GENERAL NEUROLOGY
Topical evaluation and etiology of consciousness disorders
David Goldemund M.D.
Updated on 07/03/2024, published on 27/11/2023
 Introduction
Introduction
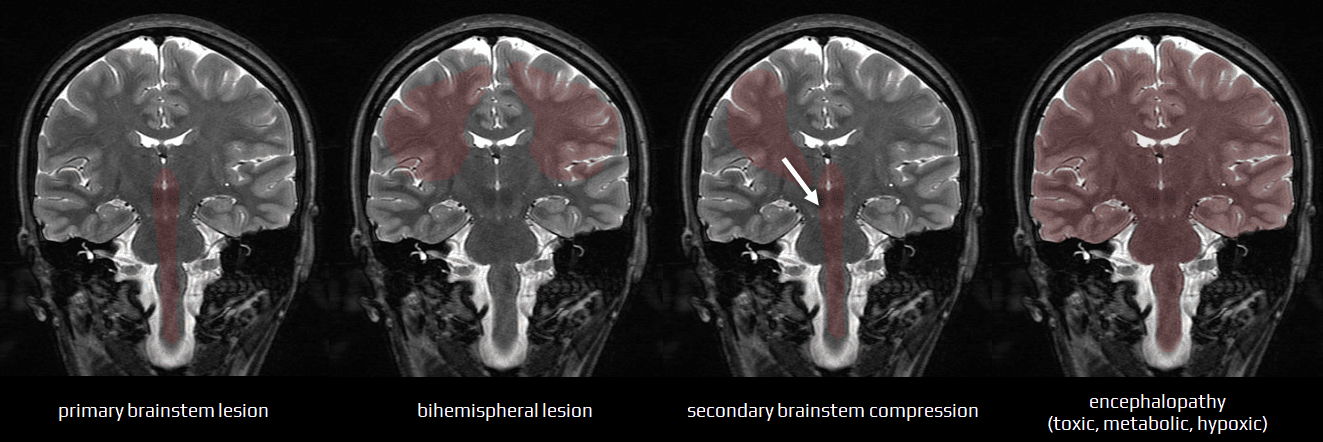
Impaired consciousness can be caused by:
- infratentorial lesions (direct brainstem lesion or external compression)
- dysfunction of brainstem reticular formation (RF) and other structures (cranial nerve centers, ascending and descending tracts, and autonomic centers)
- the combination of symptoms and signs can help localize the lesion and determine the extent of damage.
- small, localized lesions cause well-described brainstem syndromes (Wallenberg, Dejerine. etc.)
- these syndromes are typically of vascular origin corresponding to specific arterial territories, though they may also result from tumors or inflammatory processes
- these syndromes are typically of vascular origin corresponding to specific arterial territories, though they may also result from tumors or inflammatory processes
- extensive lesions, like hematomas, usually cause coma and extensive neurological impairment, preventing precise localization of the lesion
- bilateral supratentorial lesions ± secondary brainstem compression
- unilateral supratentorial space-occupying lesion with secondary brainstem compression
- compression leads to brainstem dysfunction, which progresses in a caudal direction (→ rostrocaudal deterioration)
- compression leads to brainstem dysfunction, which progresses in a caudal direction (→ rostrocaudal deterioration)
- diffuse encephalopathy
- toxic, metabolic, or hypoxic encephalopathies interfere with metabolic processes in the cerebral cortex and brainstem
- initial changes may be functional (functional transection) but may become irreversible due to complications such as edema, hemorrhage, or ischemia
The initial neurological examination in comatose patients focuses on determining the pathophysiological cause of the coma and localizing the functional impairment (encephalopathy, primary cortical or brainstem lesion, and its level). Serial neurological examinations refine the topical assessment and evaluate the evolution or regression of the lesions (following the course of the rostrocaudal deterioration syndrome).
