Differential diagnosis of Visual impairment
David Goldemund M.D.
Updated on 02/04/2024, published on 23/02/2024
- the cornerstone of diagnosing visual impairment is the personal history, clinical examination (neurological and ophthalmological), and laboratory and imaging methods
- the nature and dynamics of the visual disturbance together with accompanying symptoms are essential for the topical-etiological diagnosis
Retinal disorders
- visual disturbance of retinal origin is usually painless with abnormal fundoscopic findings in the acute stage
- involvement of the inner layer of the retina (e.g., in the CRA occlusion) leads to similar visual field disturbances as lesions of the anterior optic nerve because this layer contains ganglion cells (causing most often altitudinal hemianopsia)
- monocular visual field defects occur in affected ipsilateral eye
- degenerative retinal lesions (e.g., retinitis pigmentosa) or glaucoma are characterized by concentric narrowing of the visual field or annular scotomas
Retinal artery occlusion
- etiology – embolism (thrombi, cholesterol, plaque fragments), vasospasms, migraine
- transient monocular vision loss (amaurosis fugax) → more here
- vascular occlusion can also lead to permanent vision loss → more here
- fundoscopic examination shows a normal finding on the disc, retinal pale edema, and cherry-red spot macula (choroidal perfusion is visible in the macula, surrounded by ganglion cells affected by infarction, which are absent in the macula)
Retinal vein occlusion
- subacute, for several hours developing monocular vision loss
- retinal hemorrhages, cotton wool spots, edema, and tortuous dilated retinal veins are present on fundoscopy
- there is usually a peripheral loss of vision; a decrease in visual acuity indicates concurrent macular involvement or ischemia of the optic nerve.
Glaucoma
- progressive retinal damage due to increased intraocular pressure. In the initial stages, the disease is asymptomatic, with scotomas appearing gradually
- diagnosis is made by measuring intraocular pressure, with regular measurements recommended from around the age of 40.
Optic nerve lesions
optic nerve Ischemic neuropathy
- sudden, painless loss of vision in one eye with reduced visual acuity, altitudinal visual field defect is common → see separate chapter
optic neuritis
- the most common cause of lesions of the optic nerve arising from an autoimmune process (typically MS)
- lesion of the maculopapular bundle with typical central/centrocecal scotoma
- optic nerve head may remain normal, be edematous, or atrophic during fundoscopic examination depending on the temporal profile of the lesion and the location of the lesion
- edema is present in inflammation affecting the intraocular segment of the nerve (papillitis) but not in a lesion behind the bulb (retrobulbar neuritis)
- atrophy is due to degeneration of retinal ganglion cell axons and develops > 4 weeks from the onset of the lesion.
Leber hereditary atrophy
- a hereditary disease caused by a mutation in the mitochondrial genome, maternally transmitted and with a 4:1 male preponderance
- characterised by loss of central vision; onset in the 2nd-3rd decade and acute onset simulating neuritis
- disability is bilateral, initially asymmetric
- the fundus in the acute stage resembles edema in papillitis (pseudoedema), but fluorescein angiography does not show any leakage of fluorescein outside the papilla
- in the chronic stage, it is difficult to differentiate it from other causes of optic atrophy
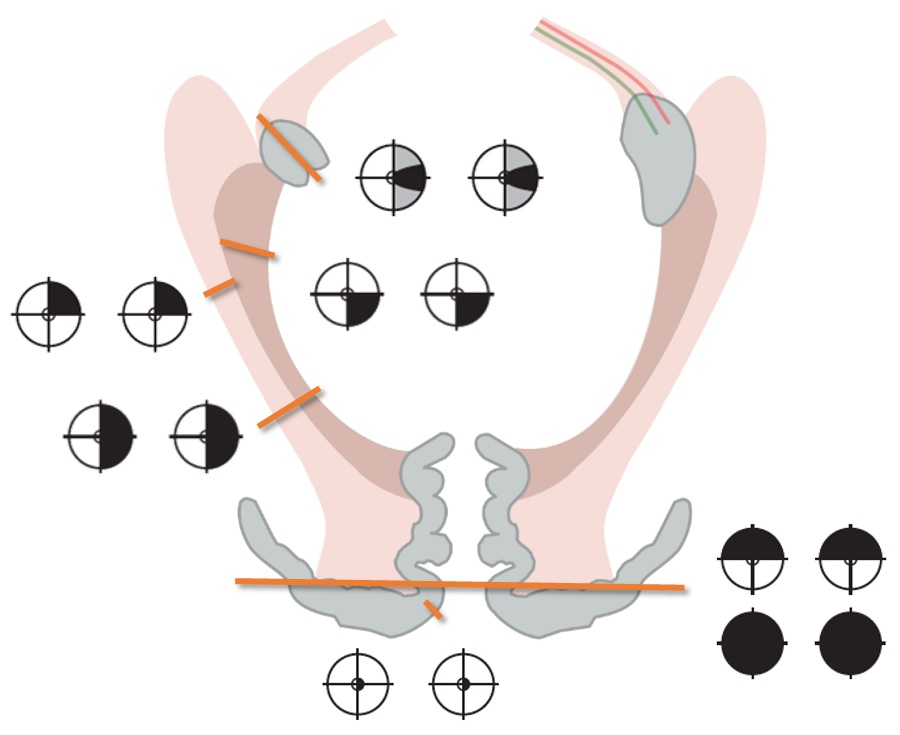
Optic chiasm lesions
- The clinical picture depends on the location and etiology of the lesion
- The most common is bitemporal hemianopsia
- Patients with slowly developing lesions often have no subjective visual complaints, and visual acuity impairment may not be apparent if the patient only reads the nasal half of the examination charts. Some patients complain of double vision due to non-corresponding nasal halves of the visual fields.
