31.01.2024
Colchicine May Benefit Patients With Diabetes and Recent MI
Microscopic Colitis Linked With Cardiovascular Risk
28.01.2024
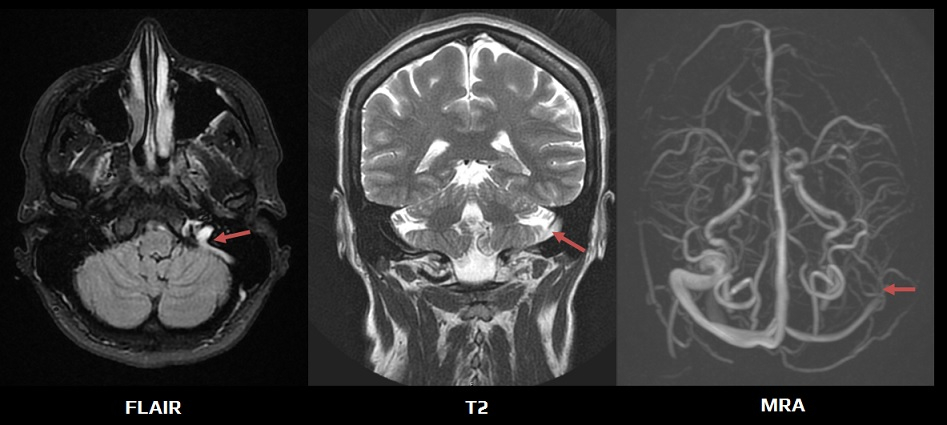
Diagnosis and Management of Cerebral Venous Thrombosis: A Scientific Statement From AHA
08.01.2024
Effect of the Factor XIa Inhibitor Asundexian According to Baseline Infarct Pattern and on MRI Covert Infarct Outcomes
04.01.2024
Window for Post-Stroke Antiplatelet Therapy Can Be Extended
Warfarin Benefits Patients After Surgical Aortic Valve Replacement
20.12.2023
Subhairline EEG: Potential for LVO Stroke Detection Unlocked
Catheter-Directed Strategy Improves Pulmonary Artery Occlusion
Time Window for Induced Hypertension in Acute Small Vessel Occlusive Stroke With Early Neurological Deterioration
Management of Poststroke Hyperglycemia: Results of the TEXAIS Randomized Clinical Trial
06.12.2023
Less Severe Strokes With LAA Closure vs DOAC in AF?
How Low Should You Go? Is Very Low LDL-C Safe?
Management of Poststroke Hyperglycemia: Results of the TEXAIS Randomized Clinical Trial
21.11.2023
Single Injection Reduces Blood Pressure for 6 Months: KARDIA-1
Asundexian Phase 3 AF Study Halted for Lack of Efficacy
More Evidence of Better Outcomes With 120 mm Hg BP Target
05.11.2023
Study of Rivaroxaban for Cerebral Venous Thrombosis: A Randomized Controlled Feasibility Trial Comparing Anticoagulation With Rivaroxaban to Standard-of-Care in Symptomatic Cerebral Venous Thrombosis
Transport Strategy in Patients With Suspected Acute Large Vessel Occlusion Stroke: TRIAGE-STROKE, a Randomized Clinical Trial
Effect of Individualized Versus Standardized Blood Pressure Management During Endovascular Stroke Treatment on Clinical Outcome: A Randomized Clinical Trial
22.10.2023
Tenecteplase Non-inferior to Alteplase in Stroke: ATTEST-2
12.10.2023
Primary findings of the TENSION trial
No Benefit of Enteric-Coated Aspirin vs Uncoated in CVD
Comparing Functional Outcomes and Safety Profiles of First-Line Aspiration Thrombectomy Versus Stentriever for Acute Basilar Artery Occlusion: Propensity Analysis of the PC-SEARCH Thrombectomy Registry
20.09.2023
Trial Halted for Bleeding Reduction With Abelacimab vs Rivaroxaban in AF
14.09.2023
