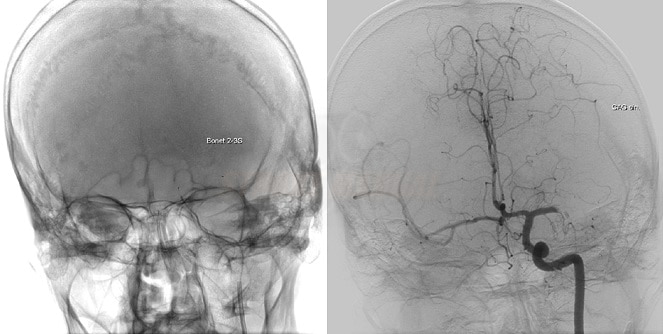
Digital subtraction angiography (DSA)
Updated on 13/12/2023, published on 03/05/2021
- Digital Subtraction Angiography (DSA) is a fluoroscopic technique used to visualize the vascular system. Structures such as bone are digitally subtracted from the image, allowing for better visualization of blood vessels
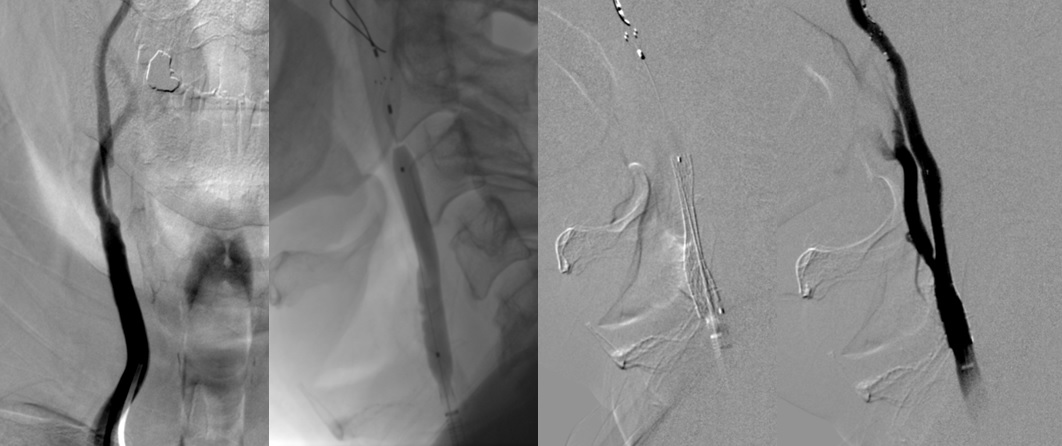
- the Seldinger method is used to access the vessels
- the vessel is punctured with a hollow needle
- a curved, soft-tip guidewire is inserted through the needle and positioned in the vessel lumen
- a guidewire is held while the needle is carefully removed
- the large catheter is threaded into the vessel lumen over the guidewire
- the guidewire is subsequently removed
- sheath now serves as a route for diagnostic catheters and other medical devices
Indications
Acute and elective therapeutic endovascular procedures
- acute ischemic stroke endovascular treatment (EVT)
- local intra-sinus thrombolysis in patients with cerebral sinus thrombosis → more
- angioplasty and stenting of extra- or intracranial stenoses → carotid angioplasty with stenting
- endovascular treatment of malformations (AVM, DAVF) and aneurysms
Diagnosis of cerebral vascular diseases
| Content available only for logged-in subscribers (registration will be available soon) |
Functional tests
- balloon test occlusion (BTO) – assesses whether an artery can be temporarily/permanently intentionally occluded without significantly affecting brain perfusion
- Wada test – short-term blockade of the function of a specific part of the brain after the selective intra-arterial administration of a short-acting barbiturate. It helps to determine which hemisphere controls language function and how important each hemisphere is for memory function
Detection of circulatory arrest in brain death diagnosis
Contraindications
Most contraindications are relative ⇒ assess risk-benefit
- contrast-related contraindications
- renal insufficiency (laboratory tests results must be obtained before the examination)
- estimated Glomerular Filtration Rate (eGFR) should be > 30 mL/min in patients receiving iodinated contrast agent
- use with caution in patients with eGFR < 45 mL/min
- estimated Glomerular Filtration Rate (eGFR) should be > 30 mL/min in patients receiving iodinated contrast agent
- hypersensitivity to iodinated contrast media (contrast agents)
- reaction to contrast media is not a true allergy but a pseudoallergy in nature (no allergic antibodies are present)
- the contrast media cause mast cells to release histamine and other chemicals directly
- the concentration of the contrast media affects the severity of an adverse reaction (higher concentration = higher risk of an adverse reaction)
- the risk of serious, life-threatening reactions, including anaphylaxis, is ~ 0.1%
- renal insufficiency (laboratory tests results must be obtained before the examination)
- pregnancy (relative contraindication for acute therapeutic procedures)
- blood clotting disorders and use of anticoagulants (relative)
- unstable cardiopulmonary/neurological status
Procedure
Preprocedural evaluation
- check:
- personal medical history (presence of atherosclerotic disease, diabetes, renal dysfunction, etc.)
- adverse reactions and previous exposure to iodinated contrast media
- prior vascular procedures
- review relevant vascular imaging studies (CTA, MRA, neurosonology)
- the patient should be fasting (for > 4h, except for acute interventions)
- ensure adequate hydration for nephropathy prevention
- for diabetic patients, avoid oral antidiabetic agents (e.g., metformin) in the morning before the procedure
- insert an intravenous cannula and urinary catheter
- obtain the patient’s informed consent for the procedure, ensure they are fully informed about the procedure and its risks
Principles of contrast media administration and allergy premedication
Monitoring during examination
- the angio suite should be equipped with a monitor and a crash cart
- standard monitoring during diagnostic DSA
- heart rate
- blood oxygenation (pulse oximetry)
- blood pressure (intermittently via a self-inflating cuff)
- an anesthesiologist should be available if sedation or general anesthesia (GA) is required
Procedural technique
| Content available only for logged-in subscribers (registration will be available soon) |
Postprocedural care
- bed rest for at least 4-6 hours
- careful compression and monitoring of the puncture site and peripheral blood supply
- blood pressure monitoring
- adequate hydration
Complications
- the risk of permanent neurological deficit associated with diagnostic DSA is low (0.09-0.14%)
- increased risk is associated with endovascular procedures (thrombectomy, coiling, stenting, etc.)
→ local and systemic complications of endovascular procedures