ISCHEMIC STROKE / PREVENTION
Management of asymptomatic carotid stenosis
Updated on 07/05/2024, published on 03/01/2022
- carotid artery atherosclerotic disease (CAAD or CAD) is a substantial stroke risk factor (classified as TOAST 1)
- extracranial carotid artery stenosis is associated with ~ 20% of ischemic strokes
- classification of carotid artery disease
- asymptomatic x symptomatic (signs/symptoms of cerebral or ocular ischemia in the past 6 months)
- low risk x high risk
- high CV risk features:
- significant carotid stenosis of ≥ 50%
- detection of vulnerable plaque (characteristics are discussed below)
- additional uncontrolled CV risk factors (atrial fibrillation, diabetes mellitus, metabolic syndrome, etc.)
- identifying and treating carotid artery disease is an important part of preventing stroke
Stroke risk and prevalence of asymptomatic carotid stenosis
- the prevalence of carotid artery atherosclerotic disease depends on the population studied and the stenosis threshold used for inclusion
- the prevalence of asymptomatic stenosis > 50% is 2-8%, and the prevalence of asymptomatic stenosis > 80% is 1-2%
- the prevalence of stenosis > 50% increases with age
- < 60 years – 0.5% , > 80 years – 10%
- the risk of stroke in patients with asymptomatic carotid stenosis > 50% is about 1-2%/year (rate of coronary events is 7%)
- compared to symptomatic stenosis, the risk is much lower
- according to a population-based study and meta-analysis, the risk of stroke increases with the degree of stenosis – the risk of 80-99% stenosis is higher than that of 50-79% stenosis [Howard, 2021]
- see below for individual parameters of high-risk plaques
- in addition to the increased risk of stroke, patients with asymptomatic carotid stenosis also have an increased risk of MI ⇒ intensive systemic therapy is essential
- in general, prophylactic CEA is not required before surgery using general anesthesia (GA) or extracorporeal circulation (ECC) → Carotid endarterectomy
Screening for asymptomatic carotid stenosis
- screening for asymptomatic carotid stenosis in the general population is not recommended by the U.S. Preventive Services Task Force (due to unknown cost-benefit)
- the situation may vary from country to country.
- it is recommended to screen selected patients with:
- symptomatic peripheral artery disease (PAD), coronary artery disease (CAD), or atherosclerotic aortic aneurysm
- ≥ 2 of the following CV risk factors, including arterial hypertension, hyperlipidemia, smoking, family history of early-onset atherosclerotic disease in a first-degree relative, or family history of ischemic stroke
- symptomatic peripheral artery disease (PAD), coronary artery disease (CAD), or atherosclerotic aortic aneurysm
- repeated duplex examination:
- patients with carotid stenosis >50% should be assessed annually for progression and response to therapeutic intervention.
- patients with normal/mildly increased baseline IMT should not have repeat carotid Doppler (because of the very slow rate of IMT increase)
Best medical therapy
- best medical therapy (BMT) is the mainstay of carotid stenosis management (it also leads to a reduced risk of MI)
- antiplatelet drugs
- intensive management of vascular risk factors
- the relatively low risk of stroke was reported with such an approach (~1.68%/year) [Raman, 2013]
Antithrombotic therapy
Antiplatelet drugs
- aspirin 75-325 mg/d
- aspirin intolerance or contraindication: clopidogrel (75mg) or ticlopidine
- clopidogrel resistance/allergy: consider ticagrelor (BRILIQUE)
Anticoagulant drugs
- antiplatelet + low-dose anticoagulant:
- ASA + rivaroxaban 2×2.5 mg in selected patients
- in the COMPASS trial, carotid disease included both asymptomatic stenoses and patients with previous revascularization. The combination was maximally effective in patients with ‘symptomatic PAD’ defined as the co-existence of symptomatic peripheral artery disease of lower extremities and carotid artery disease
- ASA + rivaroxaban 2×2.5 mg in selected patients
- anticoagulants alone: not recommended
- antiplatelets + standard-dose anticoagulants: not recommended
Vascular risk factors management
Carotid artery revascularization
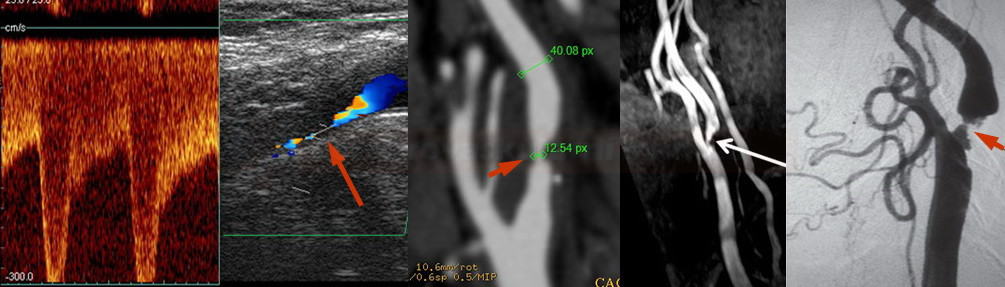
- carotid artery revascularisation (CAR) = carotid endarterectomy (CEA) or carotid angioplasty and stenting (CAS)
- carotid revascularisation should only be performed in a ward with low perioperative complications (<3% for asymptomatic stenosis)
- CEA and CAS have similar safety, but CEA seems to be a little safer (ACST-2)
- the SAPPHIRE and CREST trials demonstrated the similar safety of CAS and CEA
- ACT 1 and ACST-2 trials demonstrated comparable safety even in asymptomatic stenoses [Rosenfield, 2016]
- on the other hand, CEA appears somewhat safer than CAS according to an analysis of 5 randomized trials [Moresoli, 2017]
