GENERAL NEUROLOGY
Rostrocaudal deterioration
Updated on 06/07/2024, published on 18/11/2023
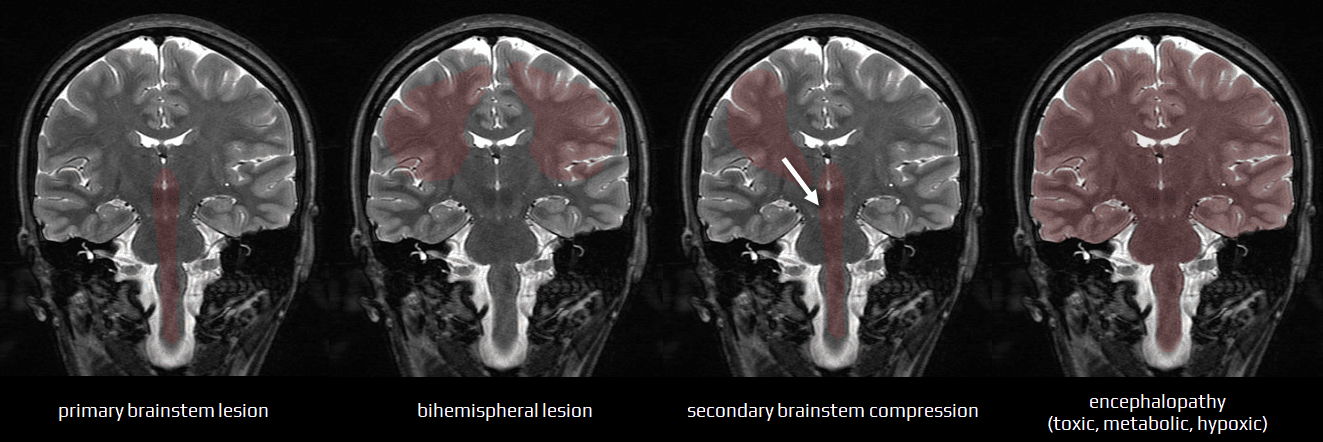
- disorders of consciousness are caused by dysfunction of the ascending reticular activating system (ARAS) in the brainstem, its impaired connections with the cerebral cortex (reticulo-cortical pathways), or generalized cerebral dysfunction
- dysfunction in these areas can result in a spectrum of impaired consciousness, ranging from mild confusion to deep coma
- a lesion in one hemisphere typically causes coma only if there is secondary damage to the brainstem or its connections to the cerebral cortex
Impaired consciousness can be caused by:
- infratentorial lesions (direct brainstem lesion or external compression)
- dysfunction of brainstem reticular formation and other structures (cranial nerve centers, ascending and descending tracts, and autonomic centers)
- the combination of symptoms and signs can help localize the lesion and determine the extent of damage.
- small, localized lesions cause well-described brainstem syndromes (Wallenberg, Dejerine. etc.)
- these syndromes are typically of vascular origin corresponding to specific arterial territories, though they may also result from tumors or inflammatory processes
- these syndromes are typically of vascular origin corresponding to specific arterial territories, though they may also result from tumors or inflammatory processes
- extensive lesions, like hematomas, usually cause coma and extensive neurological impairment, preventing precise localization of the lesion
- bilateral supratentorial lesions ± secondary compression of the brainstem
- supratentorial unilateral space-occupying lesion with secondary compression of the brainstem
- compression leads to brainstem dysfunction, which progresses in a rostrocaudal direction (rostrocaudal deterioration) – this will be discussed further
- compression leads to brainstem dysfunction, which progresses in a rostrocaudal direction (rostrocaudal deterioration) – this will be discussed further
- diffuse encephalopathy
- toxic, metabolic, or hypoxic encephalopathies interfere with metabolic processes of the cerebral cortex and brainstem
- initial changes may be functional (functional transsection) but may become irreversible due to complications like edema, hemorrhage, or ischemia
- the neurological examination of the unconscious patient differs from a standard examination in several key aspects:
- scale-based evaluation of consciousness level (GCS, Beneš-Drábek, Ramsay scale, etc.)
