ISCHEMIC STROKE / ETIOLOGY
Lacunar stroke
Updated on 16/06/2024, published on 02/12/2022
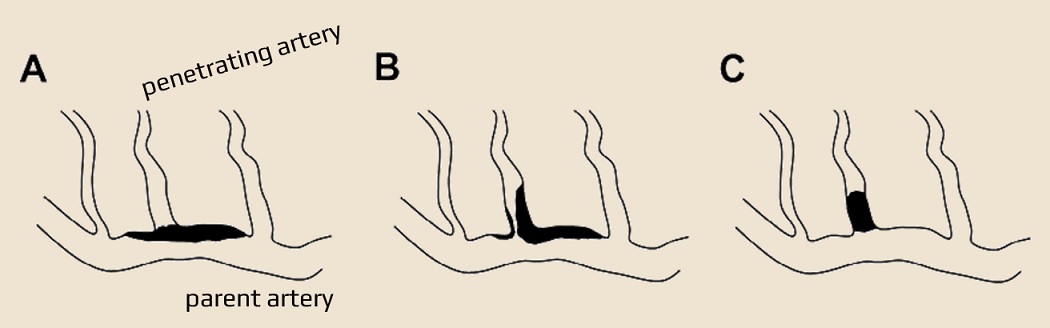
- lacunar stroke (lacunar cerebral infarct – LACI) is defined as a small subcortical lesion ≤ 1.5 cm in diameter, resulting from the occlusion of small penetrating arteries
- penetrating arteries originate at sharp angles from larger vessels, making them anatomically susceptible to stenosis and occlusion
- the term “lacune” was first described in the late 19th and early 20th centuries – it commonly describes a small, chronic cavity that represents the healed phase of a lacunar infarct
- etiology of the lacunar infarct is not necessarily of arteriolopathic origin ⇒ various mechanisms can lead to their occlusion!
- typical lacunar stroke locations correspond to lesions of the lenticulostriate arteries, the anterior choroidal artery, thalamoperforant arteries (TPAs), paramedian branches of the basilar artery, and the Heubner´s recurrent artery (originating from the ACA)
- basal ganglia (globus pallidus, putamen, thalamus, and caudate)
- pons
- subcortical white matter structures (internal capsule and corona radiata)
- penetrating arteries originate at sharp angles from larger vessels, making them anatomically susceptible to stenosis and occlusion
- lacunar stroke syndrome (LACS) is a clinical manifestation of lacunar stroke; the most common syndromes are listed below
Etiopathogenesis
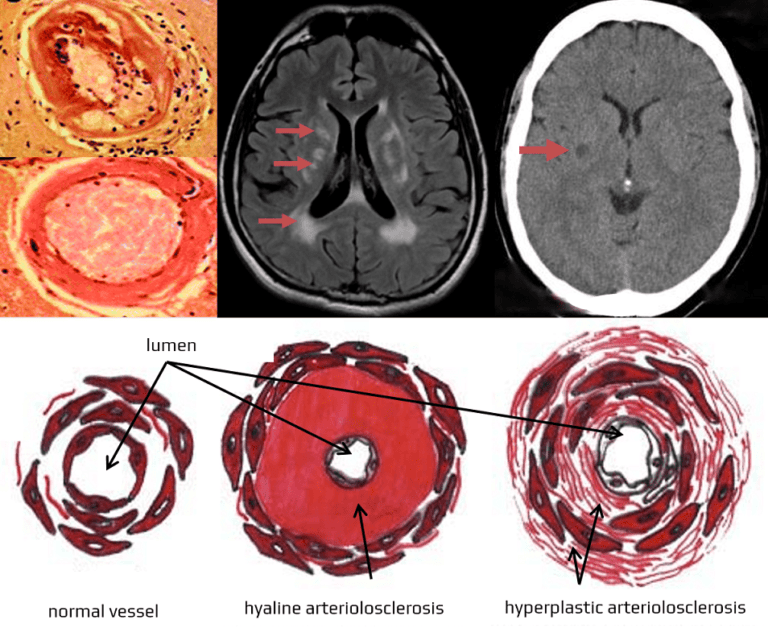
- cerebral small vessel diseases (SVDs) encompass a group of disorders that primarily affect small blood vessels in the brain (small arteries, arterioles, capillaries, and venules)
- cerebral SVD is typically associated with leukoencephalopathy, lacunar strokes, and microbleeds
- the underlying causes may differ:
- sporadic forms
- genetic forms
- both forms result in impaired blood flow, vessel wall damage, and leakage of blood components into brain tissues; these changes lead to significant morbidity and mortality due to stroke and dementia
Clinical presentation
- lacunar infarct symptoms typically have a sudden onset but can also show a more gradual progression
- symptoms usually do not include cortical signs ( agnosia, aphasia, neglect, apraxia, or hemianopsia)
- cortical functions must be tested to differentiate between the MCA stroke and the subcortical stroke (involving structures like the thalamus and internal capsule)
- the most common syndromes associated with lacunar strokes are:
- pure motor hemiparesis
- pure sensory stroke (unilateral numbness of the face, arm, and leg, affecting all sensory modalities)
- ataxic hemiparesis (unilateral limb ataxia that is disproportionate to the strength/motor deficit)
- sensorimotor stroke (unilateral weakness and numbness)
- dysarthria-clumsy hand syndrome (unilateral facial weakness, dysarthria, dysphagia, and dysmetria/clumsiness in one upper extremity)
