GENERAL NEUROLOGY
Lesions of the corpus callosum
Updated on 18/05/2024, published on 14/05/2024
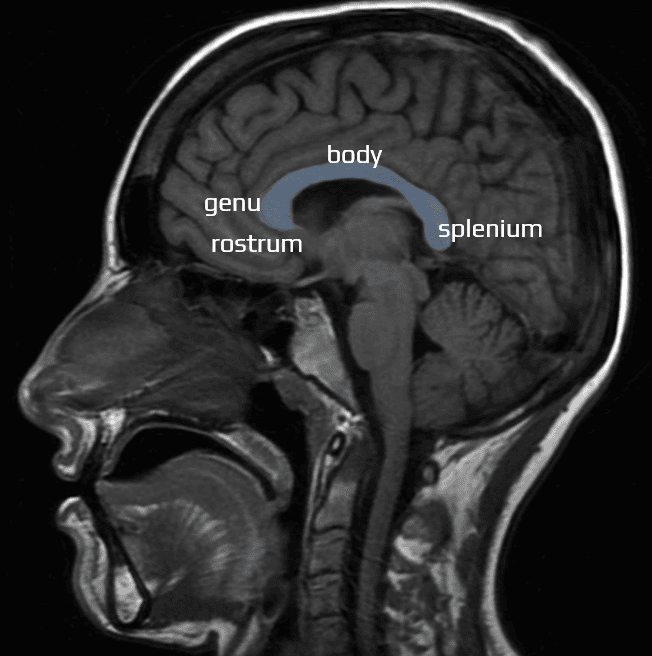
- corpus callosum facilitates communication between the two hemispheres and integrates motor, sensory, and cognitive information
- isolated lesions of the corpus callosum are rare and may represent transient responses to injury or myelination abnormalities
- more common butterfly lesions involve the corpus callosum and both cerebral hemispheres—a pattern associated with aggressive tumors, demyelination, and traumatic brain injury (TBI)
- unenhanced CT is a first-line neuroimaging modality
- CT can help characterize hemorrhage, edema, mass effect, calcification, and necrosis
- MRI provides more detailed information regarding tissue structure and composition, using various pulse excitation sequences, such as FLAIR, to distinguish abnormal signals in the corpus callosum from adjacent CSF in the lateral ventricles
- administration of IV contrast material is useful for the characterization of neoplastic and vascular lesions, which may show characteristic patterns of enhancement
- this article reviews the causes and imaging characteristics of lesions involving the corpus callosum
Vascular |
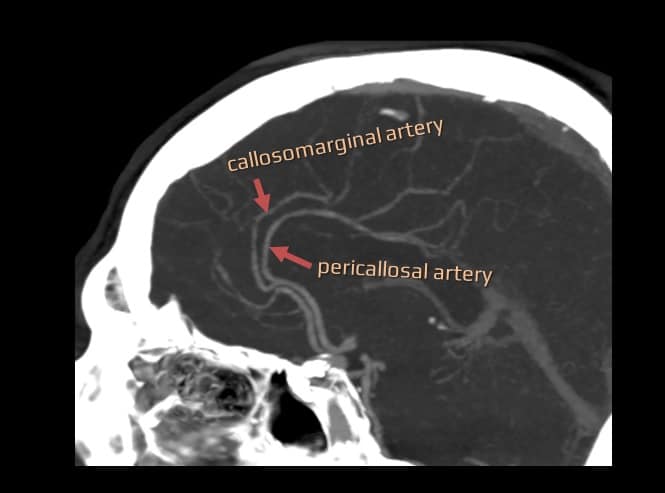
The corpus callosum is supplied by multiple penetrating vessels arising from both the anterior and posterior circulation branches
- because of a rich collateral blood supply, corpus callosal infarcts are rare and associated with systemic vasculitides, shower emboli, major ischemic stroke, or subfalcine herniation with mass effect and secondary damage
- the splenium is most commonly affected, followed by the body and genu
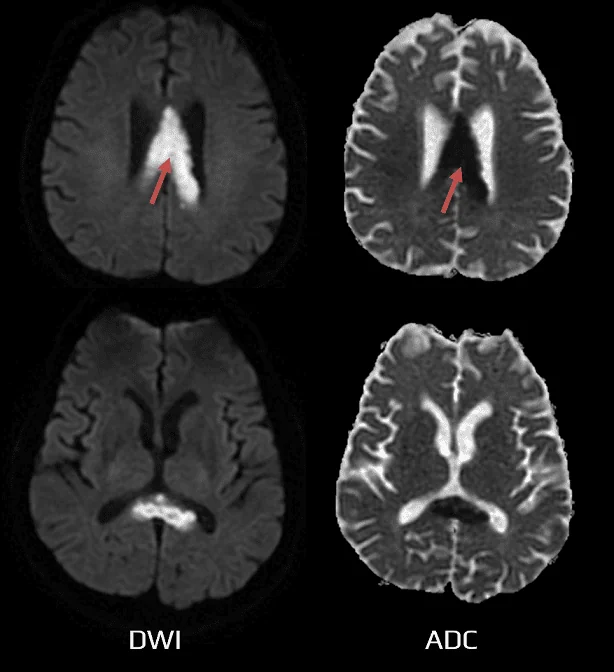
- MRI shows a typical DWI lesion, followed by edema with T2 hyperintensity and T1 hypointensity; contrast enhancement is variable but more likely in the acute phase
- the corpus callosum is involved in large ischemias affecting either hemisphere or very rarely in isolation (Isolated corpus callosum infarction – ICCI)
Isolated Corpus Callosum Infarction (ICCI)
- a rare disorder varying in extent and location (Yang, 2014)
- genu x corpus x splenium (and combinations thereof) – depending on the location of ischemia, it can be determined whether the anterior or posterior circulation is affected
- uni- or bilateral