 Brain herniation
Brain herniation
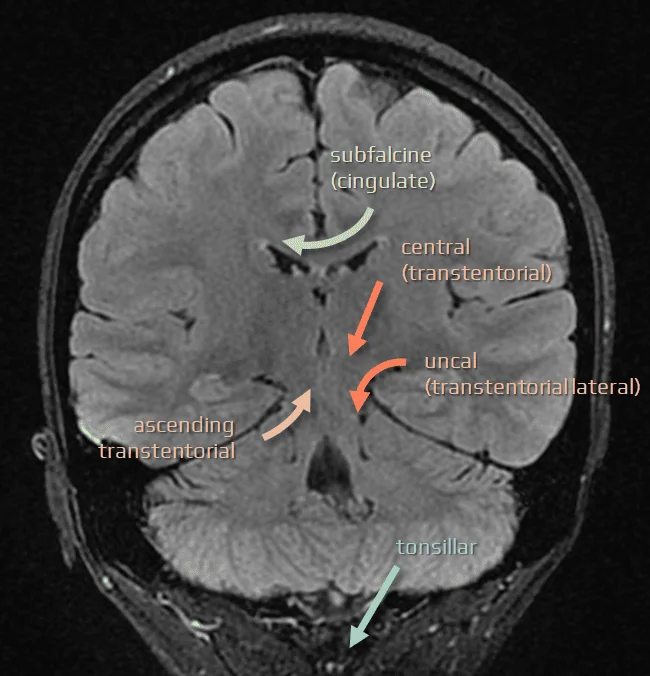
- brain herniation refers to the displacement of brain tissue, cerebrospinal fluid, and blood vessels, typically caused by a space-occupying lesion with decompensated intracranial hypertension (due to traumatic brain injury, stroke, tumor, inflammation, diffuse post-hypoxic edema, etc.)
- herniation can lead to serious and life-threatening compression of vital brain structures and disrupted blood flow (causing secondary damage)
- prompt medical intervention is crucial to manage intracranial pressure and address the underlying cause
- herniation is diagnosed by:
- characteristic physical exam findings
- brain imaging (usually cranial CT scan in the the emergent setting)
Supratentorial space-occupying lesions
- caused by lesions located above the tentorium cerebelli
- focal, such as tumor (benign or malignant), ischemia, hematoma, or abscess
- diffuse, such as post-hypoxic edema
- they lead to increased intracranial pressure and compression of adjacent brain structures
- clinical manifestations depend on the lesion’s size, growth rate, and location
- management typically involves neuroimaging for diagnosis, followed by appropriate surgical or medical interventions
In supratentorial large mass lesions, coma is caused by three main mechanisms:
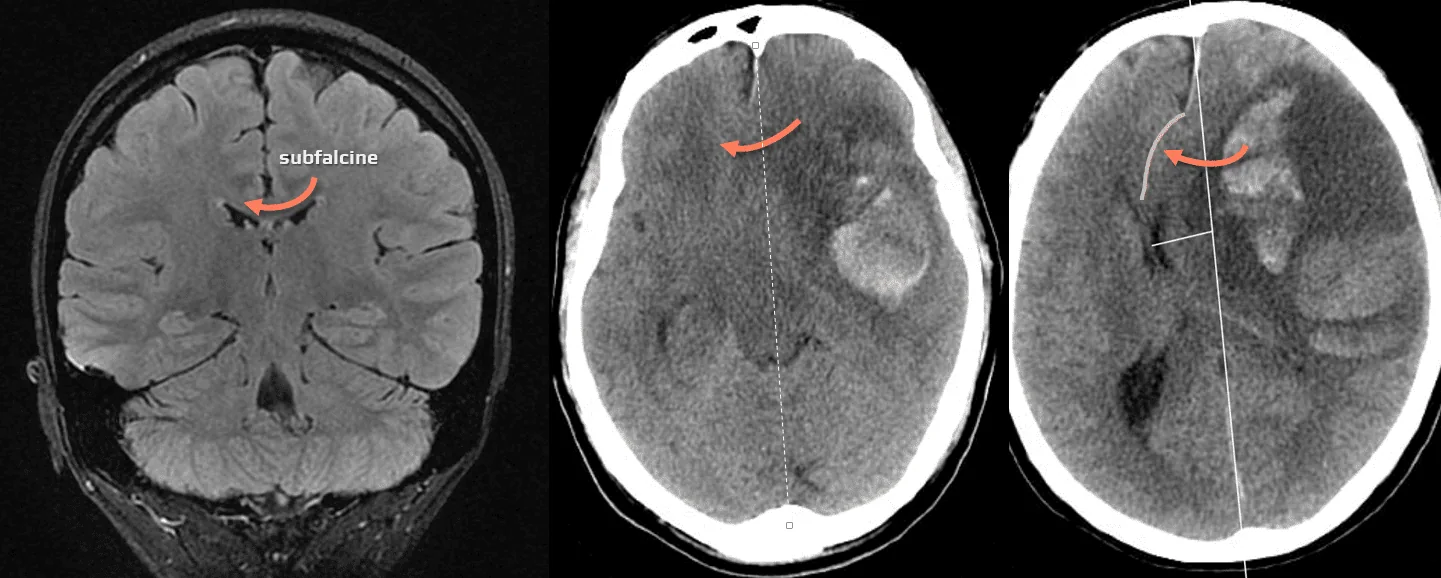
- horizontal and horizontal-rotational hemispheral shift
- descending lateral transtentorial herniation
- descending central transtentorial herniation
