ADD-ONS / SCALES
TOAST classification of stroke
Updated on 22/07/2024, published on 28/12/2022
- the exact etiology of ischemic stroke has implications for both prognosis and management
- a classification system for ischemic stroke subtype, mainly based on etiology, was developed for the Trial of Org 10172 in Acute Stroke Treatment (TOAST)
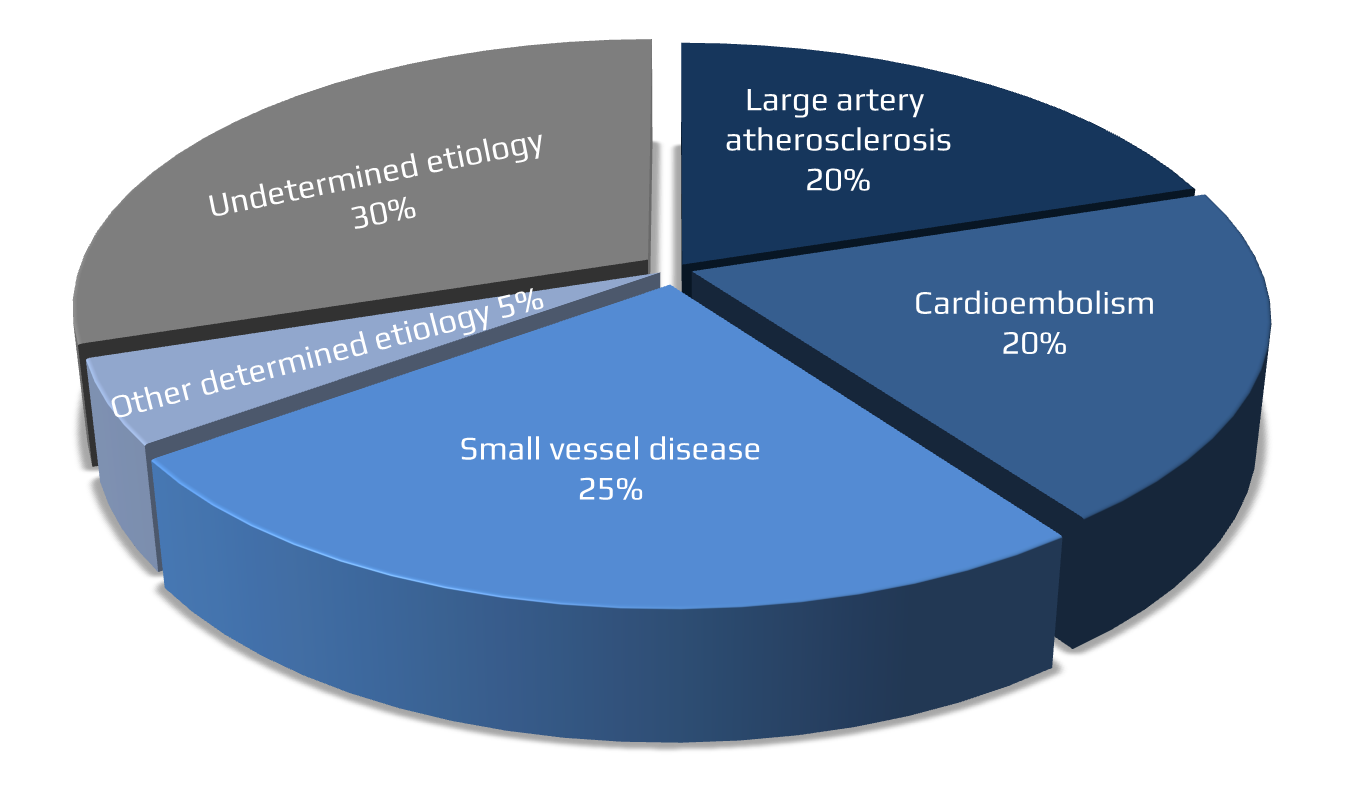
- the TOAST classification identifies five ischemic stroke subtypes:
- 1 – large-artery atherosclerosis (LAA)
- 2 – cardioembolic stroke (CE)
- 3 – small-vessel disease (SVD) / penetrating artery disease (PAD)
- 4 – stroke of other determined cause