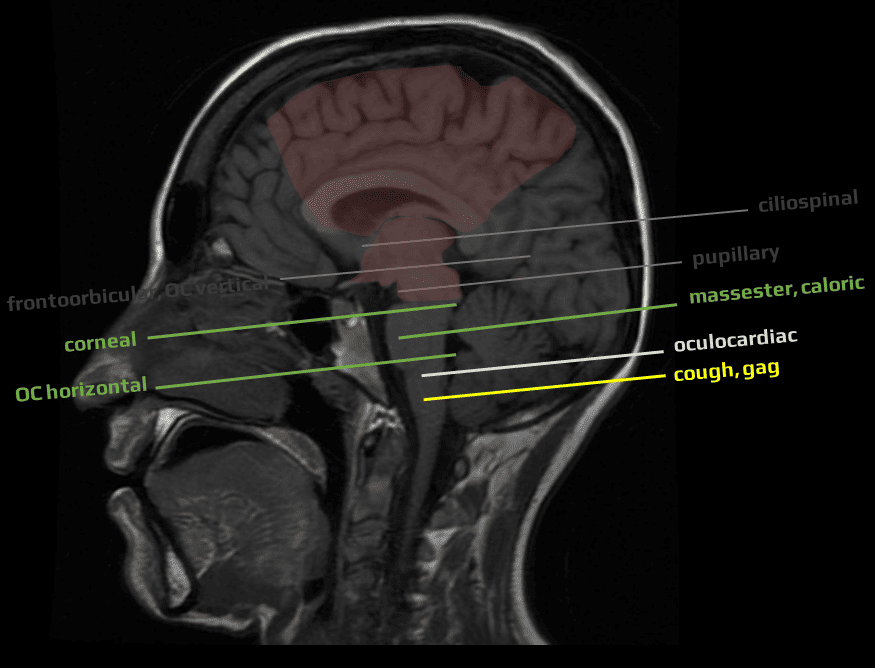
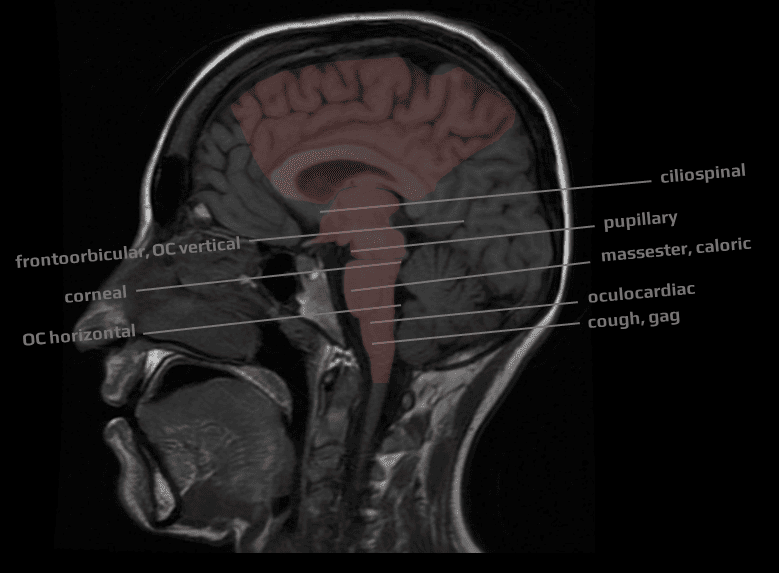
- assessment of brainstem reflexes
- testing of specific motor and oculomotor responses (→ pupillary response in brainstem lesions)
- assessment of the respiratory pattern if the patient is not already on mechanical ventilation
- this examination aims to:
- evaluate the level of consciousness
- determine the lesion’s location and extent
- suggest the likely cause (structural lesion vs. diffuse metabolic disorder or intoxication)
- repeated examinations are crucial for assessing the progression or regression of the impairment (course of rostrocaudal deterioration syndrome, differentiation between functional and permanent lesion)
- evaluate the level of consciousness
- differentiation and topical assignment of the symptoms become imprecise with increasing lesion extent; presentation with coma and decerebration complicates determining the extent and potential reversibility of the disorder
- serial examination of brainstem reflexes and motor and oculomotor responses may help to assess progression and refine prognosis prediction
Assessment of rostrocaudal deterioration in space-occupying supratentorial lesions
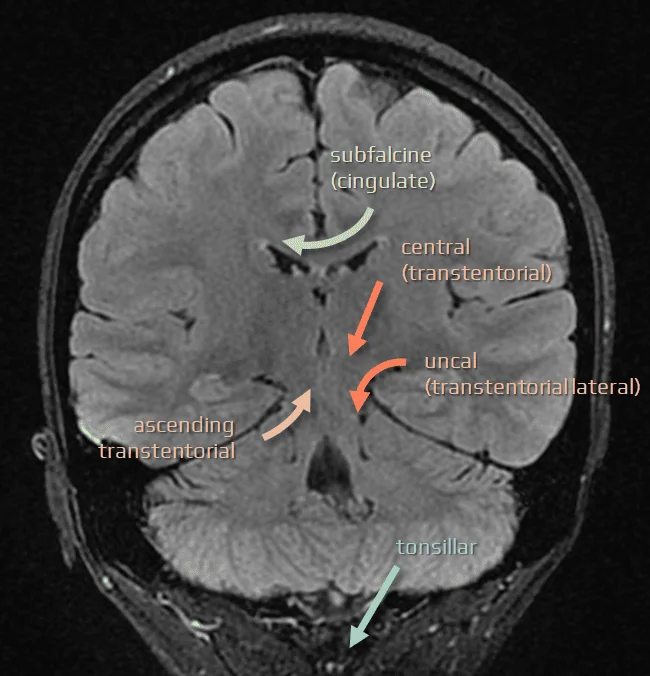
- supratentorial space-occupying lesions are associated with herniation, causing a typical pattern of cerebral rostrocaudal deterioration
- the initial cortical lesion (such as hematoma, ischemia, tumor, or contusion), along with secondary injuries (edema, hemorrhage, or ischemia due to artery or vein compression), leads to compression of surrounding tissue and then extends laterally (to the contralateral hemisphere) or caudally to the diencephalon and brainstem
- the compression causes caudally spreading transsectional disorders (functional or structural), with brainstem reflexes becoming non-excitable accordingly
- the process is known as McNealy and Plum’s (~ 1960) concept of rostrocaudal development of cerebral dysfunction
- transient functional disorder without persistent morphological alterations can occur in cases where secondary involvement of the brainstem is brief; longer-lasting and more extensive damage typically results in permanent dysfunction (due to structural lesion)
- regardless of the primary process’s nature, secondary damage often becomes predominant, influencing the patient’s course and outcome
- the final stage of craniocaudal deterioration is complete loss of brainstem function (brainstem death)
- understanding the various patterns of cerebral herniation is essential for etiologic and topical diagnosis
- brain imaging (CT or MRI) is effective in diagnosing cerebral herniation, guiding therapeutic decisions, and improving prognosis prediction