- symptoms are often nonspecific, sometimes resembling encephalopathy (DDx: tumor, infection)
- various etiologies (embolism, atherosclerosis, moyamoya, hyperviscosity syndrome)
- midline and parasagittal aneurysms (located in the distal ACA or AcomA) can occasionally rupture into the corpus callosum
- non-enhanced CT is useful for the diagnosis of subarachnoid hemorrhage; CT/MR angiography helps localize the bleeding aneurysm that needs to be treated (coiling x clipping)
- cerebral vasospasm may provoke additional cerebral ischemia (Delayed Ischemic Deficit – DID), which also may affect the corpus callosum
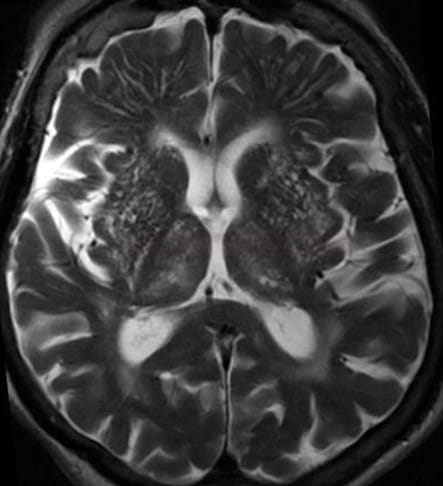
- cerebral arteriovenous malformations (AVMs) involve the corpus callosum in ~ 10% of cases
- nonenhanced CT shows hemorrhage, edema, mass effect, and calcifications
- CTA or time-of-flight MRA can help delineate the feeding arteries, central nidus, and draining veins
- MRI may also show magnetic susceptibility artifacts in regions of calcification
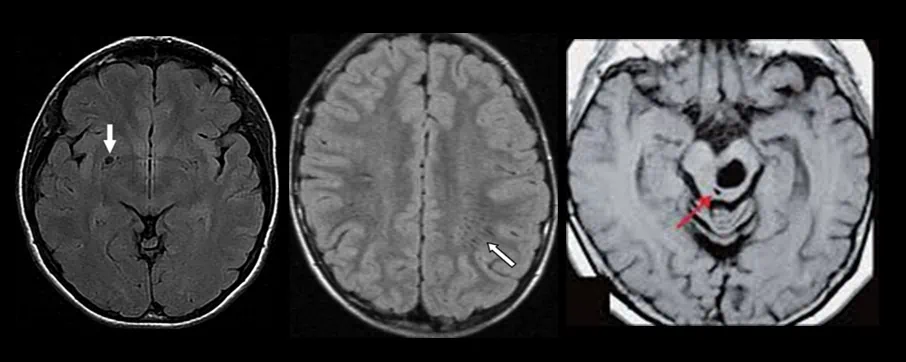
- small hyperintense lesions on FLAIR in the anteroinferior portion of the splenium commonly occur in patients with small-vessel ischemic disease
- lesions correspond to subependymal gliosis
- there is an association with periventricular white matter disease (leukoaraiosis), which appears hypodense on CT and hyperintense on T2-weighted MRI
Neoplastic lesions |
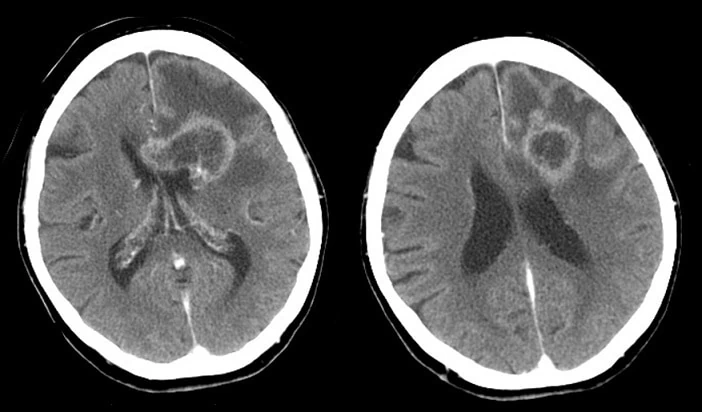
- glioblastoma multiforme (GBM) is a common, aggressive primary brain tumor in adults (grade IV based on WHO classification)
- tumor may involve both cerebral hemispheres extending across the corpus callosum, producing a typical butterfly appearance
- imaging:
- CT – an irregular, heterogeneous mass with peritumoral vasogenic edema or mass effect and possible internal areas of necrosis, calcification, and hemorrhage
- MRI – heterogeneously T1 hypointense and T2 hyperintense, with possible foci of susceptibility, vascular flow voids, and irregular contrast enhancement
- gliomatosis cerebri is a slow-growing, diffuse form of glioma, classified as WHO grade III; it infiltrates ≥ 2 lobes and shows minimal contrast enhancement
- primary CNS lymphoma is a rare, aggressive neoplasm preferentially affecting usually immunocompromised patients
- it may involve or extend through the corpus callosum
- imaging characteristics:
- CT: increased density on unenhanced CT