- 5 – stroke of undetermined cause (cryptogenic stroke)
- 1 – large-artery atherosclerosis (LAA)
- diagnosis is based on clinical features and data from brain imaging (CT/MRI), vascular imaging (CTA/MRA, neurosonology, DSA), cardiac imaging, and laboratory tests
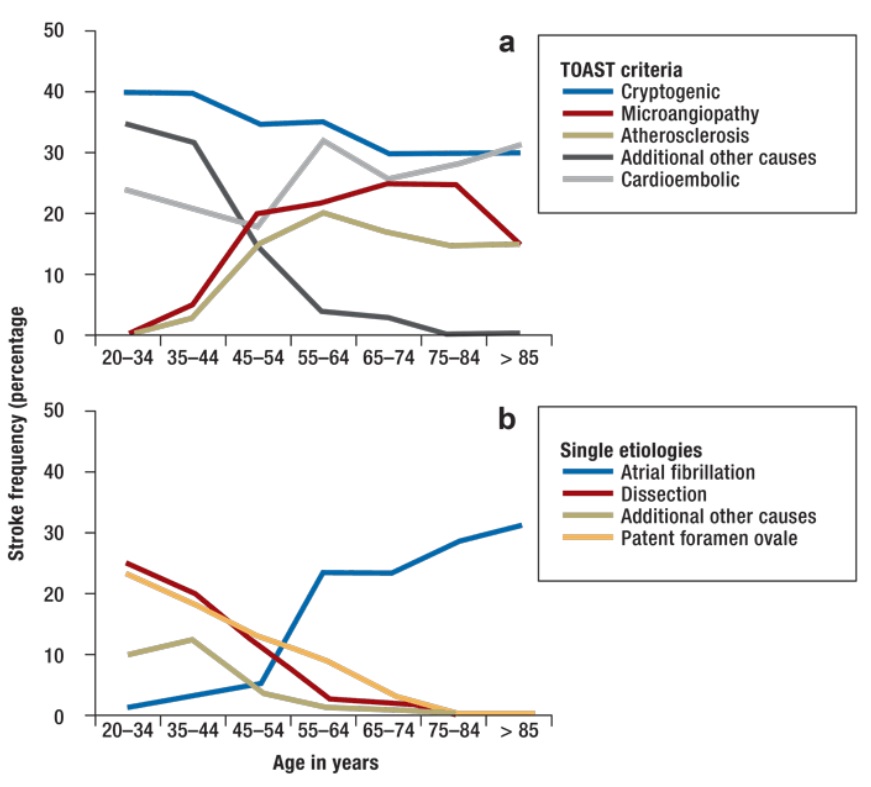
- the prevalence of each group varies depending on the mean age of the patient cohort
- cryptogenic stroke and TOAST 4 are predominant in younger age groups
- arteriolopathy and cardioembolic stroke are more prevalent in older age groups (reflecting the increased incidence of atrial fibrillation and other cardiac diseases.)
