ISCHEMIC STROKE
Topical diagnosis of stroke
David Goldemund M.D.
Updated on 23/02/2024, published on 20/06/2023
Topical diagnosis in stroke refers to the localization of ischemia within the brain based on clinical signs and symptoms and neuroimaging. This approach helps to differentiate between different stroke subtypes, such as cortical versus subcortical strokes, or to identify specific vascular territories that may be affected (large vs. small vessel occlusion, anterior vs. posterior circulation). Accurate topical diagnosis is essential for timely and targeted intervention and can help determine the etiology of stroke and initiate appropriate secondary stroke prevention.
 Diagnostic methods
Diagnostic methods
Both clinical examination and imaging should help answer the following questions:
|
 Clinical presentation
Clinical presentation
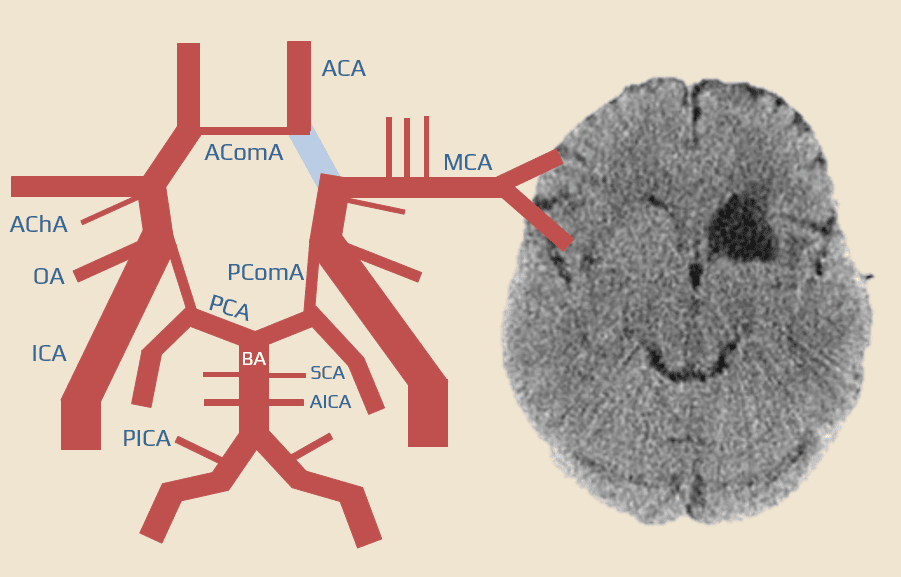
The main regions to consider are:
- anterior circulation (carotid system) involving the internal carotid artery, middle cerebral artery, and anterior cerebral artery and their branches
- posterior circulation (vertebrobasilar system) involving the vertebral arteries, basilar artery, and posterior cerebral artery
Common carotid artery (CCA) and external carotid artery (ECA) |
- the common carotid artery (CCA) is most usually affected by atherosclerosis
- extensive atherosclerosis may occur due to radiation-induced vasculopathy
- concentric wall thickening is a characteristic feature of Takayasu arteritis
- trauma/dissection (usually extending from the aortic arch) usually leads to sympathetic plexus disruption and the development of complete Horner’s syndrome
- the extent of anhidrosis varies with the level of lesion
- lesions affecting the plexus surrounding the CCA affect the entire half of the face
- lesions affecting the plexus surrounding the ICA affect only the medial part of the forehead and the lateral aspect of the nose
- in Horner syndrome, the upper eyelid never descends below the center of the pupil
- Pseudo-Horner syndrome is the coincidence of simple anisocoria (20% of the population) and measurable asymmetry in the width of the eye slits (15% of the population) with a narrower pupil and eye slit on the same side (3-4% of the population)
- the extent of anhidrosis varies with the level of lesion
- CCA occlusion/stenosis may be asymptomatic or have a clinical presentation similar to ICA occlusion/stenosis (see below)
- ECA occlusion/stenosis is typically asymptomatic
- ECA stenosis may become symptomatic if the ACE serves as the dominant collateral pathway in case of the ipsilateral ICA occlusion
- inflammatory involvement has typical clinical presentation → temporal arteritis
Internal carotid artery (ICA) |
- variable clinical presentation, from asymptomatic occlusion to severe hemispheric infarct
- presentation depends on:
- the dynamics of the occlusion (progressive stenosis x acute thrombotic occlusion)
- the location and extent of the occlusion (occlusion at the ICA origin x terminal ICA occlusion +/- proximal ACA and MCA involvement)
- collateral circulation status
- individual anatomical variations
- Border zone infarcts (BZIs) are also a specific finding in patients with ICA occlusion or severe stenosis
Ophthalmic artery (OA) |
- the ophthalmic artery supplies blood to the retina and other structures of the eye
- the symptoms of its occlusion are primarily visual; the severity can vary depending on the extent and speed of the occlusion
- usually sudden, painless monocular visual impairment (ranging from scotoma to complete amaurosis)→ see CRAO
- arteriolopathic changes lead to ischemic optic neuropathy (ION)
- nonarteritic forms of ION usually do not result in total blindness
- initially, there is edema of the optic nerve head, followed by its atrophy
- nonarteritic forms of ION usually do not result in total blindness
| Differential dg. sudden monocular blindness |
|
Anterior choroidal artery (AChA)
|
- the Anterior Choroidal Artery (AChA) originates from the supraclinoid portion of the ICA (above the PComA) or MCA
- the AChA supplies several important brain structures:
- choroid plexus in the lateral ventricles
- optic chiasm, optic tract, and lateral geniculate body
- internal capsule
- medial part of the globus pallidus
- amygdala and anterior segments of the hippocampus
- hypothalamus, substantia nigra, and nucleus ruber
- a variety of symptoms may be seen depending on the specific area of the brain that is affected; confusion with other types of strokes or neurological disorders is frequent
- contralateral homonymous visual field defects (lateral geniculate body)
- contralateral hemiparesis (internal capsule)
- contralateral hemihypesthesia (posterolateral thalamic nuclei)
- bilateral lesions may cause akinetic mutism
- memory deficit (if anterior segments of the hippocampus are involved)
- dysfunction in the hypothalamus, substantia nigra, and nucleus ruber is less common
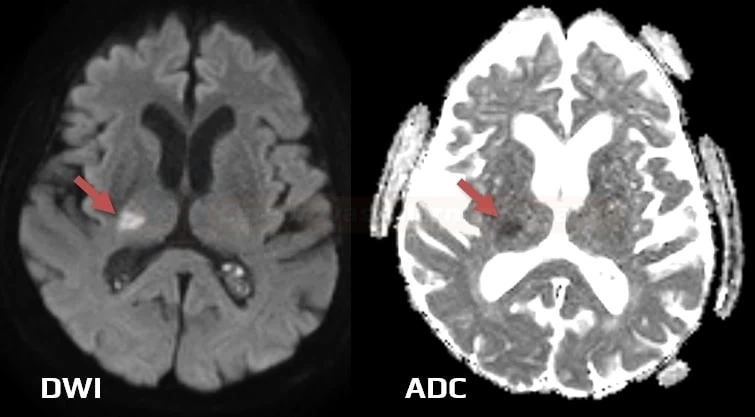
- AChA occlusion most commonly results from arteriolopathy or embolization
Anterior cerebral artery (ACA)
|
- clinical presentation can vary depending on several factors, such as the location and extent of the occlusion, the functionality of collateral circulation, such as the anterior communicating artery (AComA), and the individual’s unique anatomy.
- motor and sensory deficits:
- hemiparesis – often more pronounced in the lower extremity than the upper extremity.
