NEUROIMAGING / NEUROSONOLOGY
Transcranial ultrasound monitoring
Updated on 27/02/2024, published on 27/10/2023
- transcranial ultrasound (TCD/TCCD) is a non-invasive imaging technique helpful in evaluating flow in intracranial vessels
- prolonged continuous monitoring or repeated examinations can be useful in certain situations
Monitoring of intravenous thrombolysis
- continuous ultrasound monitoring during intravenous thrombolysis (sonothrombolysis) may accelerate thrombus dissolution; the method is currently not recommended beyond clinical trials
- intermittent diagnostic TCD/TCCD monitoring is acceptable to assess the effect of IVT
- The Thrombolysis In Brain Ischemia (TIBI) and the Consensus on Grading Intracranial Flow Obstruction (COGIF) scales were developed to standardize the assessment of intracranial occlusion via ultrasound
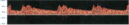
TIBI (Thrombolysis in Brain Ischemia)
- the TIBI classification was developed to grade residual flow
- it correlates with initial stroke severity, clinical recovery, and mortality in acute stroke patients
- no improvement in the residual flow correlates with the absence of early clinical recovery and increased mortality (Demchuk, 2012)
- no improvement in the residual flow correlates with the absence of early clinical recovery and increased mortality (Demchuk, 2012)
According to [Demchuk, 2001]
| Recanalization assessment [Clotbust, 2007] |
|
| Complete recanalization | TIBI 4-5 |
| Parcial recanalization | increase of TIBI by ≥1 grade (but not to 4 or 5) |
| Reocclusion | decrease of TIBI by ≤1 grade |
COGIF
Differentiation of TIBI grades 1-3 (minimal flow, blunted flow, dampened flow) may be difficult. The flow patterns of these grades not only reflect partial M1 recanalization but also the hemodynamic situation in other segments. The COGIF scoring system was designed to more clearly follow the recanalization process; it is exclusively based on known hemodynamic changes of the Doppler spectrum. The time course of grades during the serial examination must be encoded.
| Recanalization assessment | |
| Complete recanalization |
COGIF 4 |
| Partial recanalization |
improvement by ≥1 grade (but not to 4) |
| No change |
baseline COGIF grade persists |
| Worsening | decrease by ≥1 grade |
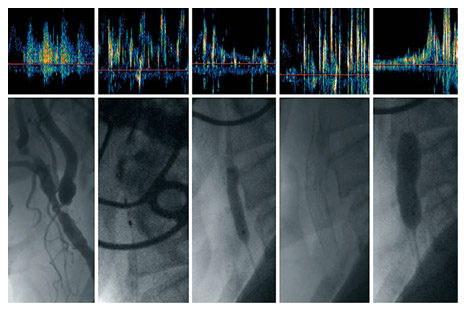
Monitoring of microembolizations
- transcranial ultrasound (TCD/TCCD) can detect high-intensity transient signals (HITS) in the cerebral circulation. These signals may represent artifacts or solid or gaseous emboli
- TCD device equipped with a headframe for transducer fixation and specific software is typically used for prolonged monitoring
Clinical application
- etiological diagnosis of stroke/TIA; microemboli detection supports suspicion of embolic etiology
- detection of unstable plaque (exulcerated with subsequent thrombus formation followed by arterio-arterial embolization)
- other sources of embolism (e.g., from the aortic arch)