- cryptogenic stroke and TOAST 4 are predominant in younger age groups
- one large-scale application of the TOAST classification is the Get with the Guidelines-Stroke (GWTG-Stroke) registry; however, the TOAST subtypes entered into the registry were accurate in only 61% of patients (Rathburn, 2024)
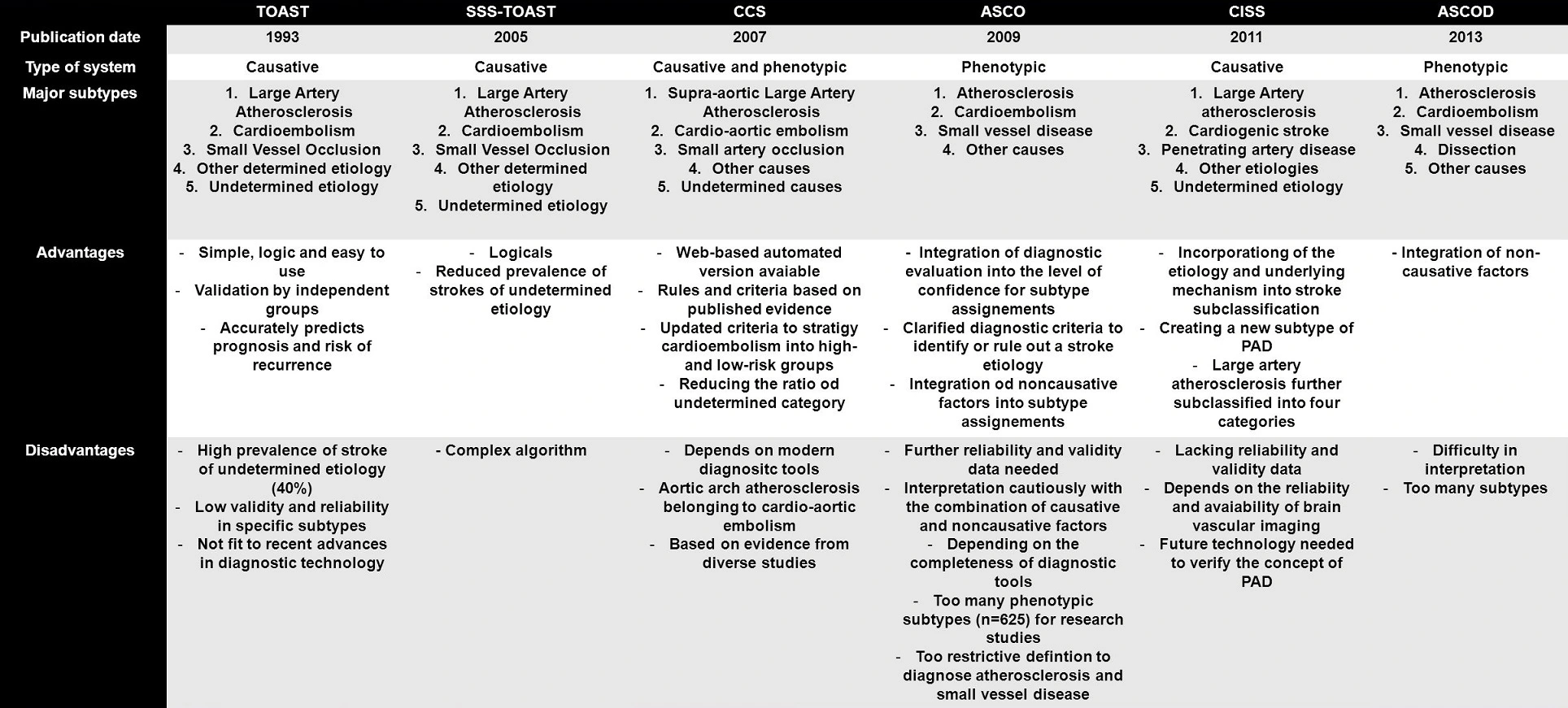
- several other improved classification systems have been introduced:
- SSS-TOAST (2005)
- CISS (2011)
- CCS (2007), ASCO (2009), ASCOD (2013)
TOAST 1 – Large Artery Atherosclerosis (macroangiopathy)
- medium and large arteries are affected
- stroke is caused by atherothrombosis or thromboembolism
- significant stenosis (> 50%) or occlusion of a relevant extra- or intracranial artery due to atherosclerosis
→ Assessment of atherosclerotic plaques
- cortical lesion on brain CT/MRI
- subcortical lesion > 1.5 cm on brain CT/MRI (originally published)
- it is known that even smaller lesions can be caused by branch artery atherosclerosis (see CISS Classification)
- it is known that even smaller lesions can be caused by branch artery atherosclerosis (see CISS Classification)
- stroke mechanisms in TOAST 1:
-
- progressive narrowing to complete arterial occlusion (symptoms vary depending on the quality of the collateral circulation)
- artery to artery embolism
- combination of both mechanisms (embolism occurring at the time of ICA occlusion)
Issues discussed regarding TOAST 1
- a specific and probably underdiagnosed cause of thromboembolism originates from unstable (complicated) non-stenosing (< 50%) plaques in CCA, ICA, aorta, and intracranial arteries [Harloff, 2010]
- additionally, small infarcts resulting from atherosclerotic plaques in the ostium of perforating arteries should be included here ⇒ branch artery disease (BAD) / branch occlusive disease (BOD)
- significance of plaque composition and morphology is increasingly acknowledged
- evidence of intraplaque hemorrhage (IPH), thrombus, thin or ruptured fibrous cap, or a large lipid-rich and/or necrotic core (visible on high-resolution MRI) correlates with an increased risk of cerebrovascular events, irrespective of stenosis severity [Kopczak, 2020] [Kamel, 2019
- these findings may support the classification of atherothrombotic etiology (TOAST 1)
- no significant atherosclerosis in major cerebral arteries
- presence of a potential cardioembolic source (especially any high-risk factor)
TOAST 2 – Cardioembolic stroke