- hemisensory loss – often parallel to the hemiparesis pattern
- cognitive and behavioral changes
- frontal lobe syndrome
- apathy, abulia, and reduced creativity
- emotional incontinence and social disinhibition
- dysexecutive syndrome
- symptoms of frontal syndrome become more severe in cases of bilateral involvement (e.g. when both ACAs are supplied by a single carotid artery)
- contralateral apraxia
- frontal lobe syndrome
- speech and language deficits
- transcortical motor aphasia (dominant hemisphere) – characterized by good comprehension but poor speech production
- transcortical motor aphasia (dominant hemisphere) – characterized by good comprehension but poor speech production
- other symptoms:
- Alien hand syndrome (nondominant hemisphere) – a person might experience involuntary hand movements
- eyes and head may deviate toward the side of the infarct
- some perforating branches supplying the anterior portion of the internal capsule may originate from the A1 segment. Occlusion of the ACA may result in paresis of the CN VII and arm
Alien hand syndrome
- Alien hand syndrome (AHS) is associated with lesions in the frontal, callosal, or parietal regions
- usually, the left hand functions involuntarily; the person has no control over its movements
- various etiology:
- stroke
- most often due to multiple emboli in the parietal and frontal lobes
- occlusion of the ACA could contribute to the syndrome if the infarct affects regions responsible for motor planning and execution
- occlusion of branches of the MCA could also result in motor and sensory deficits that contribute to the syndrome
- degenerative diseases
- post-callosotomy syndrome
- tumors
- infections
- stroke
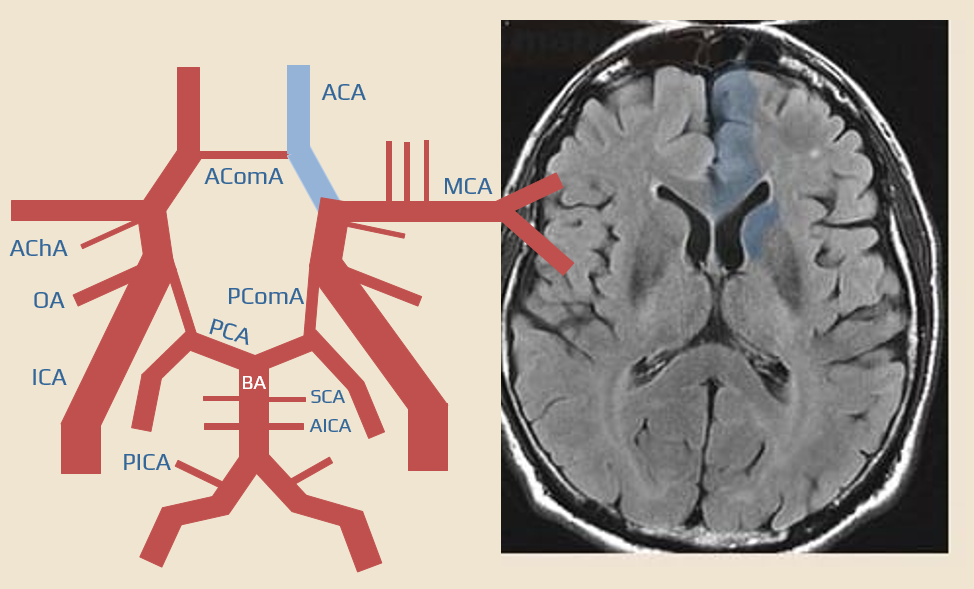
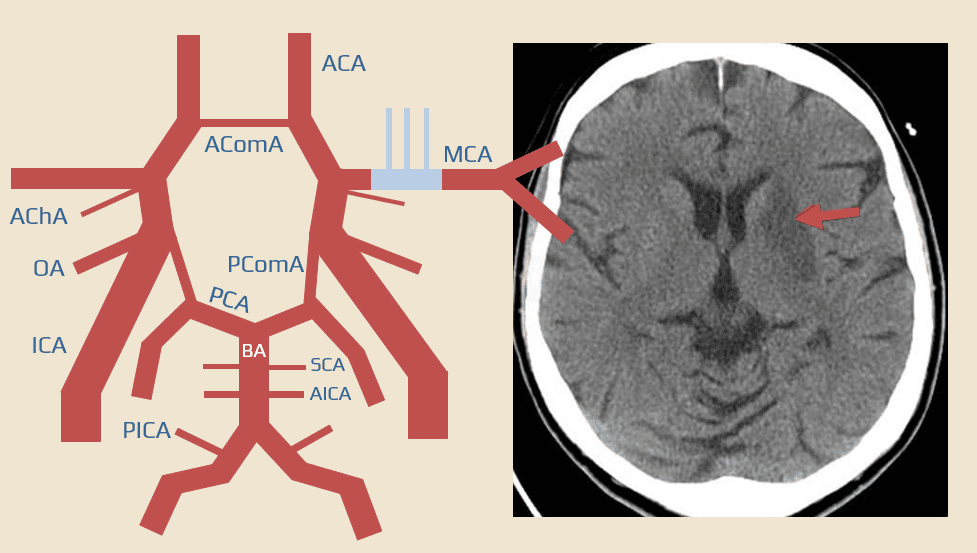
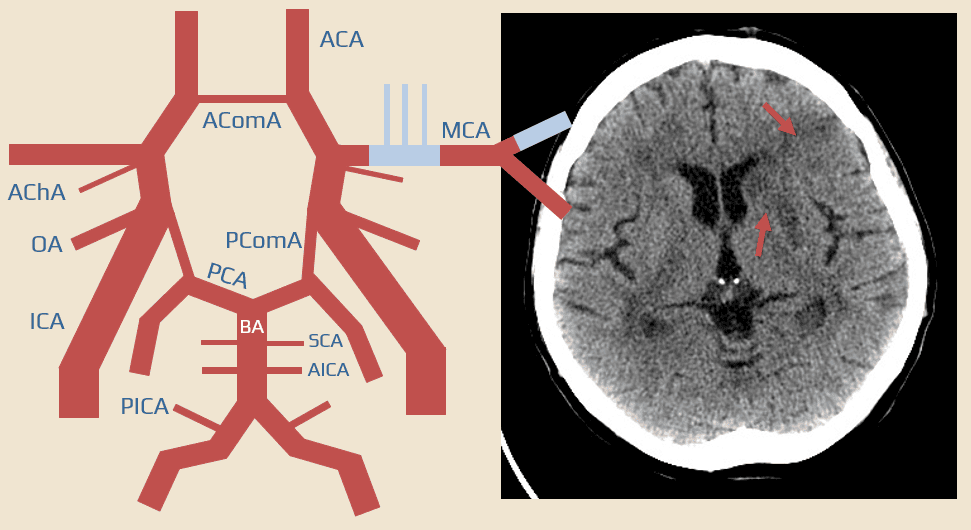
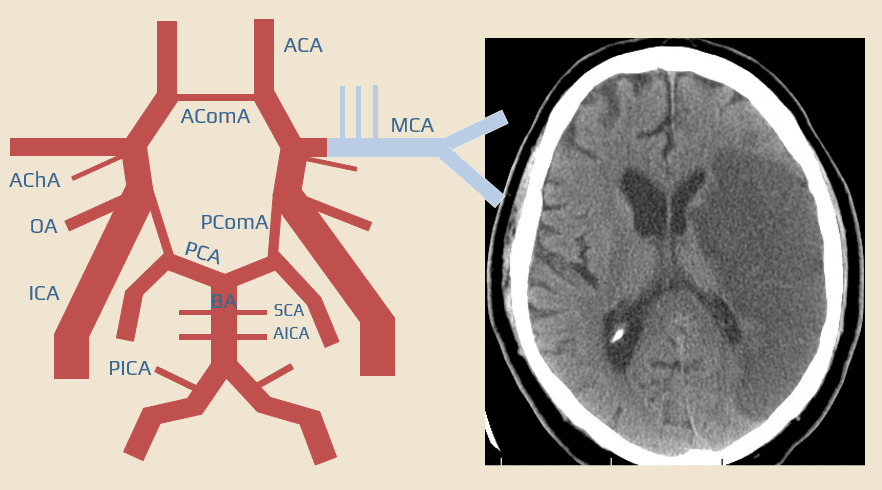
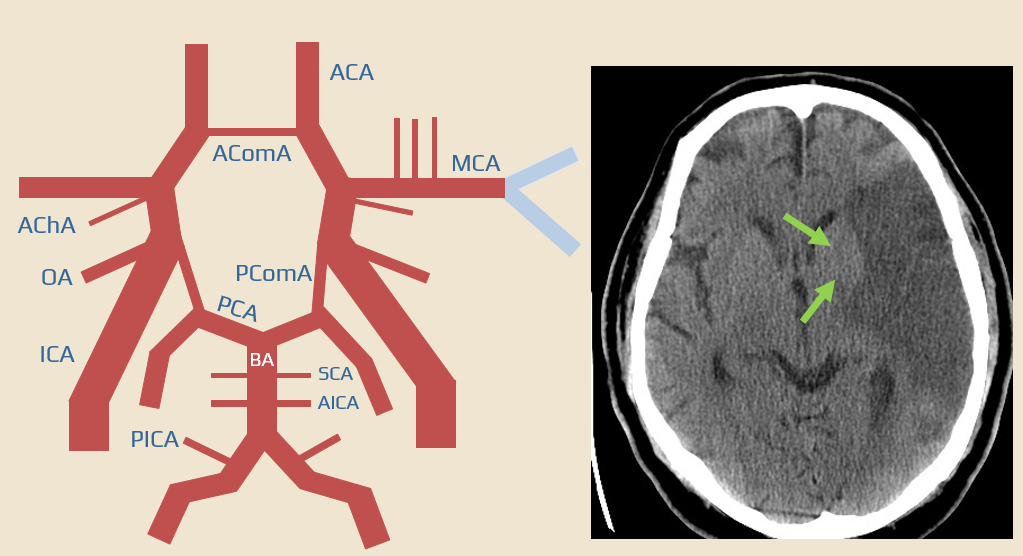
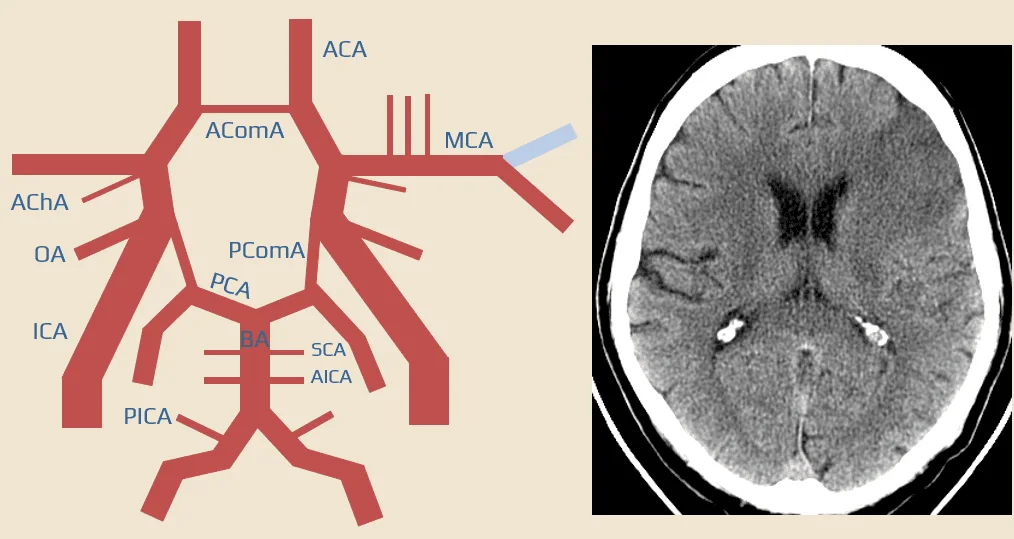
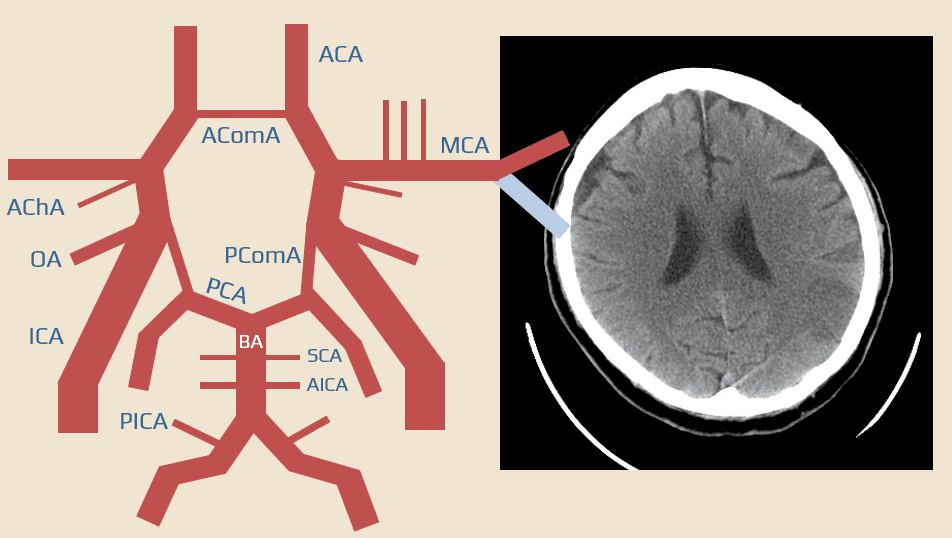
Middle cerebral artery (MCA)
|
- lenticulo-striate arteries (LSAs) branch off from the M1 (lateral LSA) and A1 (medial LSA) segments and supply part of the caudate and lentiform nucleus, the anterior and partially posterior arm of the internal capsule
- lenticulostriate arteries lack collateral circulation, which makes them more susceptible to ischemia
- occlusion of a single lenticulostriate artery results in a small deep infarct (small vessel disease – TOAST 3)
- this lesion may present with specific lacunar syndrome or may remain clinically silent and manifest over a long period. Multiple lesions cause status lacunaris (Binswanger’s disease) with pseudobulbar syndrome, cognitive impairment, and lower body parkinsonism
- enlargement (atrophy) of the perivascular Robin-Virchow spaces should be distinguished from lacunes
- this lesion may present with specific lacunar syndrome or may remain clinically silent and manifest over a long period. Multiple lesions cause status lacunaris (Binswanger’s disease) with pseudobulbar syndrome, cognitive impairment, and lower body parkinsonism
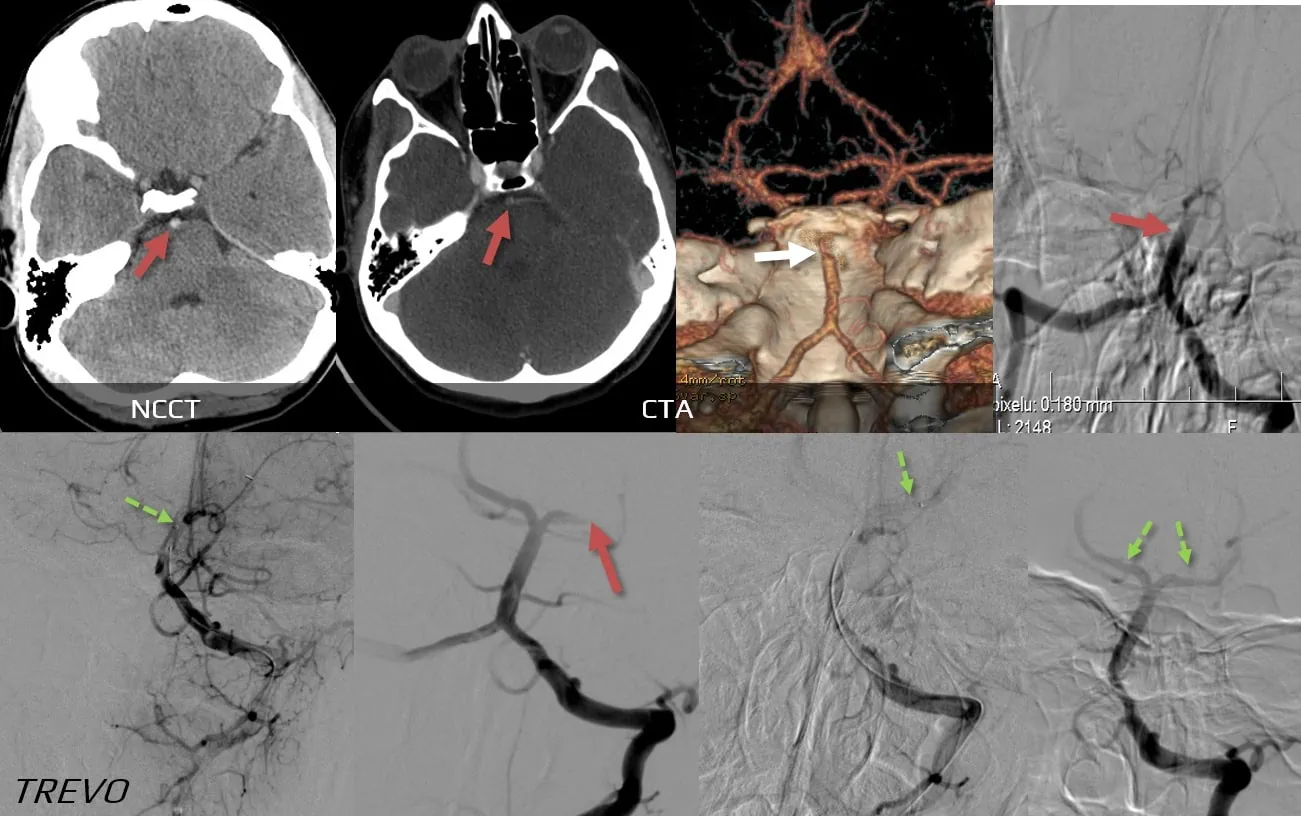