- Compression of the chiasm from below leads to a predominance of impairment in the upper parts of the temporal halves of the visual fields (upper bitemporal hemianopsia),
- Compression from above typically manifests as lower bitemporal hemianopsia
- Junctional scotoma – lesion of the anterior part of the chiasm
- Lesion of the nasal fibers before their crossing leads to an ipsilateral temporal defect (junctional scotoma according to Traquair)
- Lesion affecting the anterior part of the chiasm leads to an ipsilateral centrocecal scotoma and a defect in the upper temporal quadrant contralaterally (from the involvement of Willebrand’s knee of crossing fibers from the contralateral nasal retina
- Binasal hemianopsia
- External bilateral compression of the chiasm in cases of bilateral aneurysm of the internal carotid, hydrocephalus, or tumor of the skull base
- Eye diseases (glaucoma, optic nerve drusen, congenital hypoplasia of the optic nerve, sectoral retinitis pigmentosa)
- If the cause of the impairment is sellar expansion, prefixed chiasm, or dorsally located expansion, there is also involvement of the optic tract
Optic tract and lateral geniculate body lesions
- complete lesions of the optic tract and LGN lead to contralateral homonymous hemianopsia
- partial lesions lead to partial homonymous hemianopsia (defects are often non-congruent)
- there is a contralateral relative afferent pupillary defect (RAPD) and pallor of the optic disc temporally ipsilaterally
- etiology
- expansive sellar and parasellar processes (especially craniopharyngioma and aneurysm)
- demyelination
- ischemia
Optic radiation
- lesions of the optic radiation in the temporal lobe lead to contralateral superior homonymous quadrantanopia
- lesions of the radiation in the parietal lobe lead to contralateral inferior homonymous quadrantanopia
- in the case of a complete lesion of the optic radiation, contralateral homonymous hemianopsia is present
- pupillary reactions are preserved
- hemianopsia caused by lesions of the optic radiation are accompanied by additional associated hemispheric symptoms:
- lesions of the temporal lobe lead to memory disorders, Wernicke’s aphasia
- lesions of the dominant parietal lobe manifest as conduction aphasia, Gerstmann syndrome (finger agnosia, agraphia, acalculia, left-right disorientation) or tactile agnosia
- lesions of the non-dominant parietal lobe manifest as left-sided neglect syndrome, constructional apraxia, or dressing apraxia
- visual disturbances from lesions of the parieto-occipital junction or occipital lobe – Balint’s syndrome and cortical blindness
- deep parietal lesions can lead to homonymous hemianopsia and a disorder of tracking eye movements to the homolateral side
Occipital lobe
- unilateral lesions of the occipital lobe lead to contralateral homonymous congruent hemianopsia with typical central (macular) sparing
- the explanation for preserved central vision is twofold
- vascular supply of the occipital pole
- bilateral cortical representation of the macula
- hemianopsia caused by infarction of the occipital lobe due to vertebrobasilar thrombosis may be accompanied by brainstem and cerebellar symptoms
- the explanation for preserved central vision is twofold
- lesions limited to the area above or below the calcarine fissure lead to quadrantanopia
- bilateral lesions of the visual cortex above or below the calcarine fissure lead to altitudinal hemianopsias respecting the horizontal boundary
- cortical blindness results from bilateral lesions of the occipital lobe
Association areas
This content is restricted for paying subscribers