- patients with more extensive white matter lesions on CT/MRI (ARWMC score ≥ 7) should be treated with CEA (ICSS trial)
- when considering any intervention, several aspects should be considered that may help to select patients with the highest benefit from revascularisation (→ see here)
- degree of stenosis + plaque vulnerability should be evaluated (Brinjikji, 2016)
| Content available only for logged-in subscribers (registration will be available soon) |
All cited markers of high stroke risk associated with asymptomatic carotid stenosis:
- lack specificity
- have not been assessed in conjunction with the current optimal medical therapy
- have not been shown in randomized trials to identify those who will benefit from a carotid revascularization procedure in addition to optimal medical therapy
Stenosis degree
| Content available only for logged-in subscribers (registration will be available soon) |
Progression over time
- risk of stenosis progression is substantial and unpredictable and increases over time
- several studies showed a higher risk of stroke in progressive stenoses > 80%
- rapidly progressive stenoses, in particular, are associated with a higher risk of ischemic stroke
- the data justify the use of serial duplex scans to follow carotid stenosis; however, there is no consensus on the appropriate intervals
- according to some recommendations, the scan should be repeated every 6-12 months for stenosis > 50% (AHA/ASA 2014 IIa/C)
Plaque morphology
| Content available only for logged-in subscribers (registration will be available soon) |
Proof of microembolization on TCD/TCCD
- the association of embolic signals with the risk of infarction has been demonstrated in both symptomatic and asymptomatic stenoses
[Markus, 2017]
- detection of ≥ 2 embolic signals per hour indicates an unstable plaque or a plaque with concurrent thrombosis
- the annual risk of stroke risk in this condition is up to 8%
- embolic signals are more common in unstable, hypoechoic, exulcerated, poorly calcified plaques
- the use of TCD Holter may be helpful in these conditions
Evidence of silent ischemia
- some authors suggest that the incidence of silent ischemia on CT/MRI correlates with the degree of stenosis and the type of plaque (especially with exulcerated plaques)
- MRI is more sensitive than CT
- according to the ACSRS trial, the average incidence of stroke in patients with stenosis > 60% with silent ischemia is 3.6%/year compared to 1.3%/year in those without silent ischemia
- no difference was seen for stenosis < 60%
- in contrast, silent ischemia was not found to be related to stenosis severity in the ACAS trial
- although the benefit of revascularisation in patients with silent lesions has not been demonstrated in trials, their detection supports the indication for CEA/CAS in clinical practice
Impact of contralateral carotid stenosis or occlusion
| Content available only for logged-in subscribers (registration will be available soon) |
Gender
- in the ACAS trial, women had a higher surgical risk than men ( 3.6% vs. 1.7%); this has been reported in some smaller studies as well, while others have not confirmed these findings
- some advantages of CEA over CAS in women are discussed
- while there is no solid consensus, there is a tendency towards greater restraint in women when indicating revascularization
- women who undergo CEA do not need to discontinue postmenopausal HRT
Age
- CEA/CAS may not be contraindicated by advanced age alone; biological status, life expectancy, and other factors should be considered
- surgery is more common in patients < 75 years of age
- in the ACAS trial, age > 80 years was a contraindication
- in the ACST trial, the benefit was relatively small in patients > 75 years (ARR 3.3%/5 years)
- for asymptomatic stenoses, a higher mortality rate was reported in patients >75 years compared to those <75 years [Rajamani, 2013]
- in the ACAS trial, age > 80 years was a contraindication
Intracranial flow and vasomotor reactivity (CVR)
- data indicate a higher risk of stroke in patients with impaired cerebral vasomotor reactivity (VMR or CVR) and impaired intracranial flow
[Gupta, 2012]
- ~4 times higher risk of stroke/TIA (5.7% per year with an average follow-up of 24 months)
- methods used to assess CVR (VMR):
- transcranial Doppler (TCD/TCCD)
- hyperventilation/apnea test
- breath holding test
- acetazolamide (ACZ)
- hyperventilation/apnea test
- other imaging methods performed before and after administration of the vasodilatory agent (acetazolamide-challenged methods)
- MR perfusion or CT perfusion
[Kang, 2008]
- severe stenosis may sometimes manifest as false ischemic penumbra (FIP) on baseline CTP [Mosqueira, 2017]
- SPECT/PET
- MRI ASL/BOLD sequences
- MR perfusion or CT perfusion
- transcranial Doppler (TCD/TCCD)