- isolated M1 occlusion with good leptomeningeal anastomoses results in infarction of the basal ganglia and internal capsule (perforators occlusion)
- multiple lenticulostriate branches are often affected, and severe contralateral deficit is common
- M1 segment occlusion may be complicated by peripheral embolization to M2-3 segments (spontaneous or due to recanalization therapy) with parenchymal infarcts
- the frontal lobe is mainly affected when the superior MCA branch is occluded
- faciobrachial hemiparesis
- gase paresis
- motor aphasia
- apraxia
Vertebral artery
|
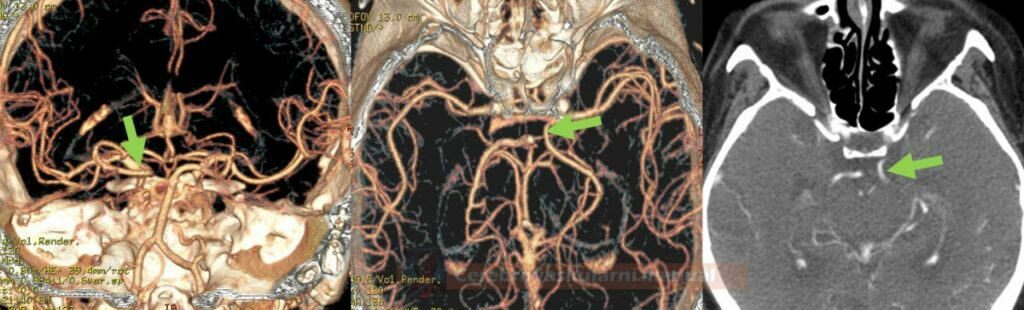
- the vertebral artery (VA) most commonly originates from the subclavian artery, passes through the costotransverse foramina of vertebrae C6 to C2, and enters the skull through the foramen magnum
- segments (V0-4):
- V0 – origin
- V1 – segment before entering the transverse foramen (this happens most commonly at the level of vertebra C6)
- V2 – intraforaminal segment
- V3 – atlas loop (C2-dura)
- V4 – intracranial segment
- major branches:
- PICA (may arise uni- or bilaterally from the basilar artery) – supplies medulla oblongata (including the vestibular nuclei) and the inferior cerebellum
- anterior and posterior spinal arteries
- atherosclerosis typically affects segments V1 and V4
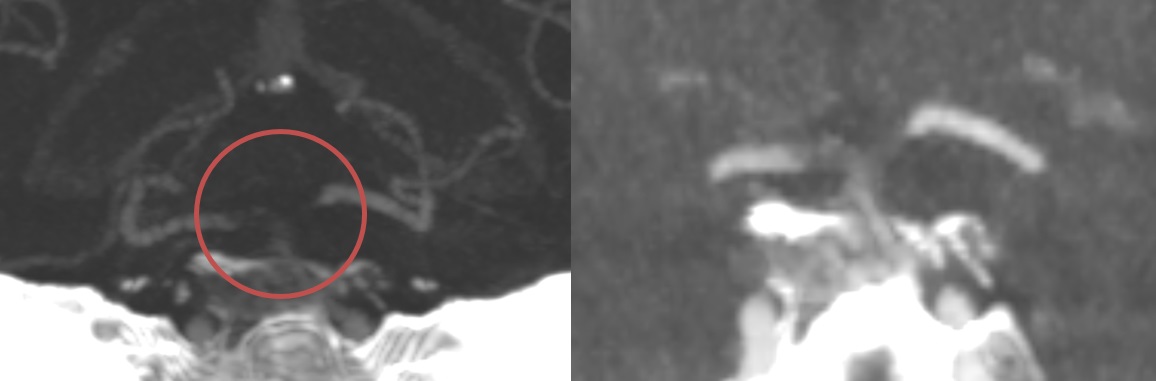
- dissection mainly affects segment V3 (although concomitant thrombosis may occlude the entire vessel)
- steal syndrome may occur in the presence of significant subclavian artery stenosis
- transient dizziness and other posterior circulation symptoms occur during physical activity involving the ipsilateral arm
- transient dizziness and other posterior circulation symptoms occur during physical activity involving the ipsilateral arm
- rarely, the VA may be compressed by head rotation (→ Bow Hunter’s syndrome)
- AV occlusion may remain asymptomatic; symptoms depend on the extent of the occlusion, the anatomic situation (is the dominant VA affected?), and whether distal embolization has occurred (to the BA or its branches)
- ischemia typically occurs in the lateral medulla oblongata (symptoms are described in the PICA section)
- extensive brainstem and cerebellar ischemia is also common
- ischemia typically occurs in the lateral medulla oblongata (symptoms are described in the PICA section)
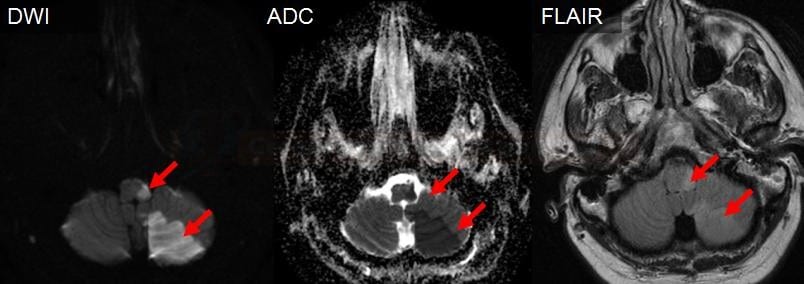
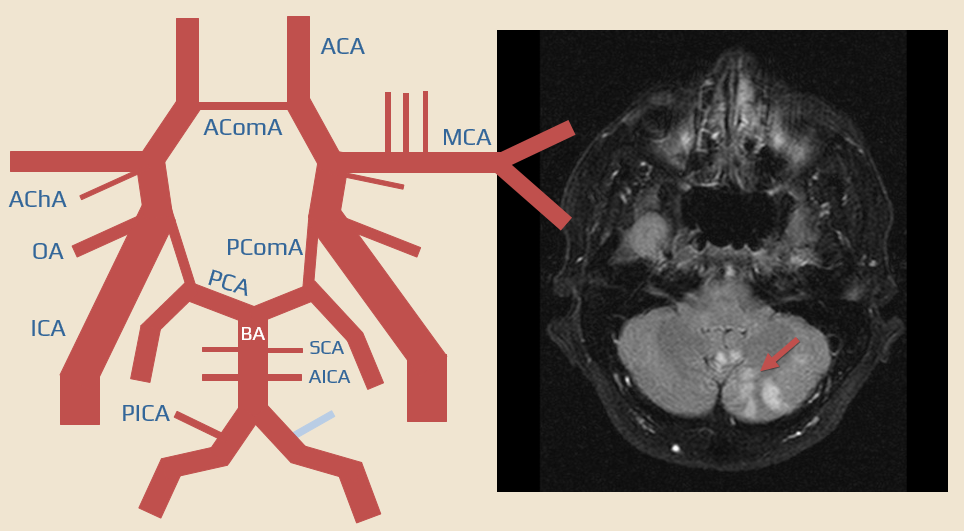
Posterior inferior cerebellar artery (PICA)
|
- etiopathogenesis:
- thromboembolism from ostial vertebral stenosis (V0 segment)
- thromboembolism from the V4 segment
- embolization from the heart and the aortic arch
- dissection (usually starting at the V3 segment; may lead to a complete VA occlusion)
- clinical presentation
- cerebellar infarct
- involves part of the vermis and hemisphere
- presenting with ataxia, vertigo, nystagmus (usually a simultaneous brainstem lesion occurs)
- lateral medullary syndrome (Wallenberg syndrome) occurs when the PICA gives off branches to the oblongata (medulla oblongata is more commonly supplied by the VA and BA)
