GENERAL NEUROLOGY
Pupillary response in consciousness disorders
Updated on 14/03/2024, published on 22/11/2023
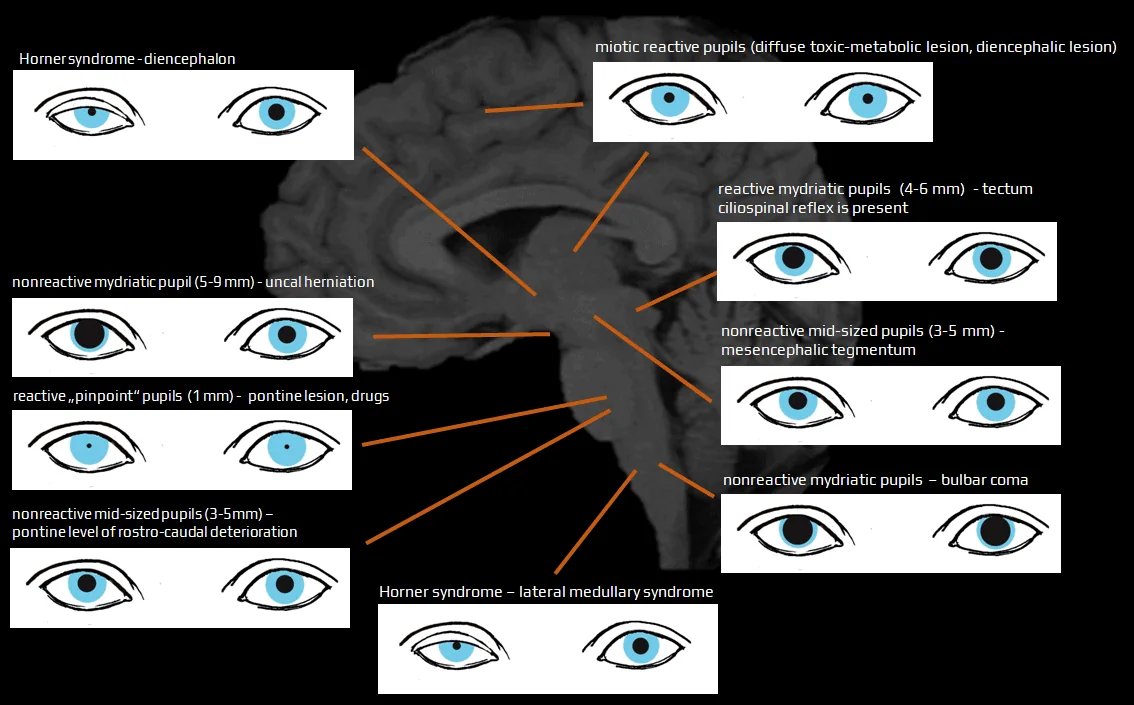
The primary goals of the neuro-ophthalmic exam are to determine the etiology, location, and severity of the consciousness disorder
Normal pupils
- normal pupils are round and regular, equal in size (isocoric) under both light and dark illumination
- in adults, the typical pupil size ranges from 2 to 4 mm in diameter in bright light and 4 to 8 mm in the dark
- normal direct and consensual response to light stimulus
- pupils constrict to direct illumination (direct response) and the illumination of the fellow eye (consensual response)
- in darkness, the pupils dilate
- an intact near response (accommodation reflex)
- the test requires voluntary effort
- both pupils constrict when the eyes focus on a near object, accompanied by accommodation (lens thickening and eye convergence
- absence of a RAPD
Pupillary light reflex
- the pupillary light reflex (PLR) is easily tested in unconscious patients:
- first, observe the pupil size in ambient and dim lighting to check for anisocoria
- shine a bright light into one eye and then alternate between each eye, observing the reactivity of both pupils
- note if the pupils react briskly, sluggishly, or show no response
- a relative afferent pupillary defect (RAPD) can be detected by swinging the flashlight from one eye to the other
Abnormal pupils
- abnormal pupil shape
- inadequate miosis or mydriasis
- bilateral, small but reactive pupils are nonspecific
- may suggest a metabolic etiology, diencephalic lesion, or the effect of certain toxins/drugs
- bilateral nonreactive mydriasis can indicate midbrain lesions or bulbar coma
- bilateral, small but reactive pupils are nonspecific
- anisocoria
- unilateral mydriasis
- uncal herniation – compression of the N III e at the Kernohan notch with the ipsilateral (rarely contralateral) nonreactive mydriasis (Hutchinson pupil) (Agrawal, 2020)
- any compressive lesion along the third nerve (e.g., ruptured posterior communicating artery aneurysm) may cause ophthalmoparesis with nonreactive mydriasis
- exclude pharmacologic dilation (administration of topical 1% pilocarpine will not constrict an atropinized, pharmacologically dilated pupil)
- unilateral, small but reactive pupil
- Horner syndrome is caused by damage to the ipsilateral oculosympathetic pathway
- the descending pathway from the hypothalamus to Budge´s ciliospinal center in the C8-T2 segments of the spinal cord
- ascending sympathetic chain that returns to the internal carotid artery, the cavernous sinus, cranial nerve VI, and then via CN V1 to the eye
- anisocoria worsening in the dark and mild ipsilateral ptosis (semiptosis) support the diagnosis of Horner syndrome (confirmation using cocaine drops is possible)
- Horner syndrome is caused by damage to the ipsilateral oculosympathetic pathway
- unilateral mydriasis
- abnormal reaction to light
- failure to dilate in the dark
- failure to constrict to light or accommodation
- dissociation between direct and consensual reactions
- relative afferent pupillary defect (RAPD)
- absent accommodation reaction
- light-near reflex dissociation
- an impaired pupillary light reaction while the near reaction remains intact
- unilateral or bilateral (dorsal midbrain lesion)
| diencephalon |
|
| mesencephalon (midbrain) |
|
| pons |
|
| medulla oblongata |
|