| Content available only for logged-in subscribers (registration will be available soon) |
- a silent lacunar infarction (SLI) is an incidental finding on imaging without any prior history of stroke symptoms
- silent strokes are much more common than previously believed
- SLIs increase the risk of a future major stroke, and multiple lesions may eventually become symptomatic (lacunar state)
- multiple lesions can affect various aspects of a person’s mood, personality, and cognitive functions (lacunar state / Binswanger’s disease)
Diagnostic evaluation
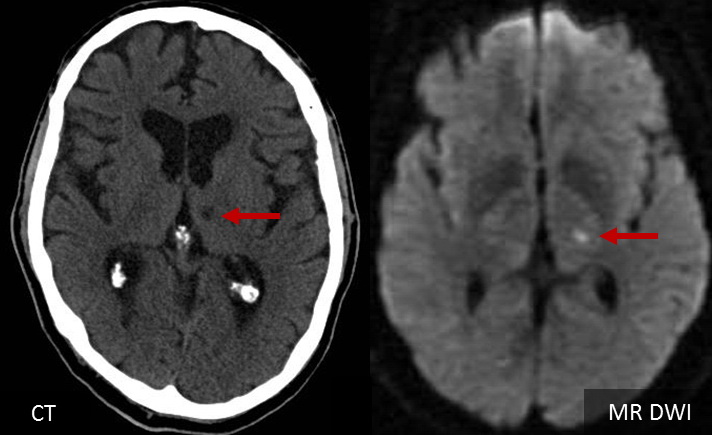
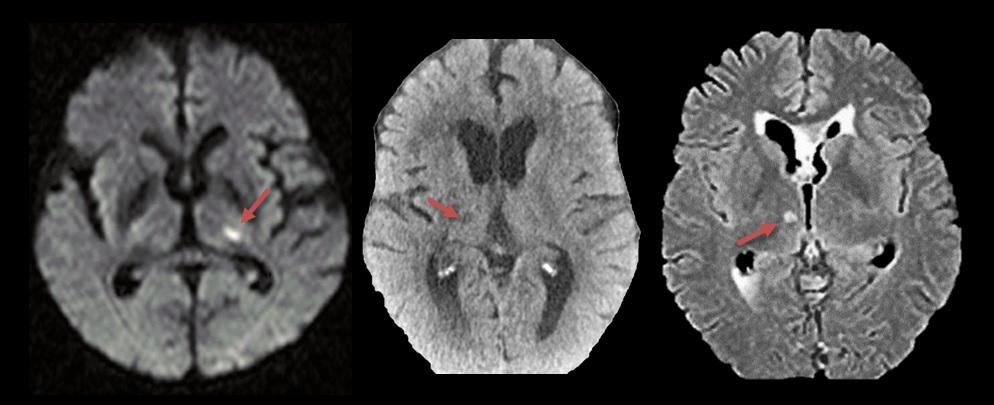
- brain imaging (CT/MRI)
- excludes hemorrhage
- DWI is more sensitive in detecting acute infarcts compared to other MRI sequences or CT scans
- in the acute phase, CT or even MRI may be negative; later, a small noncortical infarct may be visible
- vascular imaging (CTA/MRA)
- excludes large vessel occlusion/stenosis
- small perforating arteries are difficult to visualize effectively with CTA and MRA
- high-resolution MRI can detect ostial microatheroma in penetrating arteries; larger lesions are found in such cases (Sun, 2018)
- the definitive diagnosis is established by a combination of a typical lacunar syndrome + negative findings on CTA/MRA + presence of small, noncortical infarct visible on CT/MRI
- a history of longstanding diabetes, hypertension, and hyperlipidemia is typical
- such a stroke is classified as TOAST 3
- a history of longstanding diabetes, hypertension, and hyperlipidemia is typical
- for young patients without traditional risk factors, further evaluation may be necessary to exclude an embolic source and rare inherited small vessel diseases
Differential diagnosis
- vascular lesions
- large vessel stroke (larger lacune)
- subtle hemorrhage
- non-traumatic convexal SAH
- seizures (cortical symptoms) – symptoms resolve
- complicated migraine events – symptoms resolve
Management
Acute stroke therapy
- IV thrombolysis in eligible patients
- contraindications to IV thrombolysis are the same as for other stroke subtypes
- contraindications to IV thrombolysis are the same as for other stroke subtypes
- single or dual antiplatelet therapy is recommended for patients ineligible for thrombolysis
- routine symptomatic treatment of acute stroke + early rehabilitation with speech and physiotherapy
Prevention of cerebrovascular disease
- antiplatelet therapy – according to the CHANCE and POINT trials, dual antiplatelet therapy (DAPT – ASA+CLP) for 3 weeks followed by single antiplatelet therapy provides the best results
- aggressive treatment of other vascular risk factors (such as hypertension, diabetes, dyslipidemia)
- high-dose statin
- aggressive treatment of hypertension (target BP of <130/80 mmHg in the absence of significant extra-or intracranial stenosis and if tolerated)