- ipsilateral: Horner’s syndrome, facial hypesthesia for all modalities, ataxia
- contralateral: dissociated hypesthesia from the neck downward (impaired sensation of pain and temperature with preserved touch sensation)
- vestibular syndrome – vertigo, nystagmus (inferior vestibular nuclei)
- bulbar palsy (dysarthria, dysphonia, dysphagia), singultus
- nausea and vomiting
- singultus
- cerebellar infarct
.
Anterior inferior cerebellar artery (AICA)
|
- AICA arises from the lower part of the basilar artery and supplies:
- the upper part of the medulla oblongata and cerebellum
- the base of the pons
- it may give off the labyrinthine artery (also known as the auditory artery or internal auditory artery), which may also arise from the BA
- clinical presentation of isolated AICA occlusion (AICA syndrome):
- vestibular syndrome (nausea, vomiting, nystagmus, vertigo)
- ipsilateral ataxia
- sometimes contralateral hemiparesis
- occlusion of the labyrinthine artery may cause hearing loss
- ipsilateral facial weakness
- sometimes contralateral hemiparesis ( if corticospinal tracts in the pons are involved )
- vestibular syndrome (nausea, vomiting, nystagmus, vertigo)
Superior cerebellar artery (SCA)
|
- SCA arises from the rostral portion of the basilar artery, just below the PCA, and supplies:
- the superior cerebellar peduncle
- vermis
- the upper part of the cerebellar hemisphere
- the dorsolateral portion of the mesencephalon (midbrain)
- dentate nucleus
- clinical presentation
- neocerebellar syndrome with ataxia and tremor
- dysarthria
- Horner’s syndrome
- central paresis of the CN VII
- ipsilateral choreiform movements
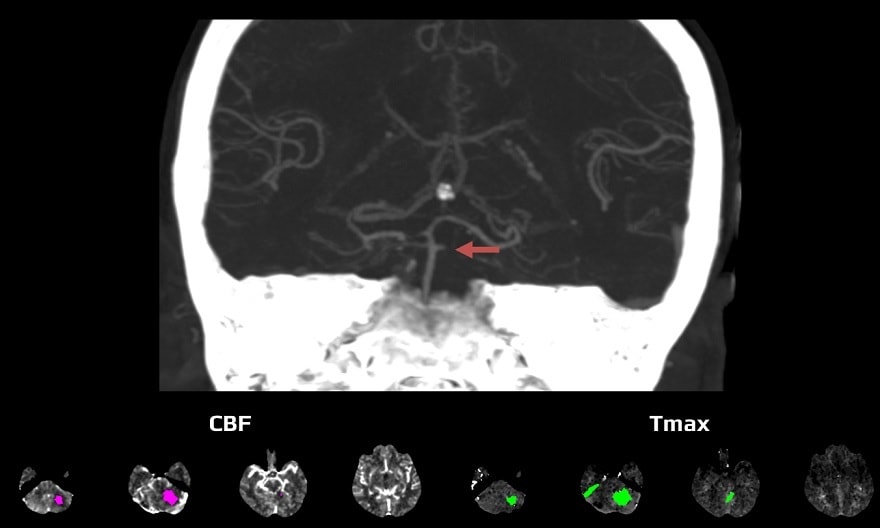
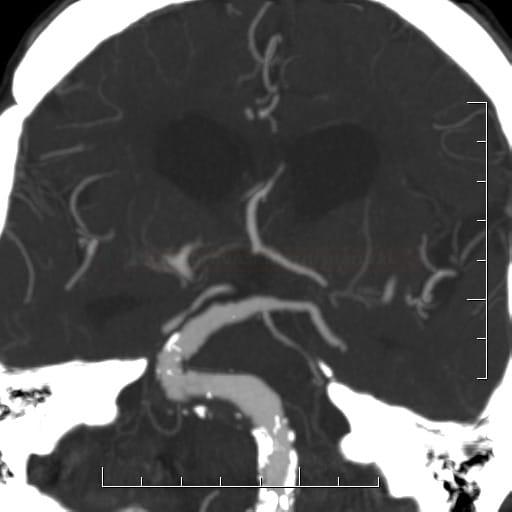
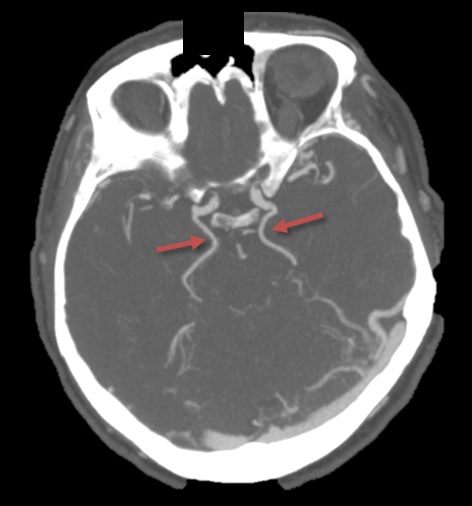
Basilar artery (BA)
|
- the basilar artery is a major blood vessel at the base of the brain that arises from the confluence of the two vertebral arteries, runs along the ventral surface of the brainstem, and gives off several branches before it branches into the two posterior cerebral arteries (PCAs)
- it supplies blood to the posterior part of the brain, including the cerebellum, brainstem, and occipital lobes
- pons ((and sometimes medulla oblongata) are supplied via perforating and circumferential branches
- occlusion of the BA or its branches (embolic, atherothrombotic) results in a mix of symptoms caused by lesions in the brainstem, cerebellum, thalamus, temporal and occipital lobes (basilar artery syndrome)
- perforators are commonly divided into:
- paramedian perforators (arise directly from the basilar artery and supply medial aspects of the pons)
- short circumferential perforators (supply lateral aspects of the pons, typically arise closer to the origin of the basilar artery)
- long circumferential perforators (superolateral group, often arise near the bifurcation of the basilar artery into the posterior cerebral arteries; they supply lateral and dorsal parts of the pons and upper parts of the medulla)
- classification of localized infarcts:
- medulla oblongata infarcts: medial, lateral, and dorsolateral
