ISCHEMIC STROKE / PREVENTION
Vertebrobasilar steno-occlusive disease
Updated on 26/01/2024, published on 06/02/2023
- the vertebrobasilar (VB) system (also called posterior circulation) comprises the subclavian, vertebral, and basilar arteries and their branches; it supplies the cervical spinal cord, brainstem, cerebellum, thalamus, and occipital lobes → anatomy of cerebral arteries
- posterior circulation is frequently affected by atherosclerosis (AS), although less frequently than the anterior circulation
- incidence ~ 20-40% of all patients with a cerebrovascular disease
- atherosclerosis predominantly affects the origin of the vertebral arteries and the V4 segment
- incidence ~ 20-40% of all patients with a cerebrovascular disease
- in addition to atherosclerosis, other conditions may affect perfusion:
- hypoplasia or aplasia (may become relevant if another pathology occurs)
- variations in the arterial course (kinking, coiling) or origin
- mechanical compression in the vertebral foramen (Bow hunter’s syndrome)
- subclavian (vertebral) steal syndrome
- dissection (typically in the V3 segment)
- hypoplasia or aplasia (may become relevant if another pathology occurs)
- the most common mechanisms of posterior circulation stroke/TIA include:
- thromboembolism (resulting from plaque, dissection, or cardioembolism)
- hypoperfusion (caused by severe stenosis of various etiologies)
- vasospasm (less common)
- thromboembolism (resulting from plaque, dissection, or cardioembolism)
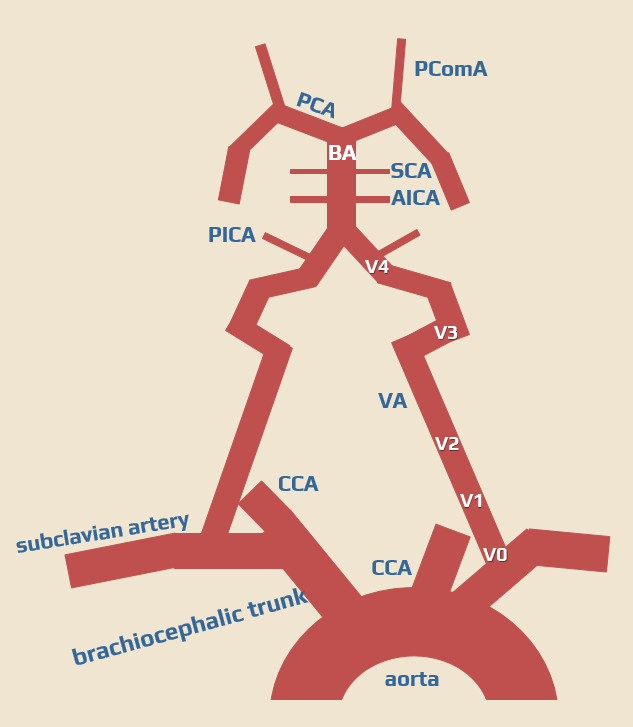
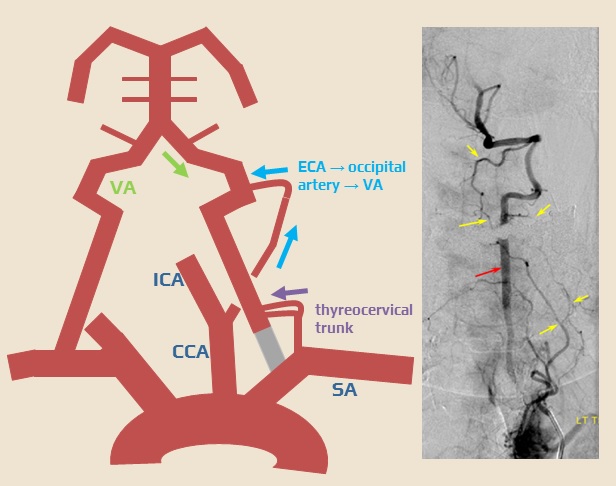
Collateral circulation
- compensatory collateral circulation may occur in the case of proximal stenosis or occlusion of the subclavian and vertebral arteries
- retrograde flow in the vertebral artery (from the contralateral VA, with or without steal phenomenon in the basilar artery)
- collaterals from the occipital artery and the thyrocervical trunk
- steal from a vertebral or mammary artery (with subclavian stenosis/occlusion)
- collateral retrograde flow from PCA (via PComA) to the basilar artery in case of its proximal occlusion
Clinical presentation
- asymptomatic stenosis (very common)
- with/without steal phenomenon (asymptomatic flow alteration in a vertebral artery) on ultrasound
- weakened pulse and lower blood pressure in the affected limb may be present with significant subclavian artery stenosis
- transient symptoms of hypoperfusion
- posterior circulation stroke
- variable combination of symptoms from the brainstem, thalamus, cerebellum, and occipital and temporal lobes
- caused by hypoperfusion or thromboembolism
- transient symptoms (TIA) may precede the infarction
Diagnostic evaluation
Neurosonology
- a first-line method in the nonacute setting
- accurate, noninvasive, safe, widely available, and inexpensive
- useful in combination with CTA/MRA when any invasive procedure is planned
- assess:
- B-mode
- size of the artery (hypoplasia?)
