OTHER VASCULAR DISORDERS
Posterior Reversible Encephalopathy Syndrome (PRES)
Updated on 10/07/2024, published on 23/09/2023
- clinical-radiologic syndrome
- sometimes called reversible posterior leukoencephalopathy syndrome ( RPLS) or acute hypertensive encephalopathy
- the name may be misleading:
- pathologic changes may extend beyond the posterior regions
- some patients may develop permanent brain damage with neurological deficits
- pathologic changes may extend beyond the posterior regions
- diagnosis is based on imaging methods (mainly typical MRI findings on T2 and FLAIR)
Pathophysiology of PRES
- there is no clear, exact etiology; different conditions can likely lead to the same clinical presentation:
- decompensated hypertension (~ BP > 170-190 mm Hg) impairs cerebral autoregulation, leading to vasodilatation, endothelial dysfunction, and subsequent vasogenic edema
- reactive vasoconstriction is followed by hypoperfusion [Bartynski, 2008]
- a systemic inflammatory response with endothelial dysfunction (a theory supported by the association with sepsis, pre-eclampsia, and autoimmune diseases), where released vasoactive substances increase vascular permeability (⇒ edema). In these patients, PRES may occur even with normal BP! [Kurukumbi, 2013]
- changes are generally reversible with early therapy; prolonged duration may lead to ischemia or hemorrhage
- lesions are typically localized in the parietal and occipital lobes (but may also occur in the frontal and temporal lobes, cerebellum, and basal ganglia) [Legriel, 2011]
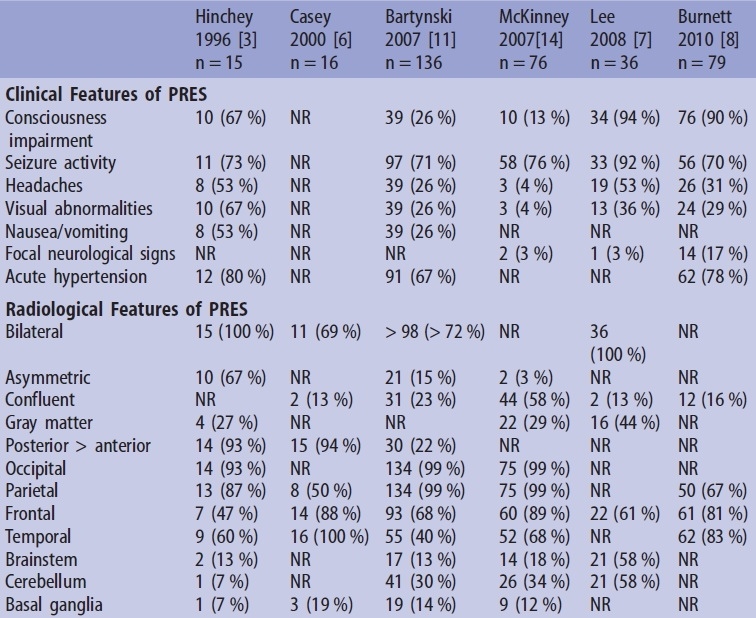
| Association of PRES with the following conditions: | |
|
|
Clinical presentation
- headache (26%)
- moderate-to-severe intensity
- often showing poor response to analgesics
- nausea, vomiting
- encephalopathy with delirium/quantitative disturbances of consciousness (ranging from somnolence to coma) – exclude NCSE!
- epileptic seizures (in up to 90% of cases, status epilepticus occurring in ~ 3% of cases)
- visual disturbances (26%)
- hallucinations
- cortical blindness, which may be associated with its denial (Anton-Babinski syndrome)
- hemianopsia
- papilledema with retinal hemorrhages and exudates
- focal neurologic signs (3-17%)
- vertigo, ataxia, etc.
- poorly controlled blood pressure (67-80%)
- no correlation has been observed between mean BP and severity of radiologic changes
- hypertensive crisis may precede neurologic signs by ≥ 24 h
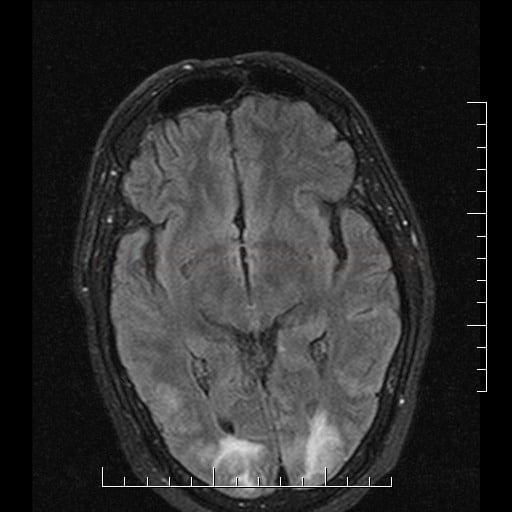
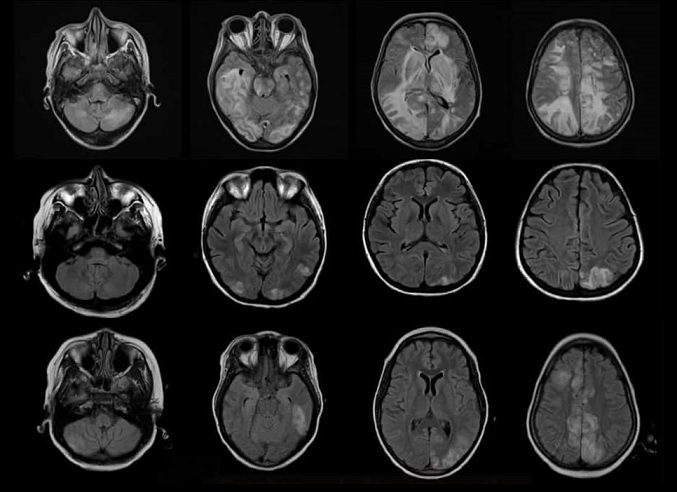
- hyperintense lesions (indicative of edema) on FLAIR, T2, DWI, and ADC
- DDx of acute ischemia (with a hypointense lesion in ADC map)
- DWI may exhibit T2 shine-through
- T1 – hypointense
- lesions are multiple and bilateral, typically in parieto-occipital regions (70-90% of cases)
- lesions can also be found in watershed areas of the frontal and temporal lobes, in the cerebellum, basal ganglia, and thalamus [Raman, 2017]
- changes are observed in both cortical and subcortical regions.