- pontine infarcts: anteromedial, anterolateral, and dorsolateral
- midbrain infarcts: medial, lateral, and dorsal
→ see brainstem syndromes
- dorsolateral and paramedian infarcts are more likely to be caused by the atherosclerosis of the circumferential and perforating arteries (branch artery disease – BAD) or embolization
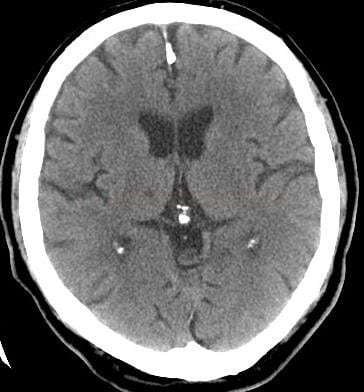
- brainstem lacunar infarcts are caused by arteriolopathy (small vessel disease)
(Kataoka, 1997)
- variable presentations – from asymptomatic occlusions to catastrophic large posterior circulation strokes with initial coma
- brainstem symptoms may include bilateral paresis, cranial nerve palsy, and progressive impairment of consciousness
- impaired consciousness may sometimes be the initial symptom (due to missing collaterals)
- locked-in syndrome is characterized by complete paralysis of voluntary muscles (tetraplegia with bilateral cranial nerve involvement, except for those controlling vertical eye movement)
- individuals with locked-in syndrome are often completely conscious and cognitively intact
- horizontal gaze is paralyzed, while the rostral segment controlling the vertical gaze remains intact
- patient can communicate by looking up and down and blinking
- modern technology has provided alternative communication methods for people with this condition, using eye movements to control computers
- the mesencephalon and occipital lobes can be spared if there is good collateral supply from the anterior circulation via the PComA.
- a short BA occlusion with good collateral circulation may be oligo- or asymptomatic
- distinguish occlusion from hypoplasia
- top of the basilar syndrome is caused by embolization rather than atherothrombosis
- affected regions include the mesencephalon (midbrain), thalamus, hypothalamus, medial temporal, and occipital lobes
- the most typical symptoms are :
- oculomotor palsy (CN III lesion with marked mydriasis and ptosis)
- vertical gaze palsy
- ataxia
- hypersomnia
- cognitive and memory impairment
- visual disturbances (from blurred vision to cortical blindness
- dysarthria
- sensory and motor deficits (depending on the areas affected)
- a progressive disease characterized by dilation and tortuosity of the arteries; it is sometimes called dilated arteriopathy
- mostly asymptomatic
- symptomatic forms present with focal signs and symptoms due to:
- brainstem compression
- partial thrombosis leading to the occlusion of perforator ostia or distal embolization
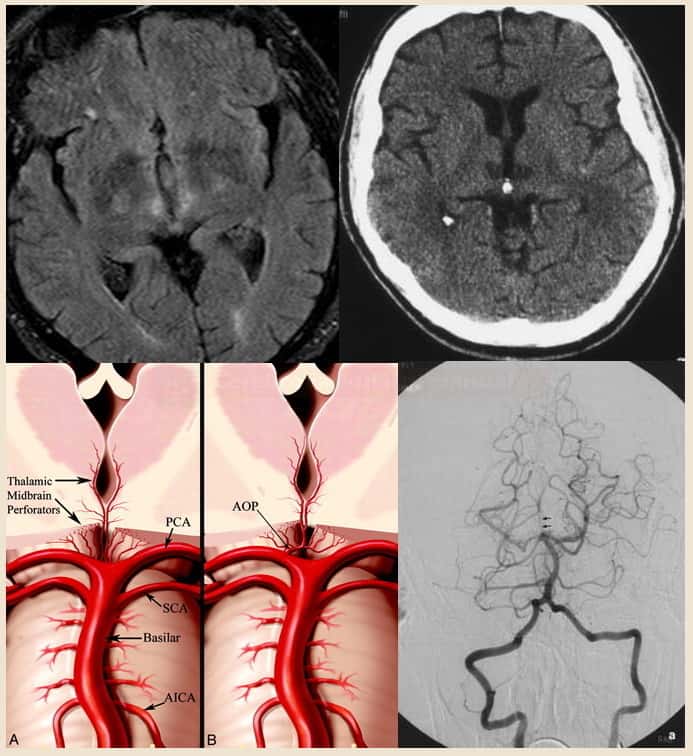
Posterior cerebral artery |
- the posterior cerebral artery (PCA) is a terminal branch of the basilar artery
- the proximal segment gives off branches to the middle part of the mesencephalon, a substantial portion of the thalamus, and the lateral geniculate body
- these branches may arise from a single PCA and supply both sides ⇒ extensive mesencephalic infarction may be thus present in unilateral PCA occlusion
- occlusion of the pre-communicating segment (P1) leads to infarction of the cerebral peduncles, thalamus, and mediobasal parts of the temporal and occipital lobes.