All three mechanisms affect the brainstem and diencephalic reticular formation and its connections to the cerebral cortex.
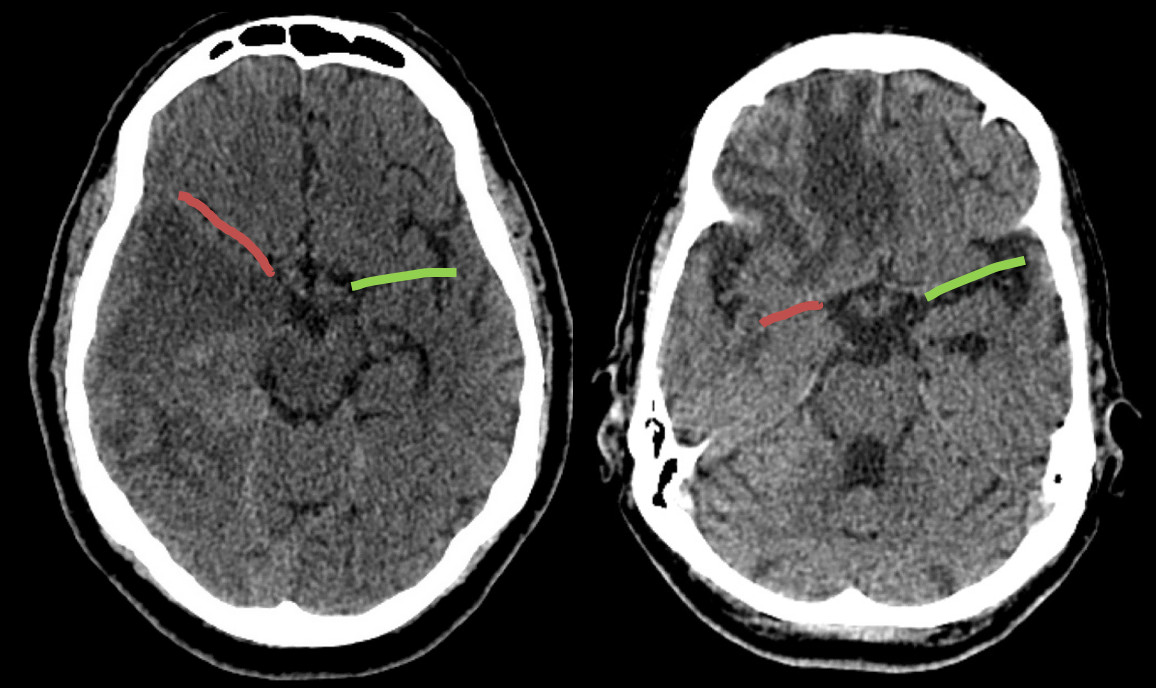
Horizontal-rotational shifts
- horizontal-rotational shift of the hemisphere and parallel shift of the midbrain compresses the meso-diencephalic reticular formation as well as the ascending reticulo-cortical pathways
- sopor, semicoma, or coma are caused by functional transection at the level of the diencephalon, diencephalic-mesencephalic junction, or mesencephalon
- progression of the lesion (due to edema, secondary hemorrhage) leads to caudal extension of the functional (later structural) transection (rostrocaudal deterioration)
- at a certain stage, the horizontal-rotational shift of the hemisphere may be accompanied by uncal, hippocampal, or central herniation, especially in the case of temporal and temporoparietal lesions
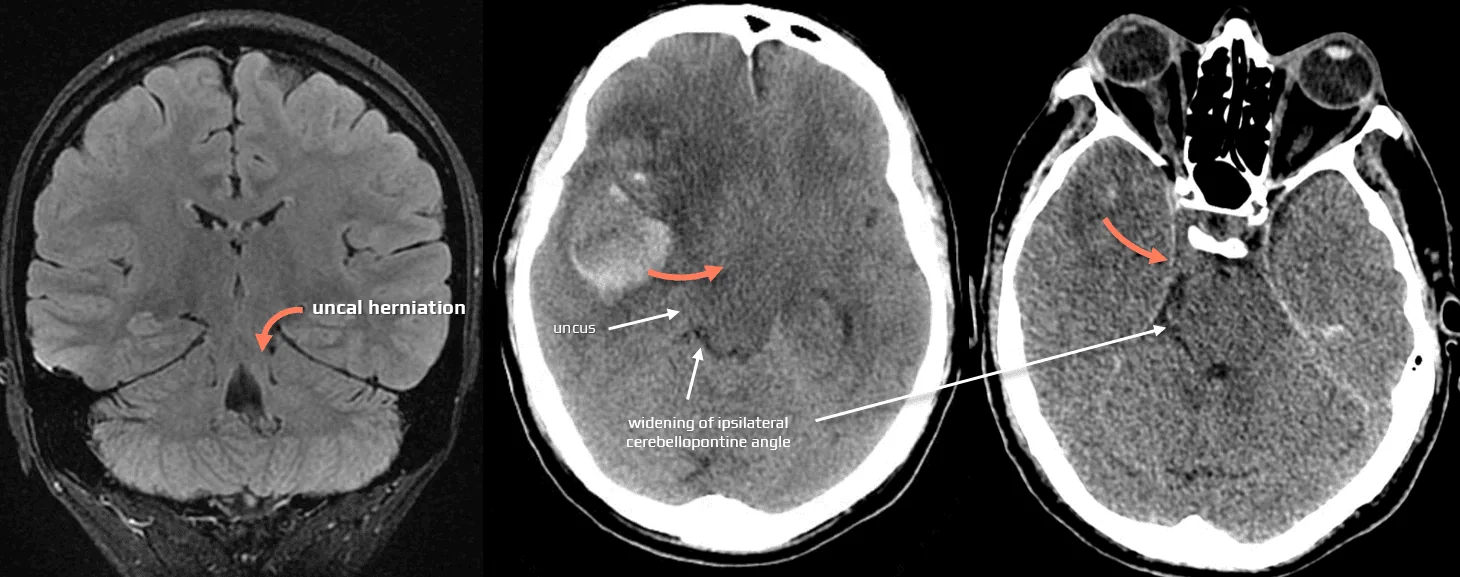
Descending lateral transtentorial herniation
- uncal herniation usually follows a horizontal-rotational shift of the hemisphere
- can be divided into three types:
- anterior (uncal) – the uncus herniates into the homolateral peduncular cistern
- posterior (hippocampal) – the parahippocampal gyrus herniate into the ambient quadrigeminal cistern
- complete (anterior and posterior) – there is only a shift and compression of the brainstem, as the rotational effects of the anterior and posterior herniation cancel each other out
| CT signs of uncal and hippocampal tentorial herniation |
|
- uncal and hippocampal tentorial herniation typically presents with:
- initially headache, nausea, and vomiting
- homolateral mydriasis and ptosis (Hutchinson’s pupil), followed by complete paralysis of the CN III due to its compression (superficially positioned parasympathetic fibers are impaired first)
- can be the first symptom to appear without severe impairment in the level of consciousness or contralateral hemiparesis
- contralateral hemiparesis (ipsilateral in ~ 25% of cases due to Kernohan phenomenon as discussed above)
- consciousness disturbances ranging from drowsiness to coma
- Cushing’s triad (hypertension, bradycardia, and irregular respiration or apnea) in advanced stages
- these symptoms are due to compression or displacement of ascending arousal pathways, the oculomotor nerve (CN III), and the corticospinal tract
- if untreated, uncal herniation progresses to central herniation
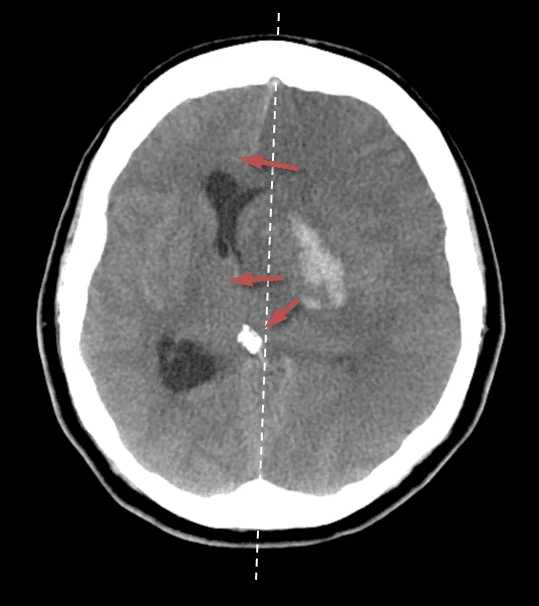
Descending central transtentorial herniation
- pressure from one or both expanding hemispheres leads to bilateral compression and caudal displacement of the thalamus and brainstem
- central transtentorial herniation is typically seen in acute lesions located near the midline and leads to transection at the diencephalic-mesencephalic level
- semicoma or coma, absent ciliospinal, frontoorbicular, and vertical oculocephalic reflexes, downward deviation of the eyes, and Cheyne-Stokes respiration may occur
- semicoma or coma, absent ciliospinal, frontoorbicular, and vertical oculocephalic reflexes, downward deviation of the eyes, and Cheyne-Stokes respiration may occur