- at least one significant potential cardioembolic source must be identified
- cardiac sources are categorized into high-risk and intermediate-risk groups based on their likelihood of causing embolization
- high-risk sources:
- clinical and neuroimaging findings are similar to those of TOAST 1
- a stroke in a patient with a medium-risk source of embolism and no other identifiable cause of stroke is classified as a possible cardioembolic stroke
- presence of significant stenosis in relevant extra- and/or intracranial arteries
TOAST 3 – Small artery disease (arteriolopathy, microangiopathy)
- lacunar strokes
- leukoaraiosis
- clinical presentation: lacunar stroke / subcortical ischemic encephalopathy
- + presence of traditional vascular risk factors (hypertension, dyslipidemia, diabetes, etc.)
- brainstem or subcortical lesion on CT/MRI (diameter < 1.5 cm)
- leukoencephalopathy on CT/MRI
(→ FAZEKAS scale, ARWMC scale)
- caused by lipohyalinosis (the main feature of lipohyalinosis is the thickening of the vessel wall with narrowing of the lumina; eventually, vessel occlusion and infarction may occur)
- distinguish non-arteriolopathic occlusion of perforating arteries
- atherosclerosis of the parent artery near the perforator origin – Branch Artery Disease (BAD) / Branch Occlusive Disease (BOD)
- infarcts tend to be larger compared to classic arteriolopathy
- high-resolution MRI can be used for diagnosis
- embolization (from proximal arterial segments or from the heart)
- atherosclerosis of the parent artery near the perforator origin – Branch Artery Disease (BAD) / Branch Occlusive Disease (BOD)
- genetic small vessel diseases should be classified as TOAST 4
- presence of significant stenosis in relevant extra- and/or intracranial arteries
- presence of a significant cardioembolic source
- hemispheric infarct on CT/MRI
TOAST 4 – Stroke of other determined etiology
- < 5% of stroke patients < 50 years of age
- mainly PACNS and Takayasu arteritis occur at a younger age
- giant cell (temporal) arteritis occurs in elderly patients (> 50 years of age)
- arterial dissection
- vasospasm
- primary (idiopathic)
- secondary (due to complicated migraine, SAH-related vasospasm, VSP provoked during angiography or by drugs, etc.)
- reversible vasoconstriction syndrome (RCVS)
- moya-moya angiopathy
- multiple etiologies (e.g., idiopathic, Grange syndrome, ACTA2 mutations, vasculitis, etc.)