- peduncles and thalamus are spared when only the P2 segment (posterior to the PComA) is occluded
- symptoms resemble those of the MCA occlusion
- homonymous hemianopsia
- hemiparesis/hemihypesthesia (with concomitant mesencephalic/thalamic ischemia)
- color vision disturbance, palinopsia, alexia, agraphia
- in the context of mesencephalic involvement, there may be upward gaze palsy, CN III lesion, disturbances of consciousness, and mnestic disturbances (if the medial part of the temporal lobes is supplied from the PCA)
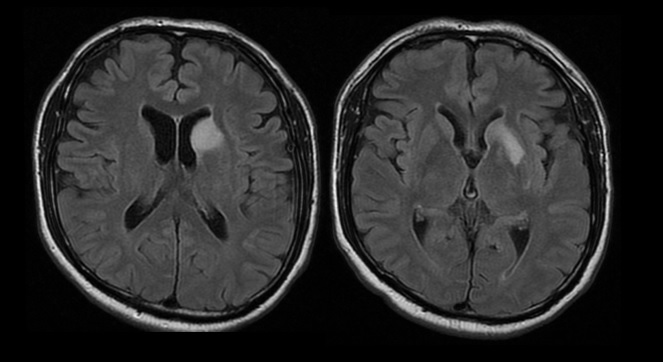
- acute confusion, apathy, memory impairment, and upward gaze paresis without significant motor or sensory deficits (if only thalamic PCA branches are affected)
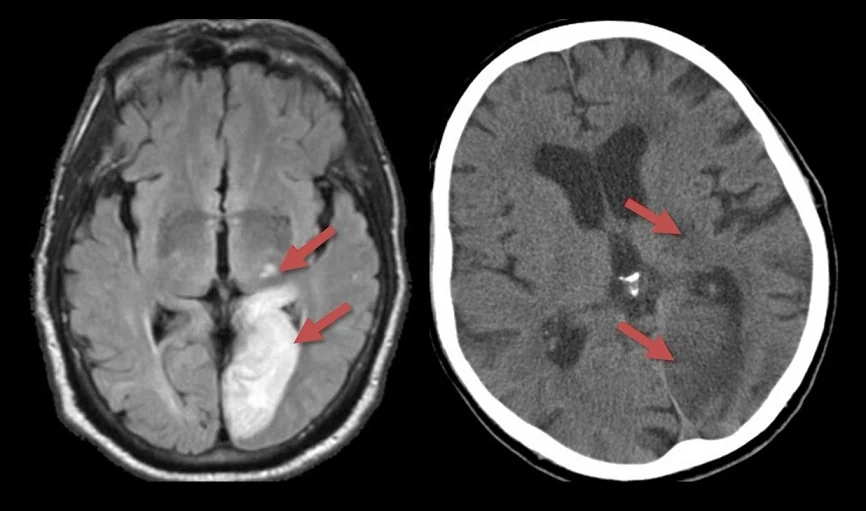
- occlusion of thalamic branches arising from a single PCA(Percheron’s artery) or both PCAs causes quantitative and qualitative impairment of consciousness; may lead to akinetic mutism or thalamic dementia
- perforators arising from the PCA:
- anterior thalamoperforating artery (from PComA)
- posterior thalamoperforating arteries (from P1 segment)
- thalamogeniculate arteries (distal P2 segment)
- posterior choroidal arteries (from P2 segment)
- occlusion of these branches results in a so-called pure sensory stroke with complete hemianesthesia; smaller lesions may cause impaired sensation only for some qualities or only in one limb or even have a pseudoradicular distribution
- ischemia may also affect part of the internal capsule, resulting in sensorimotor stroke
- ischemia affecting the ventrolateral thalamic nucleus leads to secondary hemiataxia due to interruption of the dentatorubrothalamic tract, and the clinical presentation resembles cerebellar ischemia
- occlusion of the more distal thalamogeniculate arteries may cause Déjerine-Roussy syndrome with hemiataxia, hemianesthesia, astereognosia, and hyperkinesia in otherwise mild hemiparesis. Thalamic pain often develops
- occlusion of posterior choroidal arteries causes visual field deficits or mnestic disorders
- most commonly upper or lower homonymous quadrantopsia
- sometimes, memory impairment or transcortical aphasia
- during fetal development, the PCA originates from the ICA; if this arrangement persists, it is referred to as a “fetal-type PCA”