- the central syndrome may progress craniocaudally, involving the mesencephalic, pontine, or medullary levels
Infratentorial space-occupying lesions
- most common causes: traumatic brain injury, ischemic stroke, or brainstem/cerebellar hemorrhage
- clinical presentation:
- smaller lesions present with a specific set of symptoms that allow precise localization within the brainstem or cerebellum
- complete transection at a given level is more common in rostrocaudal deterioration
- plurisegmental involvement occurs in toxic and metabolic encephalopathies
- large lesions present with nonlocalizing deep coma and apnea/gasping
- infratentorial extracerebral lesions cause coma by:
- direct compression/destruction of the ponto-mesencephalic RF
- compression of the meso-diencephalic RF due to ascending transtentorial herniation of the anterior cerebellar lobe
- compression of the ponto-bulbar reticular formation due to tonsillar herniation
| Overview of the most common causes of infratentorial space-occupying lesions |
|
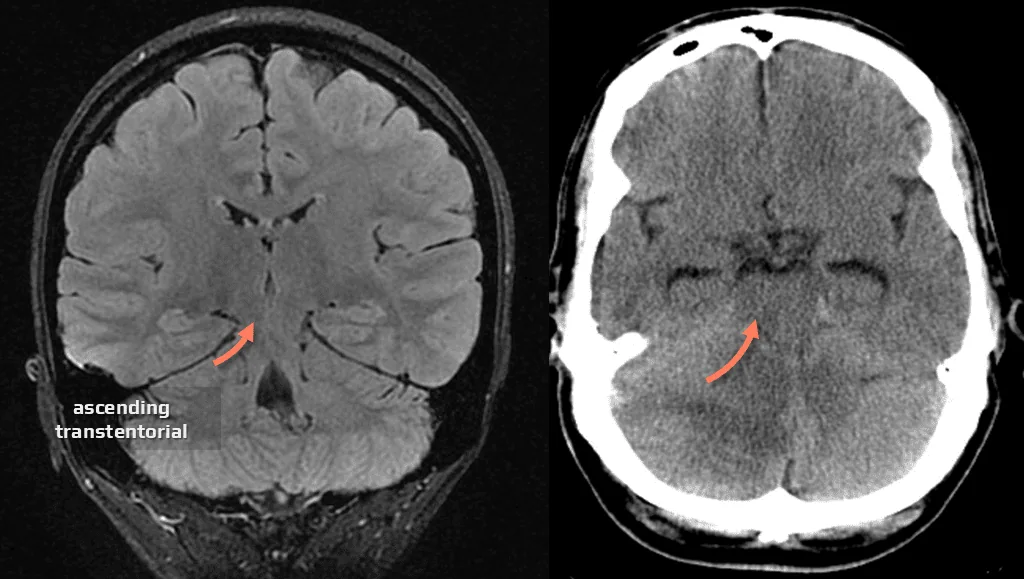
Ascending (rostral) transtentorial herniation
- herniation of the anterior cerebellar lobe is well identifiable on CT and especially on MRI
- the clinical presentation of ascending transtentorial herniation is not distinctive enough to differentiate it from the symptoms of a primary cerebellar lesion
- the typical initial symptom is gaze-evoked nystagmus
- late manifestations include:
- signs of tectal and tegmental compression (upward gaze paresis or downward gaze deviation)