Safety of Switching from a Vitamin K Antagonist to a Non-Vitamin K Antagonist Oral Anticoagulant in Frail Older Patients with Atrial Fibrillation: Results of the FRAIL-AF Randomized Controlled Trial
Intracerebral Hemorrhage Among Blood Donors and Their Transfusion Recipients
Medical Management Versus Endovascular Treatment for Large-Vessel Occlusion Anterior Circulation Stroke With Low NIHSS
03.09.2023
Statin Use in ICH Linked to Lower Risk for Subsequent Stroke
High Risk of Stroke in ANCA-associated Vasculitis
29.08.2023
Higher Mortality With Transfer to Endovascular Center in ICH
22.08.2023
COVID May Increase Risk of High Blood Pressure
Management of Inherited CNS Small Vessel Diseases: The CADASIL Example: A Scientific Statement From the AHA
15.08.2023
LAAO Tied to Fewer Post-Fall Bleeds Than DOACs in AF
Thrombectomy Improves Outcomes in Pediatric Stroke
03.08.2023
Low-Dose Aspirin and the Risk of Stroke and Intracerebral Bleeding in Healthy Older People. Secondary Analysis of a Randomized Clinical Trial
Medical Management Versus Endovascular Treatment for Large-Vessel Occlusion Anterior Circulation Stroke With Low NIHSS
Endovascular Therapy Versus Medical Treatment for Symptomatic Intracranial Artery Stenosis
23.06.2023
FDA OKs Low-Dose Colchicine for Broad CV Indication
Inflammatory Bowel Disease Tied to Increased Stroke Risk
12.06.2023
Immediate Statin After Acute Stroke Reduces Disability
Microscopic Colitis Raises Risk for Major Adverse Cardiovascular Events
01.06.2023
Tenecteplase Late After Stroke Misses Endpoint: TIMELESS
Intensive BP Reduction After Stroke Recanalization Harmful
30.05.2023
Cardiopathy No Basis for Choosing Anticoagulation in ESUS
No Added Benefit From Revascularization in Low-Risk CAS
25.05.2023
Earlier Anticoagulation Safe in Stroke With AF: ELAN
23.05.2023
Diffusion-Weighted Imaging Lesion Reversal in Older Patients With Stroke Treated With Mechanical Thrombectomy
19.05.2023
Clot Evacuation After ICH Tied to Better Outcome: ENRICH
Lipoprotein(a) Is Associated With the Progression and Vulnerability of New-Onset Carotid Atherosclerotic Plaque
23.4.2023
Infarcts in a New Territory: Insights From the ESCAPE-NA1 Trial
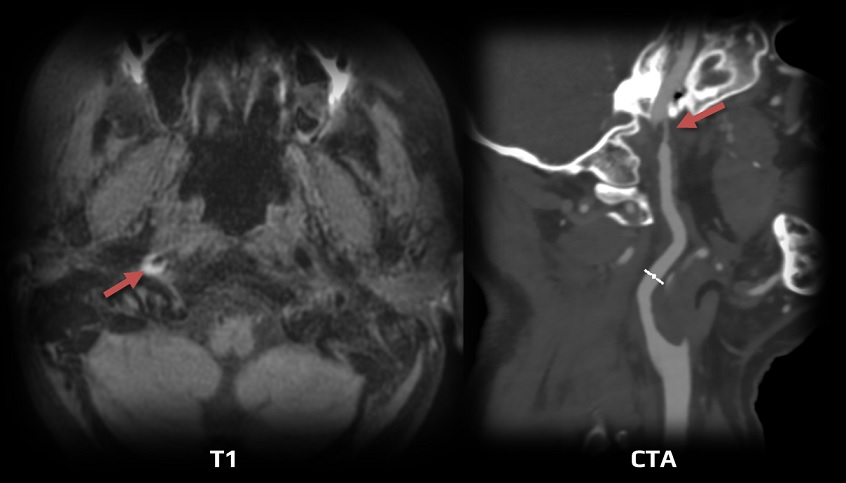
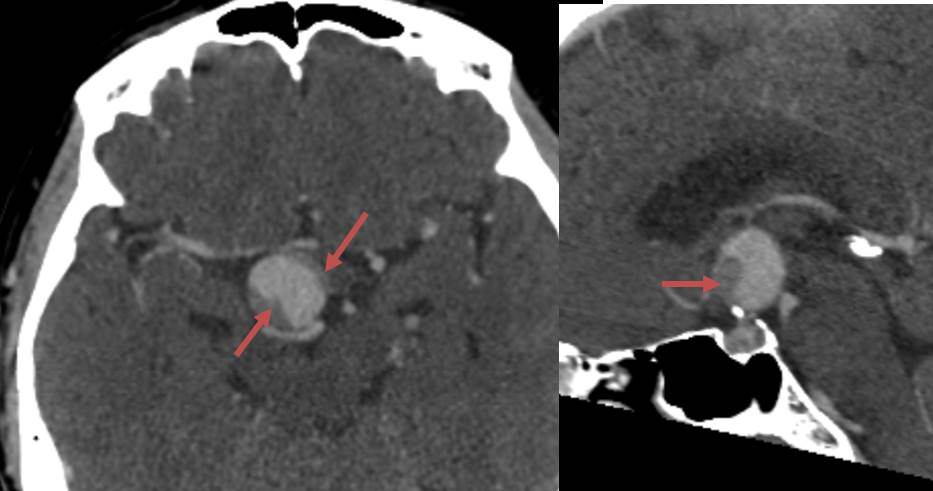