- detection of cardioembolism (including paradoxical embolization via PFO or other AV shunts)
- detection of air embolism (after vein injury, iatrogenic)
- monitoring of microemboli in asymptomatic carotid stenosis (proof of high-risk plaque)
- assessment of the effect of antithrombotic therapy (reduction/elimination of HITS)
- monitoring during CAS, CEA, or cardiac surgery (see below)
Technical aspects of transcranial monitoring
- continuous TCD/TCCD monitoring requires a head frame with a probe fixation; the temporal window is most commonly used
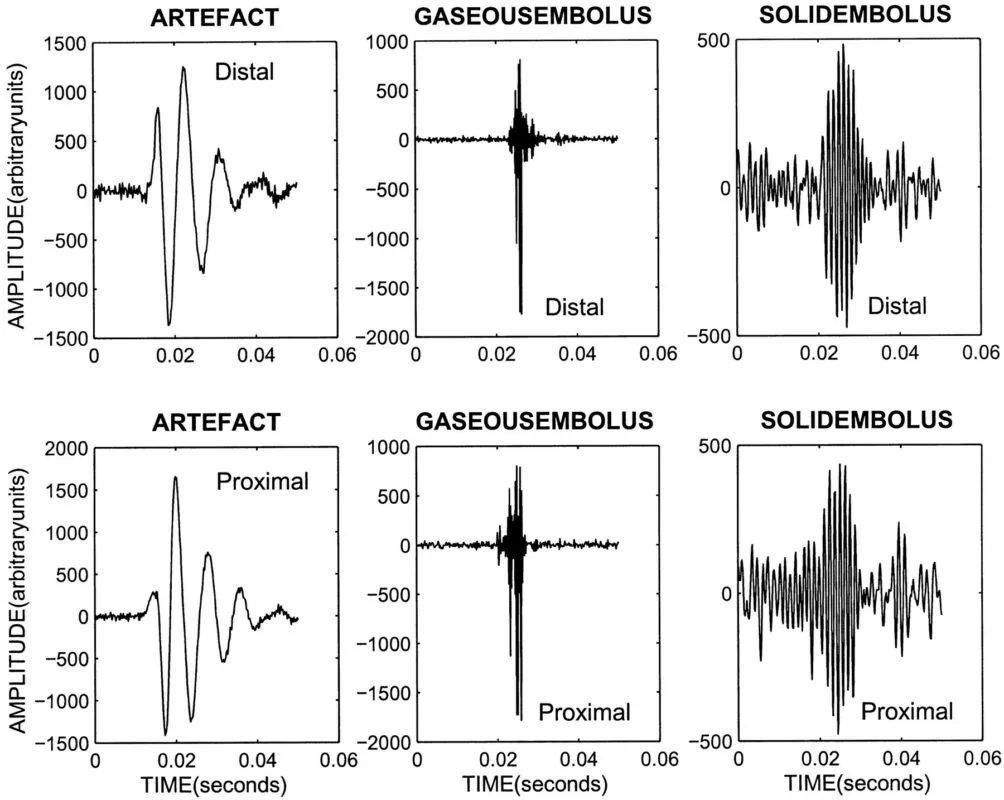
- High-Intensity Transient Signals (HITS) have the following characteristics:
- are unidirectional
- have a typical sound
- duration < 300 milliseconds (usually 2-100 ms)
- amplitude > 3 dB above background (3-60 dB)
- the intensity of the signal can be used to distinguish the type of embolus: solid embolus < gas
- software capable of distinguishing HITS from artifacts is used to register and evaluate the recording
- differentiation of HITS from artifacts is possible by using multi-gate scanning, which simultaneously records from multiple sample volumes at different depths. The signal from an embolus shows a typical delay as it moves in the artery, while artifacts have no time delay)
- variable protocols exist for TCD machine settings
- duration 20-120 minutes (up to 8 hours), single or multiple examinations
- bilateral or unilateral monitoring, usually of the M1 segment (50-59 mm depth)
- 2MHz probe
- scale -100-150 cm/s (PRF 6.5 kHz)
- lower gain
- low acoustic intensity ( 33mW/cm2)
- sampling volume 4-12
- 64-point FFT of 10ms length, 60% overlap
- high-pass filter
Microemboli in carotid stenosis
- microembolizations may occur transiently
- absence of HITS during monitoring does not definitively rule out the high-risk plaque
- rate of HITS detection depends on the duration and number of monitoring sessions
- recently symptomatic carotid stenosis is associated with the highest rate of HITS (however, the number of embolic signals decreases with time)
- detection of HITS is more frequent in patients with cerebral infarction than in those with TIA and significantly more frequent than in asymptomatic stenoses
- the incidence of microembolic signals increases with the severity of stenosis
- > 70% = 23.5%
- 50-70% = 3.4%
- administration of IV antiplatelet agents (ASA) in patients with TIA or minor stroke leads to a reduction of microembolic signals
- presence of microembolic signals in asymptomatic stenosis >50% is an independent predictor of ipsilateral stroke/TIA and may support an indication for CEA/CAS (such patients are likely to benefit from the procedure)
- in the ACES trial, the annual risk of ipsilateral stroke/TIA was 7.1% (HITS+) vs. 3% [Markus, 2010]
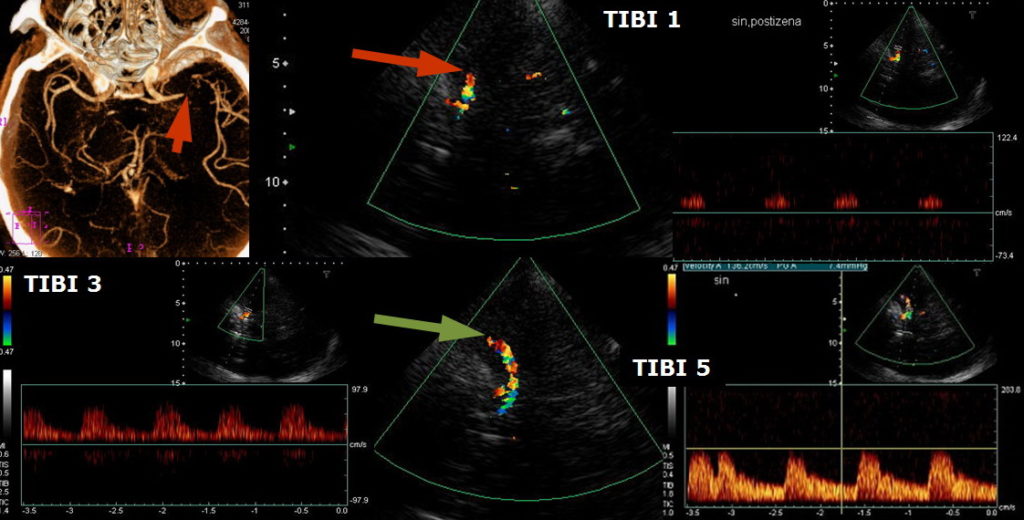
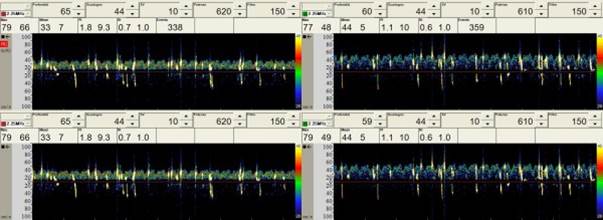
Periprocedural monitoring
- monitoring of flow through cerebral arteries (most commonly the MCA) during surgery or endovascular procedures such as:
- carotid endarterectomy (CEA) or carotid artery stenting (CAS)
- cardiac surgery
- neurosurgery
- a fixation frame is required; bilateral monitoring is preferred
- the following parameters are assessed:
- flow velocities (PSV, EDV, Vmean) and their changes during and post-procedure
- not only pathologically low but also pathologically high values (hyperperfusion) can be observed
- not only pathologically low but also pathologically high values (hyperperfusion) can be observed
- pulsatility index (PI) and resistance index (RI)
- decreased PI and RI indicate hyperperfusion syndrome (with markedly increased PSV) or proximal occlusion/stenosis (with decreased PSV)
- increased PI and RI indicate distal occlusion
- decreased PI and RI indicate hyperperfusion syndrome (with markedly increased PSV) or proximal occlusion/stenosis (with decreased PSV)
- other pathological phenomena such as microembolic signals, arrhythmias, etc.
- flow velocities (PSV, EDV, Vmean) and their changes during and post-procedure
- detects microemboli (HITS)
- detects hypoperfusion (sudden decrease of PSV in the MCA) with the potential need for shunting
- the critical moment during CEA represents the clamping of the artery, during which the flow changes in the MCA occur
- mean flow velocity (Vmean) decrease after clamping should be <60% of the baseline velocity + the Vmean should remain > 30 cm/s
- if these conditions are met, it is safe to operate without a shunt
- when operating under local anesthesia, immediate shunting is not obligatory, even with significant flow reduction post-clamping. However, immediate shunting is required if the patient’s state of consciousness or mobility alters. This strategy may reduce the rate of shunting.
- sudden hypoperfusion in the MCA (indicated by markedly decreased velocities and systolic acceleration) detected at the end of the procedure may indicate arterial thrombosis with the surgical field ⇒ acute revision is required
- detects hyperperfusion (caused by altered vasomotor autoregulation)
- ↓ resistance and ↑flow velocities occur after restoration of flow in the stenotic segment ⇒ ↑ risk of hemorrhage
- strict BP control is crucial → Cerebral hyperperfusion syndrome (CHS)
- continuous ultrasound monitoring may also have the potential to reduce thromboembolic risk (see above)
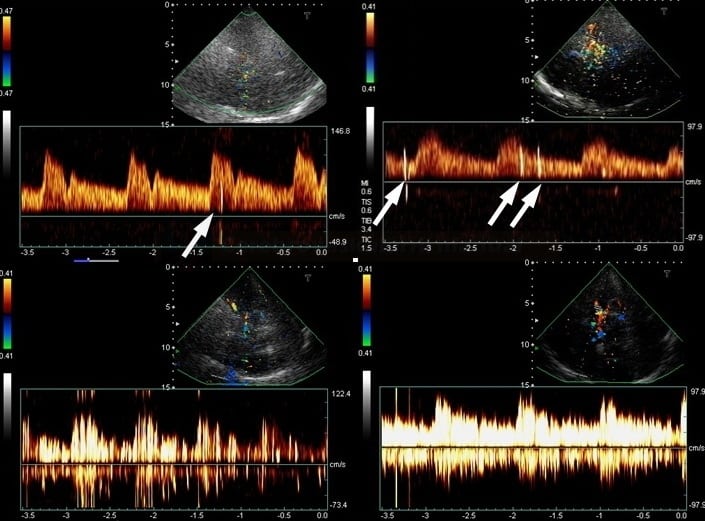
TCD/TCCD bubble test
- the TCD/TCCD bubble test is used to detect right-to-left shunts, particularly Patent Foramen Ovale (PFO)
- the test simulates paradoxical embolism by administering air microbubbles (gas emboli are thus detected)
Balloon test occlusion
- the Balloon test occlusion (BTO) is performed to determine whether an artery (usually ICA or CCA) can be temporarily or permanently occluded without inducing cerebral ischemia
- in addition to serial neurological evaluations, TCCD/TCD monitoring of the ipsilateral MCA may be used to rule out significant hypoperfusion after ICA/CCA occlusion