- hydrocephalus due to compression of the aqueduct and perimesencephalic cisterns contributing to impaired consciousness
- progressive worsening of cerebellar syndrome results from infarction of the herniated part of the cerebellum or due to compression of the superior cerebellar arteries
- episodes of decerebrate rigidity (in advanced stages)
| CT signs of rostral transtentorial herniation |
|
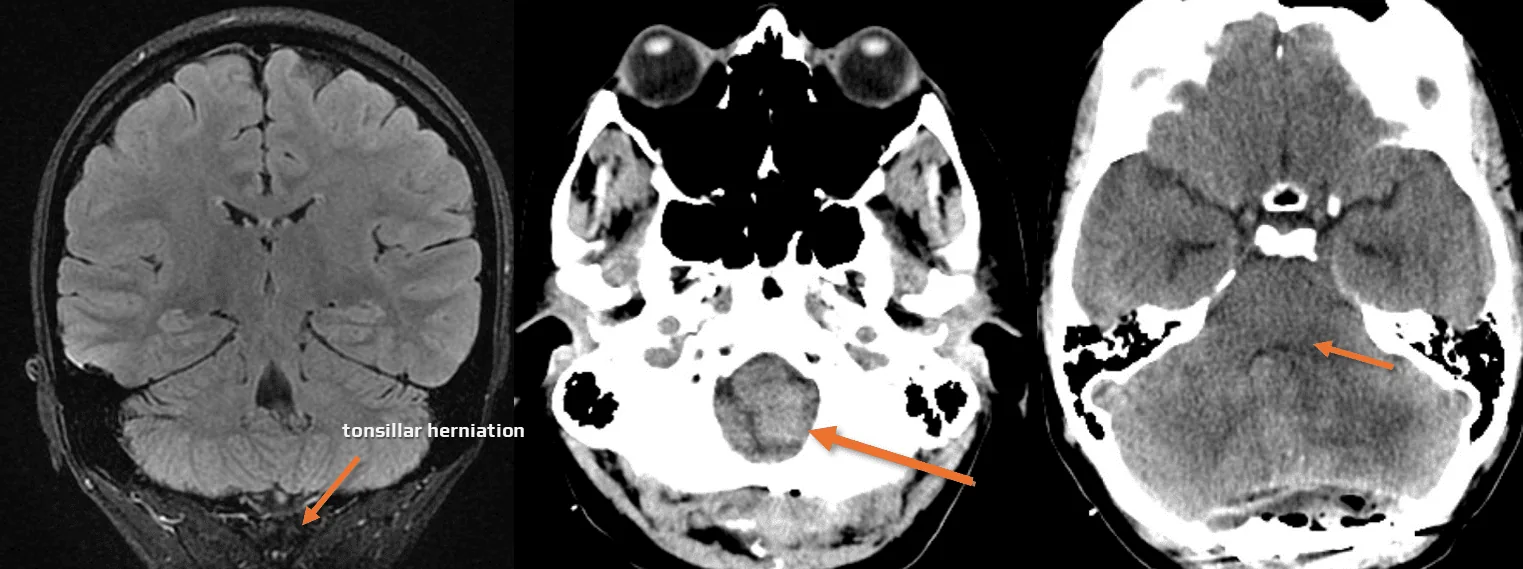
Tonsillar (caudal) herniation
- presented with respiratory disorders – ataxic and gasping breathing – followed by respiratory arrest, accompanied by failure of the bulbar vasomotor centers
- unlike tentorial herniations, impending or ongoing tonsillar herniation cannot be reliably detected by CT
Encephalopathies
- a spectrum of neurological disorders caused by systemic disturbances affecting brain function; may be reversible
- can result from a variety of etiologies, including endocrine, renal, hepatic, and electrolyte imbalances, as well as exposure to toxic substances
- clinical manifestations vary widely, ranging from mild confusion to deep coma
- diagnosis often involves a combination of clinical assessment, laboratory examinations, and imaging studies
- neurological examination can contribute to the provisional diagnosis of metabolic encephalopathy by finding certain typical symptoms or symptom complexes
- some encephalopathies may be difficult to detect
- management focuses on treating the underlying cause and supportive care for neurological symptoms