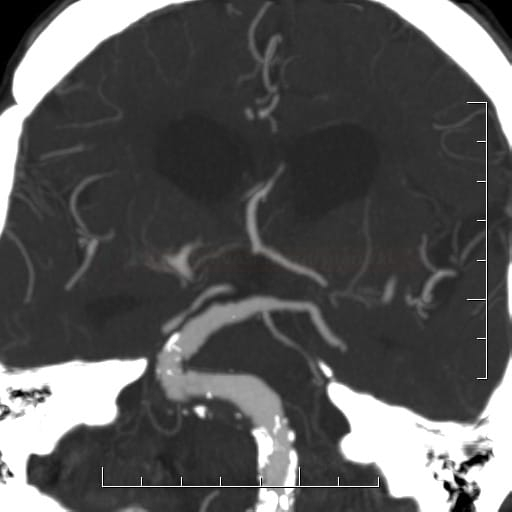
Bony Stroke: Ischemic Stroke Caused by Mechanical Stress on Brain Supplying Arteries From Anatomical Bone or Cartilage Anomalies
09.04.2023
High-Dose Prophylactic Anticoagulation Benefits Patients With COVID-19 Pneumonia
05.04.2023
US Doctor Groups Debate Best Use of New Weight Loss Drugs
Tenecteplase versus alteplase in acute ischaemic cerebrovascular events (TRACE-2): a phase 3, multicentre, open-label, randomised controlled, non-inferiority trial
Effect of Argatroban Plus Intravenous Alteplase vs Intravenous Alteplase Alone on Neurologic Function in Patients With Acute Ischemic StrokeThe ARAIS Randomized Clinical Trial
Lack of Statin Therapy and Outcomes After Ischemic Stroke: A Population-Based Study
Detection of Cardioembolic Sources With Nongated Cardiac Computed Tomography Angiography in Acute Stroke: Results From the ENCLOSE Study
03.04.2023
Complications of Intravenous Tenecteplase Versus Alteplase for the Treatment of Acute Ischemic Stroke: A Systematic Review and Meta-Analysis
23.03.2023
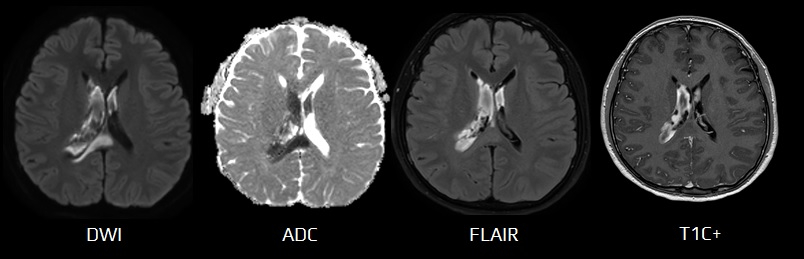
Deep Learning Algorithm Enables Cerebral Venous Thrombosis Detection With Routine Brain Magnetic Resonance Imaging
09.03.2023
Bempedoic Acid and Cardiovascular Outcomes in Statin-Intolerant Patients (CLEAR trial)
08.03.2023
Tirofiban Superior to Aspirin in Stroke Without Large Occlusion
Docs Struggle to Keep Up With the Flood of New Medical Knowledge. Here’s Advice
Early Stroke and Mortality After Percutaneous Left Atrial Appendage Occlusion in Patients With Atrial Fibrillation
Remote Diffusion-Weighted Imaging Lesions and Intracerebral Hemorrhage: A Systematic Review and Meta-Analysis
12.2.2023
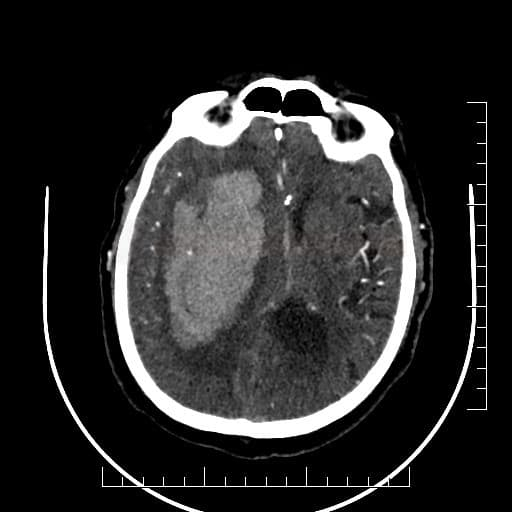
SELECT2 Trial of Endovascular Thrombectomy for Large Ischemic Strokes
ANGEL-ASPECTS Trial of Endovascular Therapy for Acute Ischemic Stroke with Large Infarct
Blood Pressure–Lowering After Thrombectomy May Be Harmful
10.2.2023
STROKE AF at 3 Years: High AF Rate After Atherosclerotic Stroke
08.02.2023
Disappointing Topline Results for Clazosentan in Aneurysmal SAH
Early Antiplatelet Resumption and the Risks of Major Bleeding After Intracerebral Hemorrhage
01.02.2023