- search for plaque (composition, stenosis), dissection, thrombus
- color Doppler
- flow direction
- turbulences (aliasing)
- spectral Doppler
- waveform
- velocities
- B-mode
| Content available only for logged-in subscribers (registration will be available soon) |
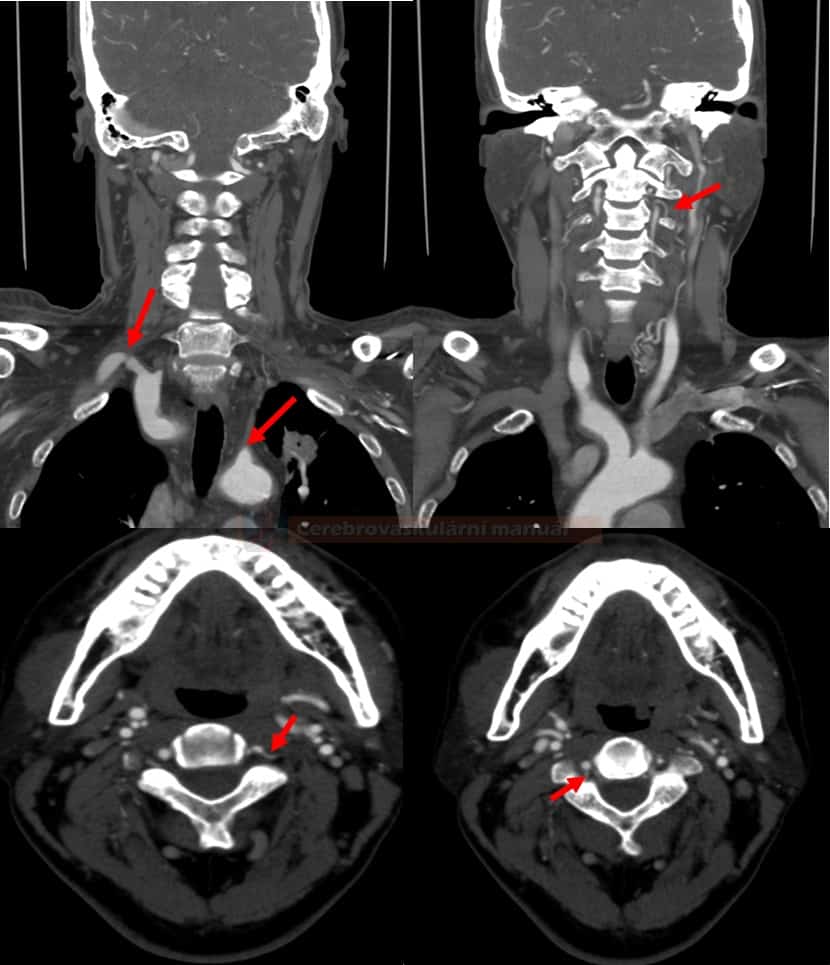
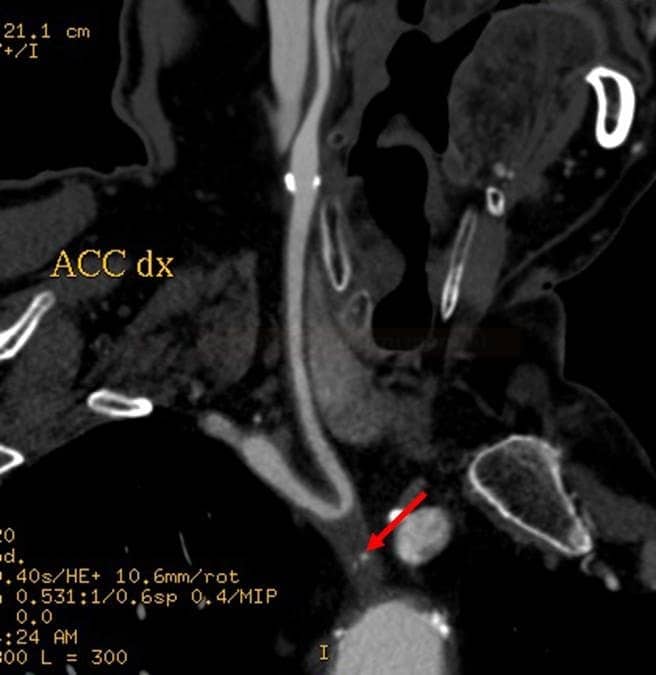
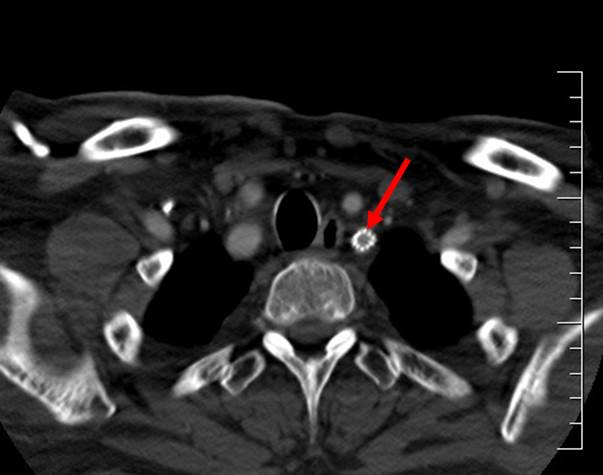
CT/MR angiography
- assess all segments of the posterior circulation, starting from the aortic arch
- CT angiography is preferred, as it provides better visualization of the aortic arch and the origin of the vertebral arteries
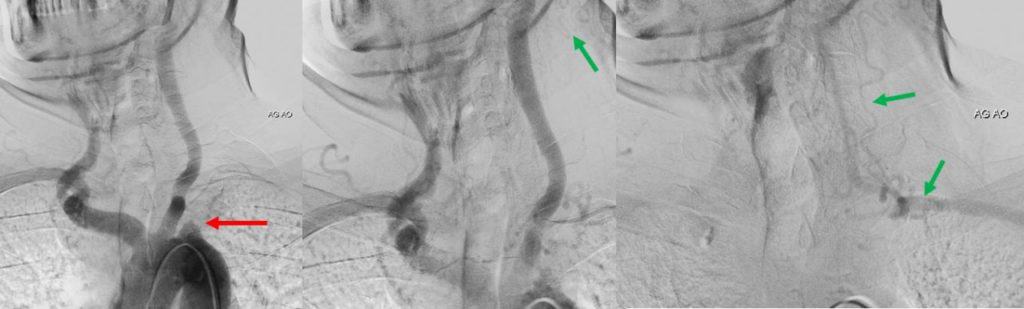
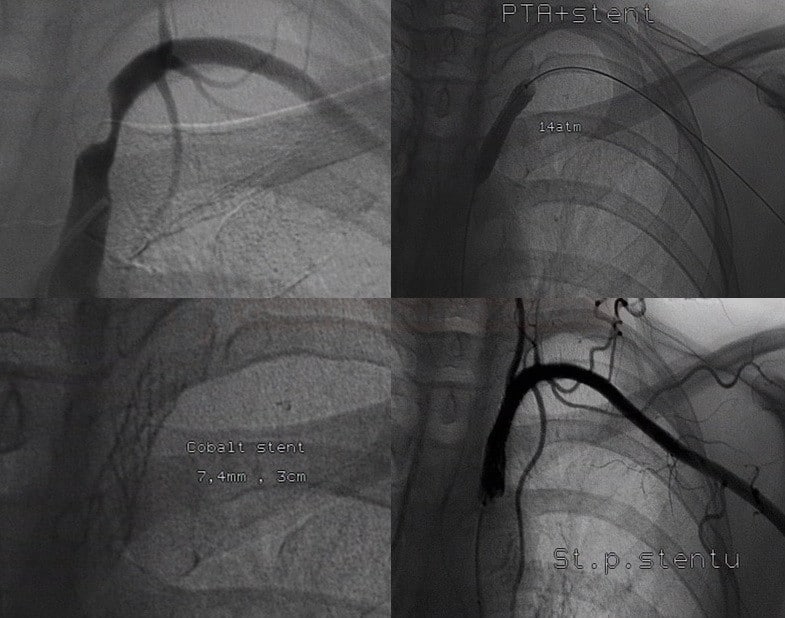
Digital subtraction angiography (DSA)
- diagnostic DSA has been almost completely replaced by noninvasive imaging techniques
- DSA has a critical role in interventional neuroradiology; it is frequently used for therapeutic interventions like coiling of aneurysms, arteriovenous malformation (AVM) embolization, thrombectomy, and stenting
Management
Acute posterior circulation stroke
- recanalization therapy for all eligible patients → posterior circulation stroke
Stroke prevention
- patients with symptomatic vertebral stenosis have a higher risk of recurrence than those with carotid stenosis [Flossmann, 2003]
- prospective studies found a 90-day risk of stroke after vertebrobasilar stroke/TIA of 9.6% in those with vertebrobasilar stenosis and 2.8% in those without, with the highest risk (13.9%) if the stenosis is intracranial (Gulli, 2009)
- aggressive medical therapy (BMT) is crucial
- there are no standardized indication criteria for interventions