Etiology
| Overview of the most common causes of comatose multifocal and diffuse cerebral lesions, primarily toxic and metabolic encephalopathies. These metabolic lesions are characterized by the absence of unifocal or lateralizing clinical signs and negative or non-specific CT and MRI images |
|
Clinical presentation
Mental Disorders
- initial symptoms of metabolic encephalopathies include mental disorders
- ideational perseveration with altered attention is observed, followed by disorders in cognitive synthesis, followed by confusion
Respiratory Disorders
- metabolic and toxic lesions may induce respiratory disorders through two mechanisms:
- neurogenically due to functional lesions at certain brainstem levels
- metabolically through the alteration of homeostatic mechanisms
Motor Symptoms
- non-specific symptoms
- generalized or partial seizures
- positive axial reflexes
- altered muscle tone – from paratonia through decorticate syndrome to decerebrate rigidity in advanced stages of cerebral dysfunctions
- paresis – transient paresis in hepatic, uremic, hypoglycemic, and hyponatremic comas
- specific involuntary movements
- tremor and asterixis – usually in the upper limbs; may also affect the tongue, face, and lower limbs
- unilateral asterixis rarely occurs in structural contralateral midbrain, thalamic, and parietal lesions
- multifocal myoclonus – most commonly associated with uremic and hyperosmolar hyperglycemic comas
- tremor and asterixis – usually in the upper limbs; may also affect the tongue, face, and lower limbs