- unilateral x bilateral
- classification:
- complete fetal type – P1 segment is absent or not visible on imaging
- partial fetal type – P1 segment is hypoplastic and smaller than PComA
- prevalence ~10-26%
- clinical implications:
- the ICA occlusion can lead to combined MCA+PCA infarction (the ACA is mostly supplied by the contralateral ACA via the AComA)
- the ICA stenosis may lead to isolated embolism in the PComA
- homonymous hemianopsia (loss of half of the vertical visual field)
- neuropsychological deficits
- dominant hemisphere – “alexia without agraphia”, Gerstmann syndrome (right-left disorder, finger agnosia, constructional apraxia, agraphia, and acalculia), transcortical sensory aphasia, anomia or anosognosia for colors
- nondominant hemisphere – spatial perception disorder, neglect syndrome, prosopagnosia
- memory impairment with mediobasal temporal lobe involvement
- bilateral altitudinal hemianopsia
- cortical blindness (blindness with preserved pupillary reactivity)
- Anton-Babinski syndrome → more here
- cortical blindness actively denied by the patient through confabulations (anosognosia of blindness)
- bilateral occipital lesions involving association areas
- impaired color vision
- severe memory impairment (thalamic dementia) when both thalami are affected
- severe memory impairment has also been described in unilateral lesions
- a common variant is that one or both PCAs are supplied exclusively by the posterior communicating artery (PComA) – thus, no visual field loss occurs with occlusion of the superior segment of the basilar artery
Other localized ischemia |
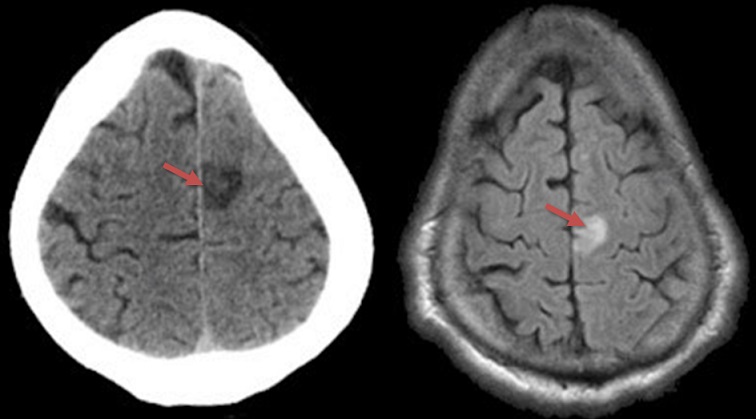
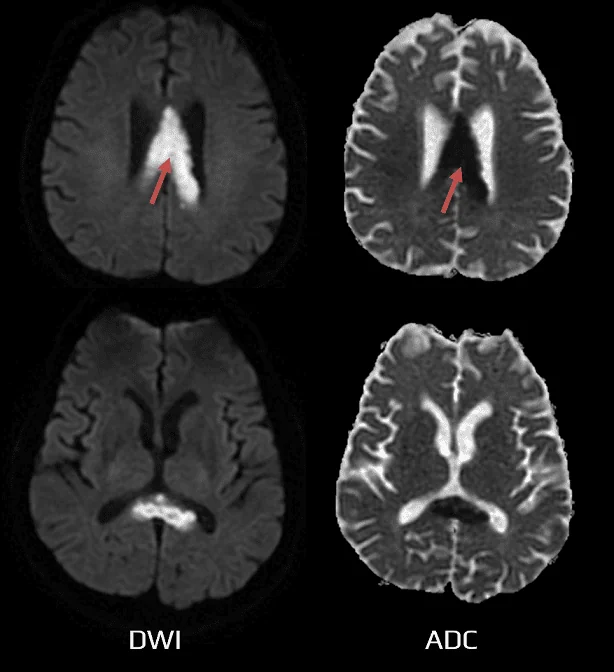
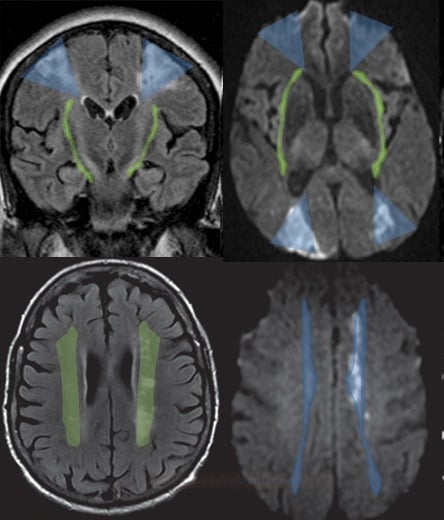
- Isolated Corpus Callosum Infarction (ICCI) is a rare disorder (rare due to the good vascular supply of the corpus callosum)
- varying in extent and location (Yang, 2014)
- genu x corpus x splenium (and combinations thereof) – depending on the location of ischemia, it can be determined whether the anterior or posterior circulation is affected
- uni- or bilateral
- symptoms are often nonspecific, sometimes resembling encephalopathy (DDx: tumor, infection)
- various etiologies (embolism, atherosclerosis, moyamoya, hyperviscosity syndrome)
-