Mechanical Thrombectomy Versus Best Medical Treatment in the Late Time Window in Non-DEFUSE-Non-DAWN Patients: A Multicenter Cohort Study0
CDC Still Looking at Potential Stroke Risk From Pfizer Bivalent COVID Shot
Acute therapy
2024- AHA – Treatment and Outcomes of Cervical Artery Dissection in Adults
2022 – ESO guidelines for an indication for intravenous thrombolysis before mechanical thrombectomy in patients with acute ischaemic stroke and anterior circulation large vessel occlusion
2022 – ESO guidelines for the management of menopause, pregnancy, and postpartum
2021 – ESO guidelines for the management of extra- and intracranial artery dissection
2021 – ESO guidelines on intravenous thrombolysis for acute ischaemic stroke
2021 – Management of Central Retinal Artery Occlusion
2019 – AHA/ASA Guidelines for the Early Management of Patients With Acute Ischemic Stroke: Update to the 2018 Guidelines
2019 – AHA/ASA – Management of Stroke in Neonates and Children
2019 – ESO-ESMINT Guidelines on Mechanical Thrombectomy in Acute Ischemic Stroke
2018 – Guidelines for the Early Management of Patients With Acute Ischemic Stroke
2016 – Scientific Rationale for the Inclusion and Exclusion Criteria for Intravenous Alteplase in Acute Ischemic Stroke
Prevention
2021 – Guideline for the Prevention of Stroke in Patients With Stroke and TIA (AHA/ASA)
2017 – Prevention of Stroke in Patients With Silent Cerebrovascular Disease
2014 – Guidelines for the Primary Stroke Prevention (AHA/ASA)
2014 – Guidelines for the Prevention of Stroke in Women (AHA/ASA)
2011 – Guideline on the Management of Patients With Extracranial Carotid and Vertebral Artery Disease
2009 – Definition and Evaluation of Transient Ischemic Attack (AHA/ASA)
Antithrombotic therapy
PFO, LAA
Others
antithrombotic drugs - hypolipidemic drugs - antihypertensive drugs - endarterectomy - angioplasty and stenting - PFO and LAA occlusion
intravenous and intraarterial thrombolysis
mechanical recanalization
acute angioplasty and endarterectomy
INTRACEREBRALHEMORRHAGE
diagnostic evaluation
etiology
therapy and prevention
diagnostic evaluation
etiology
management
diagnostic evaluation
etiology
therapy
asymptomatic aneurysm management
CT + CT angiography / perfusion
MRI + MR angiography / perfusion
DSA
neurosonology
TTE + TEE
ECG monitoring