- T1C+ – variable enhancement is seen in ~30% of patients
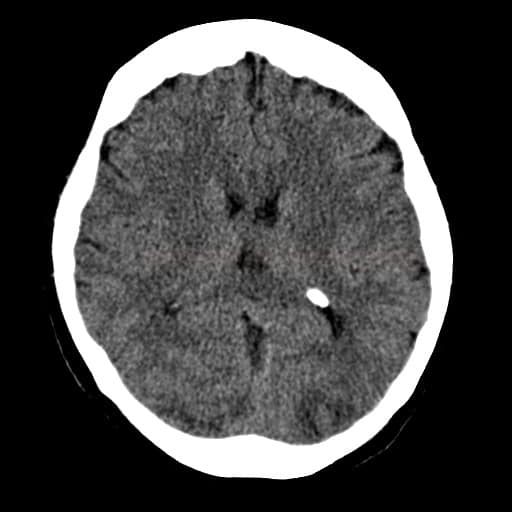
- hemorrhages are detected in approximately 15% of cases [Hefzy, 2009]
- GRE can effectively detect microbleeds
- a combination of PRES and acute ischemia is reported in ~ 10-25% of cases
- in case of ambiguity, MRI follow-up is appropriate, as radiological changes typically regress with treatment
- MRA may reveal a vasculopathic pattern with focal vasoconstrictions/vasodilatation (which may cause difficulty in DDx of vasculitis)
Other diagnostic methods
- lumbar puncture
- blood tests (e.g., autoantibodies, Ca2+/S, Mg2+/S, etc.)
- brain biopsy if an infiltrative process is suspected
Differential diagnosis
- PRES is characterized by vasogenic edema involving the parietal and occipital lobes without clear territorial distribution, accompanied by symptoms such as headache and seizures
- compared to ischemia, the foci in PRES appear hyperintense on the ADC map
- ischemia or hemorrhage may develop as complications of PRES
- compared to ischemia, the foci in PRES appear hyperintense on the ADC map
- exclude:
- severe hypoglycemia
- acute posterior circulation stroke
- progressive multifocal leukoencephalopathy (PML)
- sinus thrombosis
- gliomatosis cerebri
- hypoxic-ischemic encephalopathy
- SMART syndrome (stroke-like migraine attacks after radiotherapy)
- inflammatory cerebral amyloid angiopathy
→ DDx of leukoencephalopathies see here
Management
- with early treatment, the prognosis is good
- prolonged duration may lead to irreversible neurological deficits
Elimination of the cause of PRES
- the cornerstone of therapy is addressing and eliminating the provoking factors:
- stabilize and maintain blood pressure within a target range; prevent significant fluctuations
- identify and discontinue toxic drugs
- induce delivery in case of eclampsia
- correct underlying metabolic disorders
- stabilize and maintain blood pressure within a target range; prevent significant fluctuations
Symptomatic therapy
- antihypertensive therapy → hypertensive crisis therapy see here
- the goal is to reduce mean arterial pressure (MAP) by 20-25% in the first 1-2 hour(s)
- preferably use IV urapidil or labetalol
- the goal is to reduce mean arterial pressure (MAP) by 20-25% in the first 1-2 hour(s)
- symptomatic treatment of seizures → see here
- long-term antiseizure medication is usually unnecessary
- correct potential hypomagnesemia
- consider antiedema therapy based on clinical status and MRI findings
- corticosteroids may theoretically improve edema, but there is no hard evidence of their efficacy

Prognosis
- most patients improve within 12-24 hours (up to several days) with prompt treatment
- MRI findings may persist for weeks
- delayed treatment can lead to serious complications (ischemic stroke/bleeding) with permanent disability
- death is usually caused by hemorrhage or massive edema in the posterior cranial fossa
FAQs
- PRES is a neurological disorder characterized by variable symptoms such as headaches, seizures, altered mental status, and visual disturbances, caused by vasogenic edema predominantly in the posterior regions of the brain
- PRES is often associated with acute hypertension, renal disease, autoimmune disorders, and the use of certain immunosuppressive or chemotherapeutic agents
- diagnosis is primarily based on clinical presentation and characteristic findings on neuroimaging, particularly magnetic resonance imaging (MRI) showing edema in the posterior regions of the cerebral cortex
- in most cases, PRES is reversible with appropriate management of the underlying cause and supportive care
- however, delays in diagnosis or treatment, severe or prolonged episodes, and certain underlying conditions can lead to irreversible brain damage or other complications
- treatment focuses on managing the underlying cause, such as controlling blood pressure, discontinuing offending drugs, and treating autoimmune diseases or renal dysfunction
- supportive care for symptoms like seizures is also important
- PRES is a rare condition, but its exact prevalence is unknown. It is more commonly reported in patients with acute medical conditions and those receiving specific treatments that affect blood pressure or immune functions
- prevention focuses on managing risk factors, such as controlling blood pressure, monitoring renal function, and carefully using medications associated with PRES.