pure sensory stroke (thalamic lesions)
-
pure hemiparesis (PMH) – most often located in the internal capsule, pons
- PMH with horizontal gaze palsy
- PMH with crossed oculomotor nerve palsy (Weber syndrome)
- PMH with crossed abducens nerve palsy (Millard-Gubler)
- PMH with confusion
- PMH with internuclear ophthalmoplegia (INO)
- pure face-saving hemiparesis (PMH)
- sensorimotor stroke (thalamocapsular) – internal capsule, thalamus
- dysarthria syndrome – clumsy hand
- atactic hemiparesis (pons)
-
hemiballism-hemichorea and acute dystonia (contralateral subthalamic and putaminal-pallidal regions and the posterolateral thalamus)
- cerebellar ataxia with crossed oculomotor palsy (Claude’s syndrome)
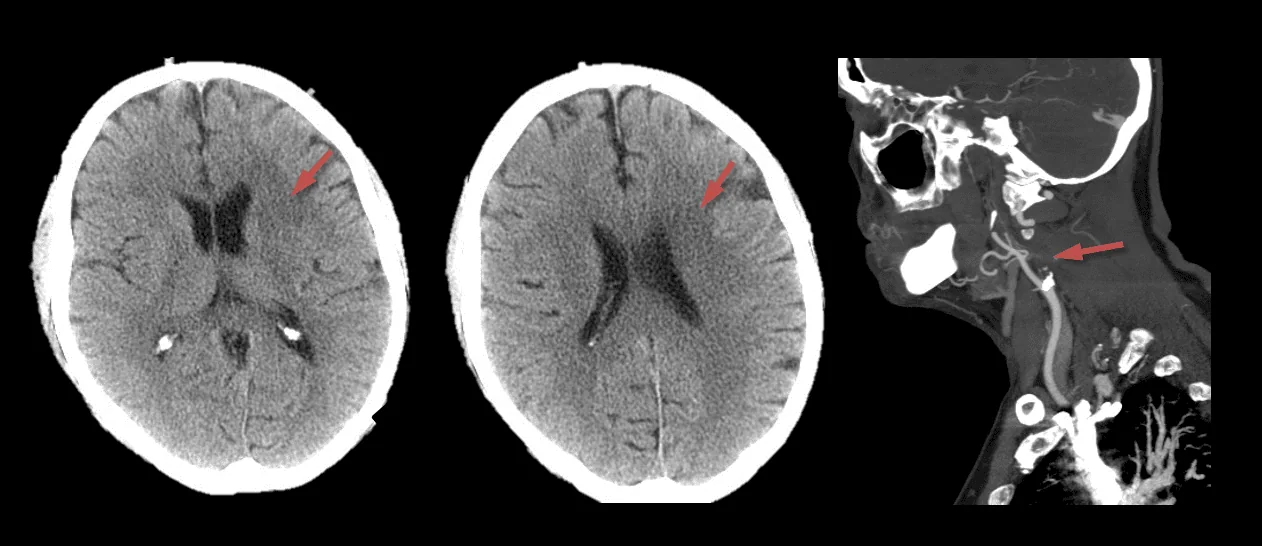
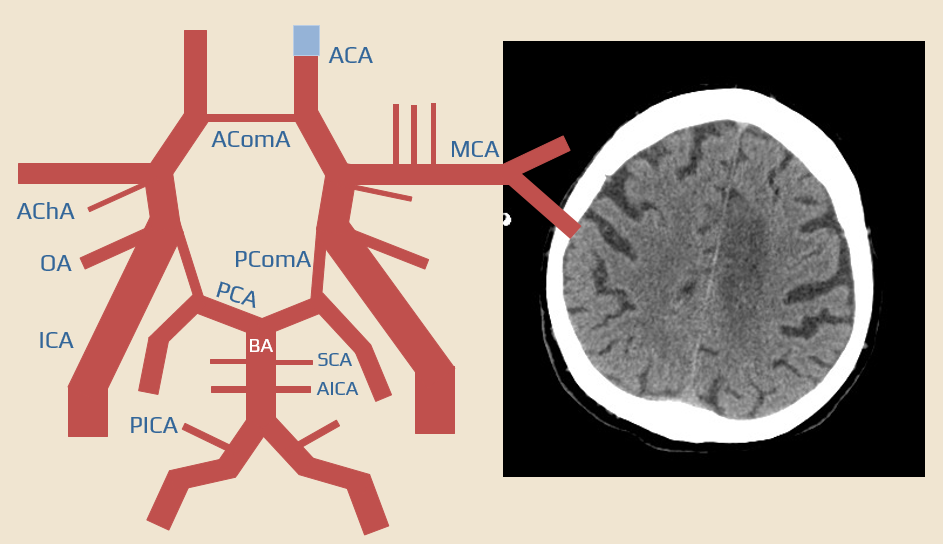
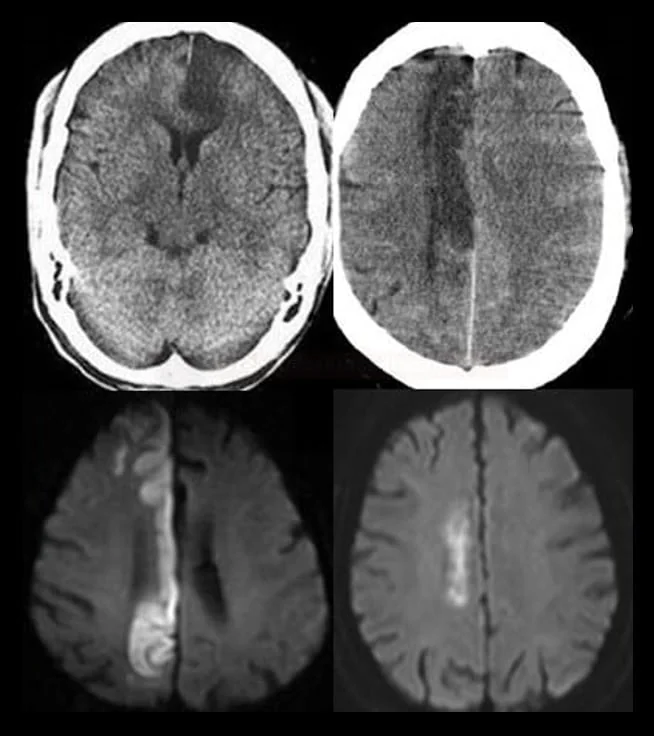
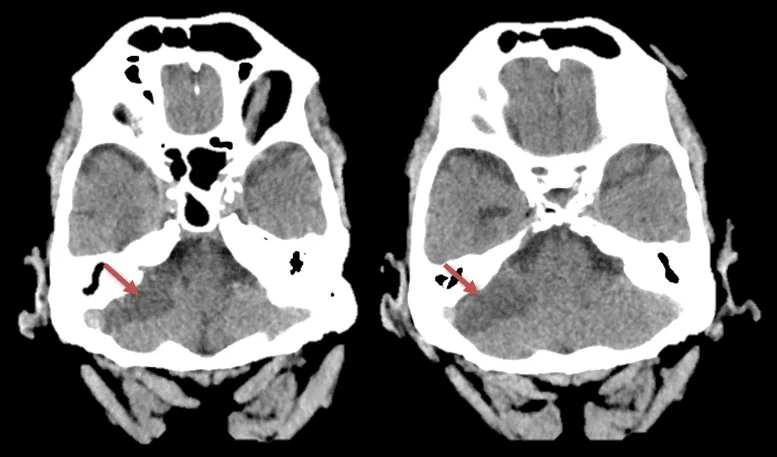
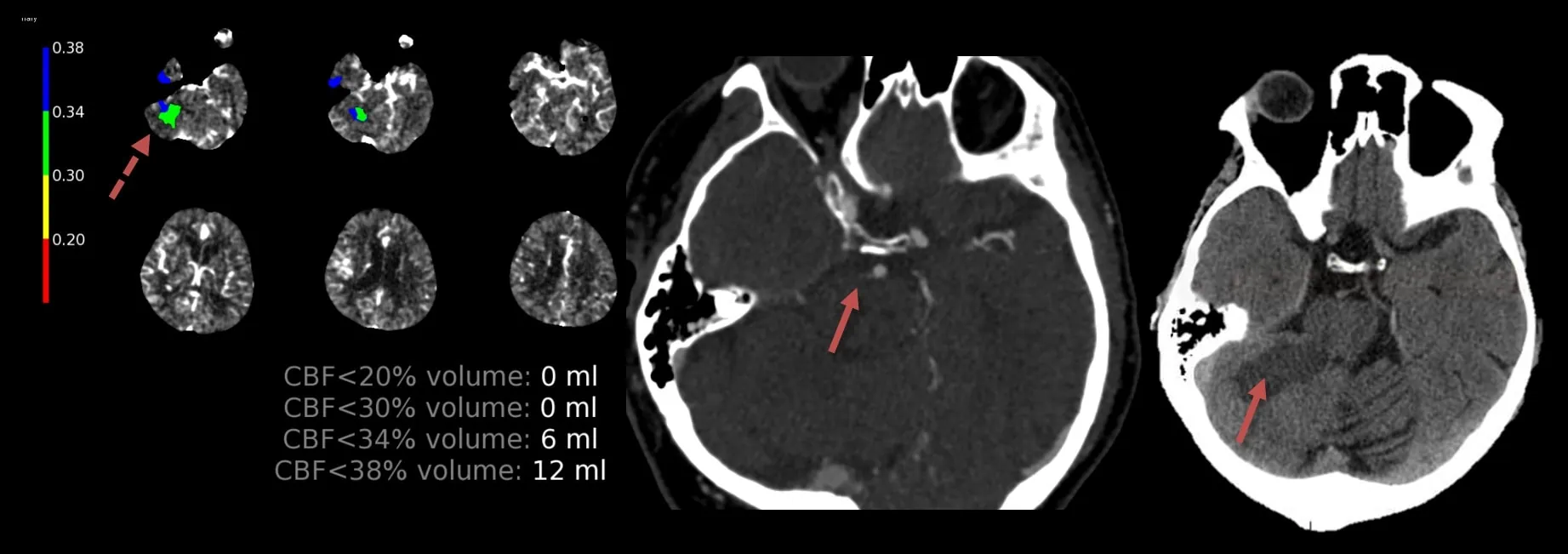
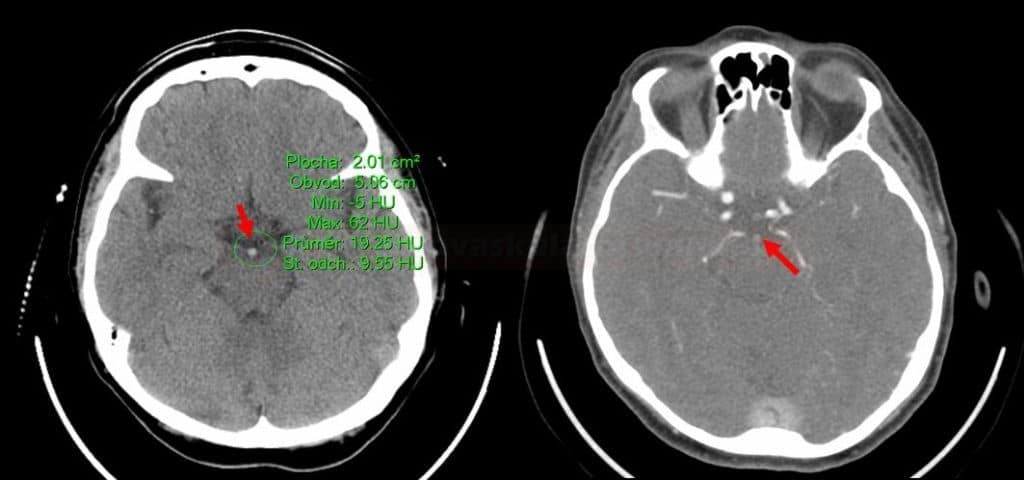
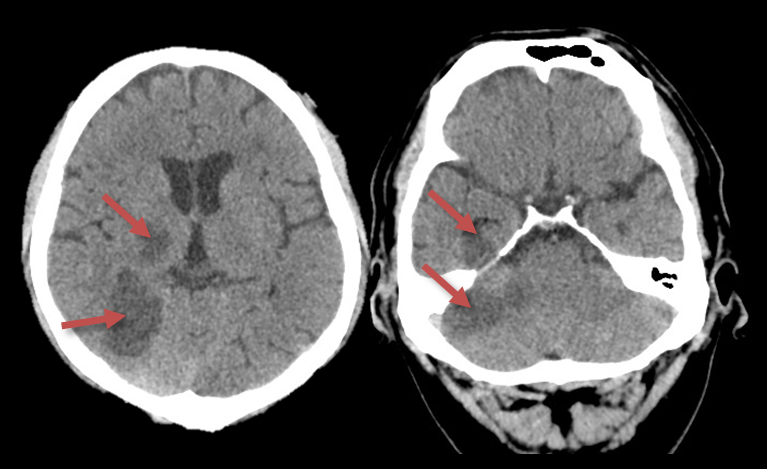
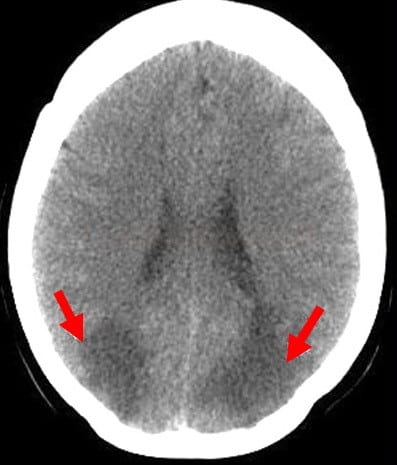
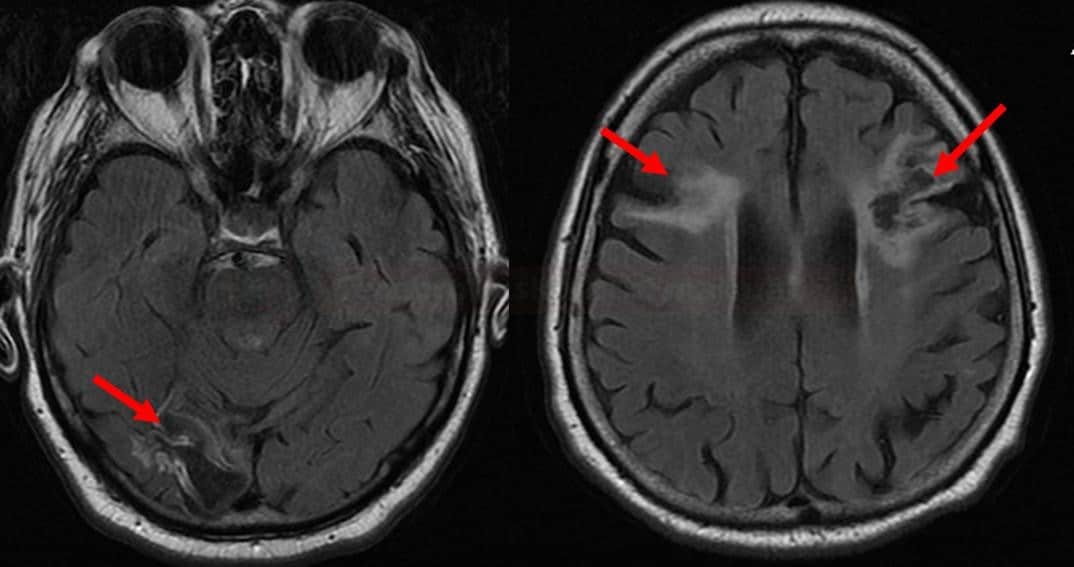
- BZI or watershed infarcts develop at the boundaries of cerebral arteries
- areas with permanently functional anastomoses (convexal pial arteries)
- areas where non-anastomosing terminal branches of different territories are adjacent (interface between deep perforating and pial arteries, for example, in the semiovale center)
- perfusion pressure in these areas gets most easily below the ischemic threshold (e.g., in significant ICA stenosis or during episodes of hypotension)
Significant stenosis/occlusion of the ICA
Cardiac failure
- cardiomyopathy
- myocarditis
- hypokinesis following myocardial infarction
Acute systemic hypotension (e.g., during surgery in ECC, during CPR, etc.)
- often, a combination of several factors is involved (artery stenosis + hypotension + microangiopathy)
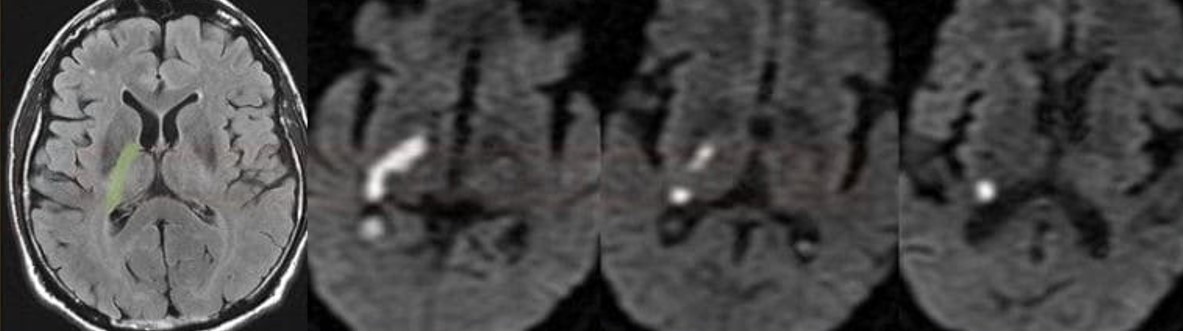
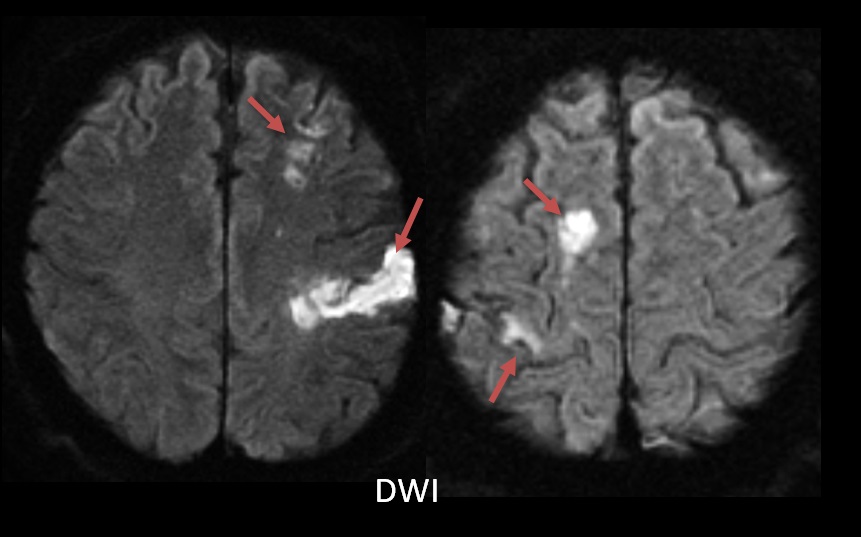
- embolic etiology of the current stroke cannot be definitively diagnosed by parenchymal imaging
- most embolic strokes present with a single lesion that is indistinguishable from other causes
- however, the presence of multiple lesions in different territories is suggestive of embolic etiology (especially if the lesions are of the same age)