- MRI:
- T1: iso- to hypointense signal
- T2: iso- to hyperintense signal compared to gray matter
- DWI: may show altered diffusion
- postcontrast: mild, homogeneous contrast enhancement
- rapid regression of the lesions may occur with steroid treatment (“vanishing lesions”)
- meningioma is the 2nd most common primary CNS neoplasm
- lesions arising from the midline and parasagittal dural surfaces occur in ~ 10% of cases and may also involve the corpus callosum
- imaging characteristic:
- CT: increased attenuation + internal calcifications
- MRI: contrast enhancement is homogeneous; larger tumors may show foci of hemorrhage and necrosis
- metastases to the corpus callosum are rare
- the tumor more often extends into the corpus callosum from nearby structures
- imaging characteristics generally involve mass effect, vasogenic edema, and heterogeneous contrast enhancement
Neurodystrophic lesions |
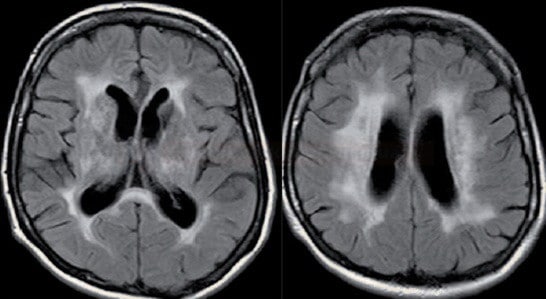
- the most common demyelinating disorder
- MR shows T2/FLAIR hyperintense lesions, with contrast enhancement in the acute stage
- subcallosal striations or callosal-septal interface lesions, which are thin bands along the undersurface of the corpus callosum, are highly sensitive and specific
- Dawson fingers are linear or ovoid lesions (hyperintense on T2/FLAIR) perpendicular to the body of the lateral ventricles that radiate along the axis of medullary veins (probably reflecting perivenular inflammation)
- in the chronic phase, T1-hypointense lesions (dark spots or black holes) reflect increased water content secondary to extreme demyelination and axonal loss
- hereditary leukoencephalopathies are congenital disorders of myelin formation or maintenance, which may affect the corpus callosum
- metachromatic leukodystrophy is the most common form
- caused by arylsulfatase A deficiency
- diffuse symmetric demyelination (hyperintense on T2/FLAIR + global atrophy
- adrenoleukodystrophy
- a peroxisomal disorder with acyl-CoA synthetase deficiency, which causes cerebral and adrenal cortical dysfunction
- demyelination typically progresses from the parietooccipital to frontotemporal lobes and involves the corpus callosum from posterior to anterior
- affected regions are hyperintense on T2 and hypointense on T1 images
- other hereditary leukoencephalopathies include Alexander disease, Krabbe disease, and Sudanophilic leukodystrophy.