- metabolic diseases
- Fabry disease
- homocystinuria
- MELAS
- migraine (probably due to prolonged vasospasm)
-
heritable connective tissue disorders (HCTDs)
- Sneddon syndrome
- non-inflammatory thrombotic angiopathy affecting small to medium-sized arteries; presenting as stroke + livedo racemosa
- carotid artery web
- Grange syndrome
- dolichoectasia (usually involving the basilar artery)
- bone disorders and stroke (bony stroke)
- rare bone or cartilage anomalies affecting arteries supplying the brain
- may be considered in patients with recurrent ischemic stroke of unknown cause in the same vascular territory
- in addition to conventional vascular imaging, the dynamic imaging modalities with the patient’s head rotated or reclined may confirm the diagnosis (e.g., Bow hunter´s syndrome)
- Eagle’s syndrome is a condition associated with the elongation of the styloid process or calcification of the stylohyoid ligament, clinically characterized by throat and neck pain radiating into the ear; rarely, it may cause carotid dissection
(Ogura, 2015) (Saccomanno, 2018)
- rare bone or cartilage anomalies affecting arteries supplying the brain
- Susac syndrome (retino-cochleo-cerebral vasculopathy)
- COVID-19
- often in younger patients, in up to 1/3 of cases asymptomatic) [Shahjouei, 2021] [Fridman, 2020]
- 36% in age <55 yrs, 46% < 65 y [Shahjouei, 2021]
- predominantly embolic mechanism with large artery occlusion (LVO) due to a hypercoagulable state [Shahjouei, 2021] [Yaghi, 2020]
- more severe course compared to non-COVID patients
- ↑ D-dimers
- often in younger patients, in up to 1/3 of cases asymptomatic) [Shahjouei, 2021] [Fridman, 2020]
- hypercoagulable states
- primary – most often antiphospholipid syndrome and APC resistance
- secondary
- oncohematologic diseases (e.g., leukemia, polycythemia vera)
- thrombotic thrombocytopenic purpura (TTP)
- non-specific intestinal inflammation
- nephrotic syndrome
- hemoglobinopathies (typically sickle cell disease)
- hematological malignancies
- hyperviscosity syndrome (HVS)
- intracardiac shunt (PFO, ASD, etc.) – usually classified as TOAST 2
- extracardiac shunt
- pulmonary AV malformations (PAVM)
- patent ductus arteriosus (PDA) (Panagopoulos, 2019)
- persistent left superior vena cava (PLSVC) (Hutyra, 2010) (Azizova, 2020)
- angiography (including cardiac catheterization) → complications of endovascular procedures
- carotid revascularization (CEA, CAS)
- Extra Corporeal Circulation (ECC) related complications
- air and fat embolism (see below)
- fat embolism
- typically occurs after trauma (long bone fractures) and surgery (including plastic surgery with fat removal)
- air embolism (microscopic x macroscopic)
- a consequence of the incorrect insertion of a venous catheter into an artery [Riebau, 2004]
- improper extraction of the central venous catheter (CVC) [Brockmeyer, 2009]
- repeated IV applications in combination with pulmonary AV shunt or PFO
- during catheterization
- embolization of cholesterol particles from plaques should be assessed as TOAST 1 → Cholesterol Embolization Syndrome (CES)
- spontaneous x iatrogenic
- various mechanisms ( e.g., vasospasm, cardioembolism in endocarditis)
-
oral contraceptives (usually in combination with a hypercoagulable state and/or smoking)
-
cocaine, crack, amphetamines, LSD, and heroin (drugs often cause IC bleeding)
-
sympathomimetics, ergotamine, sumatriptan
- various mechanisms (most usually due to a hypercoagulable state or cardioembolism)
- specific causes of stroke in pregnancy:
- preeclampsia/eclampsia
- amniotic fluid embolization (AFE)
- choriocarcinoma
- postpartum cerebral angiopathy
- postpartum/peripartum cardiomyopathy (PPCM)
TOAST 5 – Stroke of undetermined etiology
- the cause of the stroke could not be determined with sufficient certainty
- ≥2 potential causes of stroke were identified (such as atrial fibrillation in a patient with > 50% carotid stenosis or significant carotid stenosis combined with microangiopathy)
- cryptogenic stroke (CS) – no identifiable etiology despite extensive evaluation
- incomplete diagnostic evaluation