- Progressive Multifocal Leukoencephalopathy (PML) is a rare demyelinating disease caused by the replication of the JC virus in immunocompromised patients
- the infection leads to the destruction of subcortical white matter (involving corpus callosum in ~ 10–15%)
- lesions are typically multifocal and asymmetric, with progressive enlargement and confluence over time
- T1 hypointense, T2 hyperintense
- absent or minimal peripheral contrast enhancement (the patient is unable to mount an adequate inflammatory response)
- Wallerian degeneration is a process of antegrade nerve fiber degeneration that occurs distal to the site of axonal injury
- it involves the breakdown of the axon and myelin sheath, followed by macrophage-mediated cleanup and eventual nerve regeneration or scarring
- bilateral cerebral infarction can produce atrophy of the intervening corpus callosum due to Wallerian degeneration of the commissural fibers
- DWI sequences are sensitive and can be used for early detection and quantification of callosal degeneration
Trauma and exposures |
- the posterior body and splenium are preferentially involved in TBI because of their fixation to the overlying dura, with resulting torque injury
- CT may show hyperdense petechial foci of hemorrhage
- MRI is more sensitive for detection of microhemorrhages (on GRE/SWI) and subtle lesions detectable on DWI
- chronic lesions are associated with hemosiderin deposits and encephalomalacia
- diffusion-tensor imaging (DTI) with tractography promises a detailed assessment of brain abnormalities in patients with TBI (Hulkower, 2013)
- primary necrosis and demyelination of the entire corpus callosum, most commonly caused by chronic alcoholism and associated malnutrition, particularly deficiencies in B vitamins such as thiamine (Vitamin B1)
- it presents with a range of symptoms, including cognitive impairment, dysarthria, and motor dysfunction
- the clinical course may be acute and fulminant (affecting the genu and splenium) or subacute-chronic (involving the body)
- diagnosis is confirmed via MRI
- initially, affected areas are edematous (T2 FLAIR hyperintensity, T1 hypointensity, reduced diffusivity, and variable contrast enhancement)
- in the chronic stages, affected regions become necrotic and atrophic, with minimal contrast enhancement
- associated hemorrhage (visible on GRE/SWI) may occur
- treatment: thiamine supplementation and alcohol cessation with a variable recovery
- hypoxic-ischemic encephalopathy is a pattern of brain injury resulting from partial oxygen deprivation due to hypoxic, hypoxemic, or ischemic causes
- lesions appear hypodense on CT and T1-hypointense and T2-hyperintense on MRI (edema and encephalomalacia)
- the corpus callosum is affected in severe and advanced cases
- in patients with chronic hydrocephalus, placement of a new ventriculostomy catheter may yield T1-hypointense and T2-hyperintense MR signal abnormalities in the corpus callosum
- the mechanism is incompletely understood and may involve biomechanical compression, edema, ischemia, demyelination, or a combination
Congenital |
- the corpus callosum develops between the 8th and 20th weeks of gestation, primarily from anterior to posterior, with the genu forming first, followed by the anterior body, posterior body, and splenium; the rostrum forms at 18–20 weeks
- embryonic insults at different stages of development result in varying degrees of callosal dysgenesis
- on the midline, sagittal T1-weighted MRI, a radiating sunburst gyral pattern may be seen because of non-convergence of the major fissures
- absence of the splenium is associated with posterior cerebral hypoplasia and ventricular colpocephaly
- complete agenesis produces parallel lateral ventricles and white matter tracts known”as “Probst bun”les”; the third ventricle may form an interhemispheric arachnoid cyst at the level of the absent corpus callosum
- intracranial lipomas are rare lesions associated with persistence and maldifferentiation of the meninx primitiva, which is the embryonic precursor of the meninges.
- tubulonodular lipomas have a round or cylindrical shape, are larger in diameter, and are usually located in the anterior brain
- curvilinear lipomas are thin lesions that curve posteriorly around the splenium. Associated callosal malformations are rarer and less severe
- imaging:
- CT – homogeneous and well-circumscribed lesion with fat density (less than −30 HU) and occasional rim calcification.
- MRI – homogeneous, T1 hyperintense and T2 hyperintense lesions, without appreciable contrast enhancement; loss of signal on fat-suppressed or STIR images confirms the diagnosis
Infection, inflammation, metabolic, drug-induced lesions |
- transient signal changes in splenium have been reported in a variety of conditions
- seizures
- antiseizure medication toxicity
- antiseizure medication withdrawal
- viral encephalitis
- bacterial and parasitic meningitis
- hypoglycemia
- hypernatremia
- uremic decompensation
- osmotic myelinolysis
- Wernicke encephalopathy
- hemolytic-uremic syndrome
- lesions are well-circumscribed and located in the central splenium
- T2 and FLAIR – hyperintense
- DWI hyperintense, ADC hypointense
- T1 – hypointense
- in the acute phase, contrast enhancement and reduced diffusivity may be seen
- after disease recovery or withdrawal of the offending agent, abnormalities resolve over weeks to months
- etiology is not fully understood; reversible demyelination and intracellular edema secondary to infectious, inflammatory, or metabolic disturbances are probable